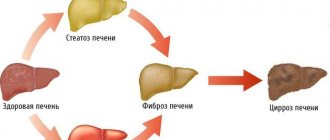
Non-drug therapy Drug therapy Advantages of a combination of phospholipids with glycyrrhizic acid Today, one of the primary tasks of hepatology is to provide medical care to patients with liver dysfunction of alcoholic, non-alcoholic, medicinal and toxic origin. The high medical and social significance of this problem is associated with the need for adequate treatment, which requires the use of drugs of various pharmacological groups and non-drug methods. Experts recommend the use of hepatoprotectors as pathogenetic therapy agents that have a positive effect on the structure and function of hepatocytes and increase their resistance to pathogenic factors. Essential phospholipids are among the most studied and safe drugs in this group.
What are phospholipids?
In biological terminology, phospholipids are complex lipids containing fatty acids, phosphoric acid and functional groups, including nitrogen. These compounds are the main building material of cell membranes. They also stimulate enzyme activity and take part in cell differentiation, division and regeneration.
Phospholipids in the structure of the liver
High-energy molecules of endogenous phospholipids are biologically active substances necessary for the normal functioning of the liver. Being integrated into the membranes and organelles of liver cells, they prevent compaction of the structure of fatty acids and regulate the metabolism of lipoproteins. At the same time, these compounds increase the concentration of glutathione, suppress oxidative stress, and reduce the production of hydrogen peroxide. Thanks to the effect of phospholipids on the liver, the amount of damage at the cellular level is significantly reduced. Taking into account the above, the main functions of phospholipids can be distinguished:
- structural,
- protective,
- regulatory,
- hepatoprotective.
The leading pathogenetic mechanism of cell damage is cross-oxidation. Phospholipids suppress this process, which makes them vital components necessary for the normal functioning of the organ.
The place of phospholipids in the treatment of various liver diseases (ALD, NAFLD, LLD)
Today, one of the most pressing problems of modern medicine is liver pathologies caused by various agents. This group of diseases includes ALD (alcoholic liver disease), NAFLD (non-alcoholic fatty liver disease), and LLD (drug-induced liver disease). For the treatment and prevention of these pathologies, drugs of various pharmacological groups are used. A special place among them is occupied by drugs with hepatoprotective properties. Hepatoprotectors include essential (irreplaceable) phospholipids.
Hepatoprotectors (HP) are a group of drugs that prevent damage to the hepatocyte and restore damage to the structure and function of the hepatocyte or the hepatobiliary system as a whole [1, 16, 21]. Data on the clinical effectiveness of GP in various forms of liver damage are characterized by inconsistency due to the small number of large-scale multicenter randomized placebo-controlled studies conducted [16, 28], and disappointing data from a meta-analysis of studies [33, 36, 37].
Nevertheless, the complexity of etiotropic therapy for liver diseases makes the group of GPs extremely promising drugs, since the main direction of their action is to influence pathogenetic mechanisms and slow down or reduce the pathological process in the liver [16].
The main requirements for an ideal GP were formulated by R. Preisig [35]: fairly complete absorption; the presence of a “first pass” effect through the liver; pronounced ability to bind or prevent the formation of highly active damaging compounds; the ability to reduce excessive inflammation; suppression of fibrogenesis; stimulation of liver regeneration; natural metabolism in liver pathology; extensive enterohepatic circulation; no toxicity.
Despite the fact that none of the drugs to date fully meets these requirements [18], GPs account for 9.2% of the total number of drugs used in the treatment of liver diseases [7]. At the same time, there are no exact data on the mechanism of action of GP, and therefore the choice of drug in each specific situation is difficult. The classification of GPs could help to adequately select a drug, but there is no unified classification of drugs in this group, which further complicates the choice of a liver protector for a particular liver disease [16].
S.V. Morozov and Yu.A. Kucheryavyi [16] presented the most used classification of HP, based on different classification criteria and not very suitable for such a choice: herbal preparations; preparations of animal origin; essential phospholipids; amino acids and their derivatives; vitamins, antioxidants and vitamin-like preparations; other drugs.
Of greater practical importance is the classification proposed by S.V. Okovitym [18], dividing GPs by origin and mechanism of action: 1. Preparations of plant origin: 1) containing milk thistle flavonoids: hepabene, legalon, karsil, hepatofalk-planta, silybor; 2) containing flavonoids of other plants: hophytol, katergen (cyanidanol), LIV-52 (hepaliv).
2. Preparations of animal origin: sirepar, laennec. 3. Preparations containing essential phospholipids: Essentiale, Livolin Forte, Phosphogliv, Essliver, Eplir). 4. Preparations with a predominantly detoxifying effect: 1) with a predominantly direct detoxifying effect; 2) reducing the formation of endogenous toxins; 3) activating the formation of endogenous detoxicants; 4) accelerating the metabolism of toxins (methadoxyl). 5. Drugs of different groups.
Thus, the current classifications of HP are not very convenient for practical use, and the task of clinicians is to propose a classification that would help choose the drug that is optimal for a specific clinical situation. Below is a brief description of individual groups of SOEs.
Essential phospholipids (EPL)
All cell membranes consist of ⅔ phospholipids, and mitochondrial membranes consist of 92% [1, 21]. From this it is clear that EPL have a cytoprotective effect and are involved in maintaining normal membrane fluidity and repair [1, 7, 21]. The mechanisms of action of EPL also include the antioxidant effect [21, 27]; protection of mitochondria and microsomal enzymes from damage; slowing down collagen synthesis and increasing collagenase activity; inhibition of transformation of Ito cells into collagen-producing ones (antifibrotic effect) [7, 16, 21, 30]; a decrease in the activity of cytochrome P450 2E1, which leads to the reverse development of fatty degeneration [7].
According to C. Lieber [30], drinking alcohol in combination with EPL prevented the development of fibrosis and cirrhosis in baboons, while baboons that did not receive EPL along with alcohol demonstrated alcoholic liver disease from steatohepatitis to cirrhosis. Moreover, in a study on rats it was shown [27] that administration of an EPL mixture to animals with alcoholic liver disease normalizes not only indicators of oxidative stress and the level of hepatic glutathione, but also the level of hepatic S-adenosyl-methionine.
The authors of this publication have their own experience in the treatment of EPL using the drug livoline forte in patients with alcoholic and non-alcoholic fatty liver disease in the stage of steatohepatitis. The composition of Livoline forte includes lecithin - 857.13 mg, containing EPL - 300 mg, vitamin B1 - 10 mg, vitamin B2 - 6 mg, vitamin B6 - 10 mg, vitamin B12 - 10 mcg, nicotinamide - 30 mg, vitamin E - 10 mg. Treatment was carried out for 1 month, the daily dose of the drug was 2 capsules 3 times a day. Taking the drug for 1 month led to normalization of biochemical parameters (cytolysis and cholestasis, the initial levels of which were 2 times higher than normal). The drug was well tolerated, no adverse reactions were recorded. This allowed us to assume that the use of livolin forte will also lead to a decrease in the degree of liver fibrosis, the dynamics of which we assessed using the fibrosis index (IF).
The “gold standard” for diagnosing the degree of fibrosis is a puncture biopsy of the liver, but this method has many limitations in practical use. This was the basis for the use of non-invasive methods for assessing fibrosis, in particular by calculating the IF according to the Bonacinni scale. Our own data obtained by comparing the results of liver puncture biopsy and IF showed the high sensitivity of the latter [9, 10]. The simplicity and accessibility of obtaining IF make it possible to widely use it to evaluate the results of treatment of patients with diffuse liver diseases in the stage of fibrosis (cirrhosis).
We assessed the antifibrotic effect of the drug livoline forte in patients with non-alcoholic steatohepatitis. The study included patients with obesity, type 2 diabetes, mixed steatohepatitis; the level of increase in cytolysis enzymes exceeded the norm by 2 times, cholestasis - more than 2 times; The FI was 3.4±1.1 points. Patients received livoline forte 2 capsules 3 times a day for 6 months; control of biochemical analysis and calculation of IF were carried out every 3 months. Indicators of cytolysis and cholestasis normalized during the first 3 months of treatment (see table)
.
As can be seen from the presented data, initially the studied patients had elevated levels of cholesterol, triglycerides, transaminases, and gamma-glutamate transferase (gamma-GT). 4 patients had type 2 diabetes mellitus with elevated fasting glucose levels. Over 3 months of therapy with Livolin Forte, a tendency towards a decrease in transaminases, gamma-GT, and alkaline phosphatase was noted. By the 6th month of treatment, a significant decrease in AST and gamma-GT was revealed.
The FI in the study group, assessed using the discriminant scoring scale (Bonacinni), before treatment was 3.4±1.1 points; after 3 months of treatment, a significant decrease to 2.5±0.7 points was observed. After 6 months, the IF remained at the same level - 2.5±0.8 points (differences compared with the initial level are significant, p
<0,05).
Clinically, non-alcoholic steatohepatitis was manifested by the presence of heaviness after eating (40% of cases), discomfort in the right hypochondrium (30%), weakness (30%). It should be noted that the intensity of the symptoms was low. Basically, the disease was characterized by an asymptomatic or low-symptomatic course. Some patients had dyspeptic symptoms (a feeling of bitterness in the mouth, nausea, loss of appetite).
Thus, the studies have shown the effectiveness of livolin forte in the treatment of patients with alcoholic and non-alcoholic steatohepatitis (by normalizing cytolysis and cholestasis). The study of liver fibrosis (according to IF) showed positive dynamics after 3 months of treatment and maintenance of the achieved effect by the 6th month of therapy. Livolin forte demonstrated protective properties both in normalizing hepatocyte metabolism and in antifibrotic effect. There were no undesirable side effects during long-term treatment (6 months) in the study.
A large group of patients consists of patients with drug-induced liver damage, which begins with damage to the cell membrane. In these cases, livoline forte is the drug of choice with which therapy is started and continued until the structural and functional activity of the organ is restored.
Amino acids and their derivatives
Heptral - S-ademetionine - a coenzyme that takes part in the processes of transmethylation (synthesis of phospholipids), transsulfation (participation in the synthesis of glutathione, cysteine, taurine, coenzyme A) [2, 10]; synthesis of polyamines (proliferation of hepatocytes and liver regeneration) [2, 9]. Thus, S-ademetionine has an antioxidant, detoxifying, cytoprotective, regenerative effect, in the clinical aspect eliminates the manifestations of cholestasis [7, 20, 21, 29], has an antidepressant, antifibrotic [3, 18, 21] and anti-neurotoxic effect [18] .
Clinical trials of Heptral began in 1990. In patients with liver pathology, long-term treatment with Heptral was accompanied by an improvement in the biochemical parameters of the liver. The drug has also demonstrated effectiveness when prescribed to women with intrahepatic cholestasis during pregnancy; in patients with depression, chronic and acute pancreatitis, where it has been used to reduce oxidative stress.
The authors of this work used Heptral in 60 patients with chronic liver diseases and cholestasis syndrome [11]. In patients with insufficient effect or resistant to treatment, a dose of 3200 mg per day was used. The effect of heptral within 4 weeks of treatment was noted in the majority of patients, primarily with alcoholic liver damage, both in clinical and laboratory parameters. Almost all patients who received prolonged therapy subsequently showed positive dynamics in laboratory parameters and normalization of clinical manifestations.
Flavonoids
Silibinin is a preparation from the fruits of milk thistle [7]. Silibinin interacts with free radicals, providing an antioxidant effect; specifically stimulates RNA polymerase A, promoting the synthesis of structural and functional proteins and phospholipids; stabilizes cell membranes and restores their permeability [7, 18]; prevents the penetration of certain hepatotoxic substances (poisons of the toadstool) into the cell [18, 21]; slows down the rate of fibrosis formation in the liver (in experimental studies [21]).
The high prevalence of viral hepatitis in recent years has forced us to look for new ways to treat this pathology, one of which was the study of new properties of long-known drugs. Thus, in 2010, data were published in the journal “Gastroenterology” [26] proving the ability of silibinin and similar substances to inhibit the RNA-dependent polymerase of the hepatitis C virus, as well as to have an inhibitory effect on the replication of the hepatitis C virus lb and on the hepatitis C virus transcription factor C 2a. Further studies revealed the ability of silibinin to inhibit the proliferation and proinflammatory activity of T cells during HCV infection [32]. These studies showed promise for the use of milk thistle in the treatment of viral hepatitis C.
In their own study [8], the authors assessed the effectiveness of the complex drug Sibektan in patients with chronic viral hepatitis of various etiologies. The study group included 30 patients with chronic hepatitis C (26), B (2) and G (2), who received sibektan at a dose of 2 tablets 4 times a day for 30-40 days. A significant decrease in transaminase levels was noted in patients with mild and moderately severe disease activity, which made it possible to recommend Sibektan primarily for this category of patients.
Ursodeoxycholic acid (UDCA) preparations
UDCA is a hydrophilic non-toxic tertiary bile acid [12, 16]. Its content in the natural pool of human bile acids is 4%. Taking UDCA leads to a slowdown in the enterohepatic circulation of hydrophobic bile acids, which have a hepatotoxic effect, thereby preventing their toxic effect on the membranes of hepatocytes and the epithelium of the bile ducts [16].
The effectiveness of ursotherapy is associated with the currently known mechanisms of action of UDCA [4, 12, 16]: 1) choleretic effect: displacement of the pool of toxic bile acids due to competitive capture of receptors in the ileum; 2) cytoprotective effect: UDCA is integrated into the cell membrane of the hepatocyte, which becomes more resistant to the damaging effects of toxic agents; 3) antifibrotic effect: the drug regulates the stimulation of stellate cell function associated with the absorption of apoptotic bodies, slows down fibrogenesis; 4) immunomodulatory effect: UDCA reduces the expression of HLA-I class molecules on hepatocytes and HLA-II class molecules on cholangiocytes, reduces the production of pro-inflammatory cytokines (IL-1,2,6, TNF, IFN); 5) antioxidant effect: blocks the release of free radicals, suppresses the processes of lipid peroxidation; 6) anti-apoptotic effect; 7) hypocholesterolemic effect; litholytic effect.
2) cytoprotective effect: UDCA is integrated into the cell membrane of the hepatocyte, which becomes more resistant to the damaging effects of toxic agents; 3) antifibrotic effect: the drug regulates the stimulation of stellate cell function associated with the absorption of apoptotic bodies, slows down fibrogenesis; 4) immunomodulatory effect: UDCA reduces the expression of HLA-I class molecules on hepatocytes and HLA-II class molecules on cholangiocytes, reduces the production of pro-inflammatory cytokines (IL-1,2,6, TNF, IFN); 5) antioxidant effect: blocks the release of free radicals, suppresses the processes of lipid peroxidation; 6) anti-apoptotic effect; 7) hypocholesterolemic effect; litholytic effect.
The authors of this work administered ursosan therapy at a dose of 12.5-l5.0 mg/kg for 6 months to 45 patients with chronic alcoholic steatohepatitis. During therapy, the following were recorded: relief of clinical and biochemical manifestations of the disease, a significant decrease in fatty infiltration of the liver according to ultrasound, and a decrease in IF [13].
Metadoxyl
Metadoxyl is a compound of pyridoxine and pyrrolidine carboxylate. It has been shown [2, 5] that metadoxine, by increasing the activity of alcohol dehydrogenase and acetal dehydrogenase, accelerates the removal of ethanol and its under-oxidized metabolites from the liver from the plasma, reducing the period of their toxic effects on the liver and other tissues. Experiments demonstrated pronounced antioxidant activity of the drug (increased ATP concentration in the liver and restoration of glutathione content) [24]. In addition, it was experimentally proven [17] that metadoxine has important antinecrotic and antifibrotic properties that are not associated with either its described effect on alcohol metabolism or antioxidant activity. It was found that metadoxine reduces the synthesis of precursors of fibrous structures (fibronectin and procollagen), and also reduces the activity of the enzyme proline hydroxylase, which promotes the conversion of soluble procollagen into collagen [2]. The drug also has a direct cholinergic effect on the central nervous system, activates the cholinergic and GABAergic systems, thus increasing the concentration of GABA and acetylcholine in the synaptic space. This is accompanied by antidepressant and psychostimulating effects [19].
Polyprenols
In the last few years, interest in natural low-molecular bioregulators—polyisoprenoids and their derivatives—has increased in medicine and biochemistry. Currently, new ways of synthesizing and obtaining these substances from plant substrates as having high physiological activity and low toxicity are being developed. Growing interest in natural bioregulators polyprenols has led to the creation of the drug ropren, which is a mixture of homologues of polyprenols obtained from pine needles ( Pinus silvestris
) and spruce (
Picea albies
). The polyprenols included in the drug are metabolized in the body to form dolichol, which takes part in the glycosylation of proteins. The pharmacological action of polyprenols is based mainly on their replacement effect. It has been established that in chronic inflammatory-degenerative liver diseases, dolichol deficiency and insufficiency of the dolichol phosphate cycle occur, which leads to disruption of glycoprotein synthesis [14]. Since glycoproteins carry out intercellular and cell-matrix interactions, play the role of signaling molecules, are part of mucus, collagen, immunoglobulins, plasma proteins, enzymes, receptors, some hormones and growth factors [6], it is difficult to overestimate the role of replenishing the deficiency of polyprenols.
The discovery of exogenous homologues of polyprenols in lipids obtained from liver homogenate in the form of functionally active molecules indicates the cytoprotective effect of exogenous polyprenols, which is due both to the direct location of dolichol in the lipid bilayer of membranes and to the participation in the glycosylation of membrane class proteins [22, 23, 25, 34, 39].
Experimental and clinical trials have shown the hepatoprotective, antioxidant, immunomodulatory, anti-inflammatory, antifibrotic, and neuroprotective effects of the drug Ropren [22, 23, 25, 38, 39].
The authors [15] studied the drug Ropren in 30 patients with alcoholic cirrhosis of the liver. There was a significant improvement in biochemical parameters, a decrease in the degree of fibrosis, the severity of encephalopathy and neuropathy on the Young scale, and a significant increase in indicators of the quality of life of patients during treatment with ropren.
Other promising directions
One of the promising areas is the use of complex homeopathic preparations containing small doses of substances of plant, mineral and animal origin. Thus, toxic and allergic effects on the human body during long-term therapeutic courses are primarily excluded [7].
Promising drugs may be those GPs that, in addition to the hepatoprotective effect, have an effect on other organs and systems. Thus, the antidepressant effect of drugs containing S-adenosylmethionine [3] and metadoxine [19] is known. The data obtained by the authors [15] when studying the drug Ropren showed both its central neurotropic effect and its effect on peripheral neuroprotection.
The data presented show that the success of hepatoprotective therapy depends primarily on the correct choice of GP for a particular nosological form, as well as on the mechanism of pathogenesis of liver pathology in a particular patient. Our own experience of using liver protectors allows us to propose a classification of GPs for consideration depending on the predominant mechanism of their action.
1. Drugs with a predominant effect on cytolysis syndrome, reducing fatty infiltration of the liver: Livoline Forte, Essentiale Forte, Essliver, Phosphogliv.
2. Drugs with a predominant effect on cholestasis syndrome:
a) UDCA preparations: ursosan, ursofalk, etc.;
b) preparations containing S-adenosylmethionine: heptral.
3. Preparations with a predominantly detoxifying effect:
a) used for acute and chronic alcohol intoxication: metadoxyl;
b) used for drug and other toxic injuries:
1) containing milk thistle flavonoids: hepabene, legalon, karsil;
2) containing flavonoids of other plants: hophytol.
4. Drugs with a presumed antifibrotic effect, recommended for use at the stage of liver cirrhosis:
a) preparations containing milk thistle flavonoids: karsil;
b) drugs from the polyprenols group: ropren;
c) UDCA preparations.
5. GPs with supposed antiviral activity (inhibiting the replication of the hepatitis C virus - preparations containing milk thistle flavonoids: silibinin, silymarin (experimental data) [26, 32].
6. Drugs that restore the biological cycle of cells and modulate the immune system: Laennec.
7. Drugs with a combined hepato- and neurotropic effect, acting on the central and peripheral nervous system: metadoxil, ropren.
We hope that the chosen classification principle will help the practitioner choose an adequate GP, and the classification itself will be the basis for its improvement.
What phospholipids can help with liver diseases
Not all, but only certain plant phospholipids, completely purified from foreign impurities, are used as medicines. They contain polyunsaturated higher fatty acids, which neutralize free radicals and counteract cross-oxidation processes, which determines the therapeutic properties of hepatoprotectors. These drugs, which help restore the integrity of cell membranes, eliminate the consequences, but not the causes of the development of pathological processes, therefore, in the treatment of liver diseases, they are used in combination with other drugs.
Benefits of combining phospholipids with glycyrrhizic acid
Hepatoprotectors, containing complex lipids of plant origin, are today one of the most popular groups of drugs used for liver diseases. However, phospholipids themselves cannot eliminate the inflammatory process, which in most cases is the cause of the development of one or another pathology. Through numerous studies and experiments, pharmaceutical scientists were able to identify a combination of substances that can protect liver cells from damage and at the same time reduce inflammation. Essential phospholipids and glycyrrhizic acid together represent a compound with antioxidant, anti-inflammatory and antifibrotic activity. The components in this combination have a therapeutic effect for hepatosis, alcoholic and toxic lesions, as well as for acute and chronic hepatitis, psoriasis, etc.
Indications for Essentiale
- chronic hepatitis; cirrhosis of the liver; fatty liver of various etiologies; toxic liver damage; alcoholic hepatitis; liver dysfunction in other somatic diseases;
- toxicosis of pregnancy;
- prevention of recurrence of gallstone formation;
- psoriasis (as an adjuvant therapy);
- radiation syndrome.
Treatment regimens
Take capsules orally with plenty of water.
The drug is suitable for use in adolescents over 12 years of age and adults. The recommended dosage is 2 capsules. 3 times a day with meals.
There are no restrictions on the duration of treatment from the manufacturer, but depending on the severity of the disease, it is important to consult with a specialist. Maintenance therapy on a regular basis is possible only if there are clear signs of improvement. In other cases, the advisability of taking the medicine or replacing it is determined by a specialist.
According to consumer reviews, a positive effect occurs in a short time (for mild ailments); for severe or complex forms of the disease, in order to achieve a lasting effect, you need to drink a minimum course of a month. Perhaps as part of complex therapy.
Contraindications
One of the main contraindications is a tendency to allergic reactions. The fact is that Essentiale capsules contain soybean oil in the shell, which can provoke severe allergic reactions in people prone to such. Otherwise, the drug is well tolerated, with the exception of individual reactions of the body to the components of the composition.
Phosphogliv* – a comprehensive approach to liver restoration
When treating liver diseases, experts recommend using Phosphogliv* as a drug that protects hepatocytes from the effects of various pathological factors and accelerates their regeneration. The combined agent has membrane-stabilizing, antioxidant, anti-inflammatory and antifibrotic effects. Phosphogliv* restores the structure of membranes, accelerates regenerative processes, normalizes organ functions, reduces the risk of developing fibrosis, cirrhosis of the liver and other diseases. The use of this drug in combination with other medications significantly improves the biochemical parameters of the blood and the general well-being of patients.
Special Recommendations
Essentiale and alcohol
Since alcohol has a well-known toxic effect on the body and liver cells, the use of Essentiale and alcohol intake become incompatible concepts. In addition, one should not assume that the drug is capable of providing a supportive and protective effect on the liver while taking alcohol-containing products. During treatment with Essentiale, it is recommended to refrain from drinking alcohol.
Essentiale and diet
Compliance with a strictly mandatory diet during the course of Essentiale is not a strict obligation, but only a recommendation. Any disease of the digestive organs and glands requires dietary nutrition. Because diet is the basis for a positive outcome in such diseases. During the acute period of the disease, the liver is especially vulnerable and it needs support “on all fronts.” So, you should maximally exclude from the diet foods that load the liver and disrupt the motility of the biliary tract: fatty and fried foods, exclude smoked and pickled foods, any dough and fresh baked goods, baked goods (for example, dried bread, crackers and biscuits in reasonable quantities), strong, rich soups with mushroom, fish or meat broths, offal, foods cooked on the grill or fire, canned food, legumes, spices.
Essentiale during pregnancy
The drug Essentiale is recommended during pregnancy as a means of relieving toxicosis and nausea syndromes. However, during this period it should be taken strictly on the recommendation of a specialist, excluding potential risks for both the fetus and the expectant mother. But during breastfeeding, this drug is contraindicated, since research in this area has not been conducted.

![Table 1. Comparison of the results of treatment with Tribestan for men with oligoasthenozoospermia [7] with mod.](https://laram-halal.ru/wp-content/uploads/tablica-1-sravnenie-rezultatov-lecheniya-tribestanom-muzhchin-s-oligoastenozoospermiej-7-330x140.jpg)