Release form, composition and packaging
Ointment for external use is white or almost white in color, with a characteristic odor.
| 1 g | |
| silver sulfadiazine | 10 mg |
Excipients: vaseline oil - 230 mg, propylene glycol - 100 mg, cetostearyl alcohol - 60 mg, glyceryl monostearate 40-55 - 30 mg, polysorbate 80 - 20 mg, methyl parahydroxybenzoate - 0.8 mg, propyl parahydroxybenzoate - 0.2 mg, purified water - up to 1 G.
50 g - aluminum tubes (1) - cardboard packs.
Directions for use and doses
Externally, both openly and in the form of occlusive dressings.
After cleansing and surgical treatment, a preparation of 2–3 mm thickness is applied to the wound under sterile conditions 2–3 times a day. During treatment, the entire wound should be covered with cream. If part of the wound opens, additional cream must be applied. The application of an occlusive dressing is possible, but not mandatory.
The cream is applied until the wound is completely healed or until the skin is transplanted. If the drug is used on infected wounds, exudate may appear. Before using the cream, you must wash the wound with an antiseptic.
The maximum daily dose is 25 g. The maximum duration of treatment is 60 days.
pharmachologic effect
Broad-spectrum antimicrobial agent, sulfonamide. Has a bactericidal effect.
The drug is active against gram-positive and gram-negative bacteria (Escherichia coli, Proteus spp., Staphylococcus spp., Klebsiella spp.).
The bactericidal properties of Sulfargin® ointment are due to the activity of silver ions, which are released in the wound as a result of the dissociation of the silver salt of sulfadiazine; The release of silver ions occurs gradually (moderate dissociation), ensuring a constant antimicrobial effect. The bactericidal activity of silver ions is complemented by the bacteriostatic effect of sulfadiazine (also released during the dissociation of the silver salt of sulfadiazine).
Sulfargin® is characterized by moderate osmotic activity and does not have necrolytic properties.
ARGOSULPHAN in the treatment of trophic and diabetic ulcers of the lower extremities B.S. Briskin, A.V. Proshin, M.V. Polyansky, Ya.I. Yakobishvili, E.V. Kuznetsov Moscow State Medical and Dental University City Clinical Hospital No. 81Trophic ulcers most often complicate the course of the underlying disease - varicose or postthrombophlebetic disease, diabetic foot syndrome [3]. From the point of view of modern basic theory, trophic disorders in chronic venous insufficiency (CVI) are a consequence of valvular insufficiency of various parts of the venous bed of the lower extremities, as a result of which phlebohypertension forms and increases. The latter does not cause direct tissue destruction, but acts through a cascade of pathological changes at the molecular, cellular, microcirculatory and tissue levels. The main proven pathogenetic mechanisms of trophic disorders in CVI are [4]: – leukocyte trapping – a significant increase in the number of leukocytes in the veins and venules of the affected limb; – occlusion of microvasculature vessels due to smudging and formation of microthrombi; – activation of leukocytes and their penetration into surrounding tissues; – extravasal polymerization of fibrinogen in the form of a fibrin “cuff” around the venous and arterial limbs of the capillaries; – swelling of soft tissues, which results in an increase in the distance between capillaries and a deterioration in metabolic processes. Ultimately, tissue damage develops with the emergence of a primary affect. Diabetic trophic ulcers are a consequence of diabetic macro-microangiopathy and polyneuropathy. The main cause of morbidity, hospitalization and mortality in patients with diabetes is infection of the lower extremities. Infection is a common complication of developing ulcers or wounds on the foot [8]. In conditions of impaired blood flow, infection significantly worsens the prognosis of the likelihood of saving a limb or even life itself [2]. The infectious process promotes thrombosis of arteries already changed due to atherosclerosis, which leads to the progression of ischemia and the development of gangrene [6]. Currently, the polymicrobial nature of a purulent focus with an association of aerobes and anaerobes on the feet of patients with diabetes is generally accepted [5, 7]. The arsenal of drugs used for local treatment of wounds has now expanded significantly, but its results remain not entirely satisfactory due to the high cost and low availability of a number of drugs. Inpatient treatment for several months is not economically feasible [1]. One of the alternative methods of local treatment of trophic ulcers of the lower extremities of various etiologies is the administration of the drug Argosulfan, which is a 2% silver salt sulfathiazole cream. It has been established that the combination of silver with sulfonamides has an antibacterial effect that is several tens of times more powerful than sulfonamides alone. Argosulfan has a local antimicrobial effect, exhibiting a wide spectrum of action against gram-negative and gram-positive bacteria. The antibacterial effect of sulfathiazole is enhanced by the influence of silver, which has an oligodynamic effect and at the same time weakens the sensitizing properties of sulfonamides. Silver ions inhibit the growth and division of bacteria by binding to DNA. Sulfathiazole inhibits the proliferation of bacteria. In addition, silver helps accelerate regenerative processes in the wound. The low solubility of the silver salt of sulfathiazole makes it possible to maintain a constant concentration of the drug in the wound, and also ensures non-toxicity due to minimal resorption. The hydrophilic base and appropriate pH level of Argosulfan cream ensure its analgesic effect and good tolerability. It should be emphasized that the drug is stable and does not decompose under the influence of light. Materials and research methods The study was carried out on the basis of the department of purulent-septic surgery of City Clinical Hospital No. 81. An analysis of the results of treatment of 72 patients with trophic defects of soft tissues of various locations and origins, in whom Argosulfan was used as local treatment, was carried out. Of these, 44 patients were in the hospital for complicated forms of diabetic foot (wounds after treatment of diabetic phlegmon and gangrene of the feet), 26 - with trophic ulcers of the legs against the background of chronic venous insufficiency with a duration of existence from 3 to 5 years. The age of the patients ranged from 36 to 76 years. There were 31 men (43.1%), 41 women (56.9%). The characteristics of patients by age and sex are presented in Table 1. The average duration of diabetes mellitus in 44 patients exceeded 15 years, which undoubtedly influenced the severity of the wound process due to neuro-vegetative disorders and pronounced changes in microcirculation. The absence of a working classification of diabetic foot syndrome in domestic surgical practice allows us to propose a generalized classification developed in our clinic, taking into account the morpho-anatomical changes in the foot, reflecting the state of regional blood flow and sensorimotor disorders [1]. Classification of complicated forms of diabetic foot syndrome A. By form: 1. Neuropathic foot; 2. Ischemic foot; 3. Neuroischemic foot.
B. According to the extent of the lesion (Wagner): degree 0 – no changes in the skin or bone deformities; 1st degree – superficial ulcer without penetration into the deeper layers; 2nd degree - superficial ulcer with damage to the tendon, bone, articular ligaments; 3rd degree – inflammation of the tendon sheath, osteomyelitis or deep abscesses; 4th degree – gangrene of the fingers or the entire foot; Grade 5 – gangrene of the entire leg.
B. According to the location and nature of the lesion: Right, left foot, damage to both feet. The surface is dorsal, plantar, and both at the same time. Foot area – toes, metatarsus, tarsus, joints, foot as a whole.
1. Fingers (felons: cutaneous, nail (paronychia, subungual felon), subcutaneous, tendon (purulent tendovaginitis, plantar and dorsal purulent tendobursitis), bone, articular, osteoarticular) 1.1. Ulcer: superficial, perforating 1.2. Acral necrosis of the finger 1.3. Pandactylitis: gangrene – dry, wet.
2. Foot 2.1. Abscesses 2.1.1. Skin 2.1.2. Mozolny
2.2. Cellulitis: 2.2.1. Epifascial plantar and dorsal surface 2.2.2. Interdigital 2.2.3. Subaponeurotic of the plantar surface and dorsum of the foot 2.2.4. Lateral plantar space 2.2.5. Medial plantar space 2.2.6. Median plantar space
2.3. Foot ulcer 2.3.1. Surface 2.3.2. Perforating
2.4. Gangrene of the foot 2.4.1. Dry 2.4.2.Wet
2.5. Panphlegmon.
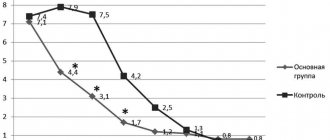
Based on the proposed classification, 26 patients (59.1%) were diagnosed with a neuropathic form of foot damage, and 18 (40.9%) - neuroischemic. The neuroischemic form of foot damage occurred with a predominance of neuropathy - in 65% and dominance of ischemia - in 35%. The group of observed patients included patients with types I and II diabetes mellitus. In table Figure 2 shows the distribution of patients depending on the type of diabetes, its severity and insulin dependence. All the patients we studied with complicated diabetic foot syndrome had trophic disorders in the tissues of the foot with the formation of ulcers, abscesses, phlegmon, osteomyelitis, necrosis, and gangrene. All patients underwent various organ-preserving surgical interventions on the foot (opening and drainage of phlegmons, disarticulation of fingers, foot resections, necrectomy). The control group included 88 patients with trophic ulcers and wounds on the lower extremities. Of these, 56 were with complicated diabetic foot syndrome and 32 were with trophic ulcers due to venous insufficiency, who received standard medications (dioxidine, chlorhexidine, ointment dressings with Levosin, Levomekol) as local treatment for wound healing. To assess the effectiveness of the ongoing antibacterial therapy, we used data from cytological studies of contents from wounds and microbial contamination of the tissues of the purulent focus. Results and discussion The use of Argosulfan in the local treatment of wound processes made it possible to improve the course of the wound process in all patients. This was expressed, first of all, in the reduction or disappearance of pain during and outside of dressings, in the cleansing of the wound defect from necrotic tissue with the appearance of mature granulations and marginal epithelization in the area of the ulcer by the 10th day of treatment in 24 of 26 patients with CVI of the lower extremities, as well as the absence or sharp decrease (up to 102) of microflora growth. The most frequently sown pathogens in this group of patients were Staphylococcus aureus – 78%, Pseudomonas aeruginosa – 13%, Proteus vulgaris – 9%. The use of Argosulfan in patients of this group led to rapid scarring of ulcers (on average within 20–22 days depending on the depth and extent of the defect), in 18 patients and in 8 it allowed to prepare the trophic ulcer for plastic closure, in contrast to patients in the control group, where this dynamics in terms of the wound process was noted only by 30–32 days. In patients with complicated diabetic foot syndrome, positive dynamics in local wound treatment were also obtained in the vast majority of patients. Locally: in 26 patients with a neuropathic form of foot damage, a decrease or disappearance of swelling on the foot, a decrease or relief of the phenomena of bacterial cellulite, a limitation of necrosis, and a tendency to cleanse postoperative wounds were noted. The most frequently cultured pathogens in patients with complicated diabetic foot syndrome are presented in Table. 3. With the neuroischemic form of foot damage, all patients noted a limitation of the purulent-necrotic process on the foot with a tendency to clear it with relief of the phenomena of perifocal inflammation. It should be noted that preventing the generalization of infection on the foot in this category of patients made it possible to carry out a complex of conservative therapy or perform reconstructive surgery aimed at relieving the phenomena of critical ischemia in the affected foot. We consider this point important in the pathogenetic treatment of the neuroischemic form of foot injury, since early radical surgical interventions on the foot without restoring blood flow under conditions of ischemia lead to the generalization of infection with the development of gangrene, which ends in high amputation of the limb. In 4 patients, against the background of local application of Argosulfan and complex conservative therapy, reconstructive surgical interventions on the arteries of the lower extremities were successfully performed, and in 8 patients, extraperitoneal lumbar sympathectomy was performed, aimed at improving regional blood flow in the affected limb. Thus, the clinical effectiveness of local treatment of wound processes with Argosulfan was 100%. The duration of local treatment with Argosulfan in patients with complicated diabetic foot syndrome was carried out on average 14–20 days, until a clear clinical effect appeared and the level of microbial contamination in the wound decreased to 103 microbial bodies per 1 g of tissue, which allowed the wound to heal or prepare it for plastic surgery. closing To assess the effectiveness of the treatment, data from studies of cytological prints from wounds and microbial contamination of the tissues of the purulent focus were used. Cytological examination of wound prints makes it possible to judge the nature and phases of the wound process, the effectiveness of the complex treatment, and, in turn, determine indications or contraindications for various conservative and surgical measures. Cytological examination was based on determining the quantitative and qualitative composition of neutrophils, lymphocytes, macrophages, fibroblasts, and the presence of microflora. For a more accurate idea of the dynamics of the cellular composition, it was expressed as a percentage when counting 100 cells in different parts of the preparation, depending on the homogeneity of the cellular composition of wound prints in patients with various forms of complicated diabetic foot syndrome (neuropathic, neuroischemic). Analysis of the data obtained indicates that upon admission to the hospital in 23% of patients, the cytology of the wound process was degenerative-inflammatory in nature. The cellular composition of the wound in this type of cytogram was characterized by the presence of neutrophils in a state of varying degrees of destruction, as well as a large number of microorganisms. In 39% of patients, a purulent-necrotic type of cytogram was noted. This was evidenced by a large number of neutrophils in a state of degeneration and destruction. In all patients, the presence of microorganisms was noted among the destroyed neutrophils in the cytograms. In 38% of patients, the cytology of the wound process corresponded to the purulent-inflammatory type. In this group of patients, the cellular composition was characterized by a predominance of neutrophils, most of which were in the stage of decay. Other cellular elements in the wound print had degenerative changes. The cytological dynamics of the wound process were assessed from the moment the patient was admitted, on days 3, 5, 10, 15 of treatment. On days 10–14 of antibacterial therapy with levofloxacin, the cytological characteristics of the wound process changed - in 42% with a transition to the inflammatory type, in 38% to the inflammatory-regenerative type, which was characterized by the predominance of a neutrophilic reaction, combined with a high level of lymphocytes and macrophages, as well as the presence in smears-imprints of single fibroblasts. Continuing the course of antibacterial therapy in patients with the inflammatory type of cytogram for 10–14 days made it possible to change it to regenerative in 79% of patients. At the same time, it was possible to achieve a reduction in the level of microbial contamination in the purulent focus to 103–104 microbial bodies in 97% of patients, in contrast to the control group, where this degree of microbial contamination was achieved only in 78%. A complex of clinical, microbiological and cytological studies made it possible to resolve the issue of discontinuing antibacterial drugs. Further treatment of the open wound was carried out only under dressings with Argosulfan, which provides a high antimicrobial effect directly in the wound. In the control group, 36% of patients continued to use broad-spectrum antibiotic therapy. Conclusions 1. Argosulfan mixes well with wound secretions and prevents the gauze bandage from sticking to the wound surface. 2. During treatment with the drug, activation of the processes of granulation and epithelization in the wound surface is observed. 3. Argosulfan is well tolerated by patients; no cases of local or general allergic reactions were detected during treatment. 4. Argosulfan 2% cream effectively prevents the occurrence of reinfection of the wound surface due to a wide spectrum of antimicrobial activity.
ABSTRACT Argosulfan in the treatment of trophic and diabetic ulcers of the lower extremities The article presents the results of our own study of the effectiveness of Argosulfan in the treatment of trophic and diabetic ulcers of the lower extremities. During the study, the clinical effectiveness of local treatment of wound processes with Argosulfan was 100%. Acceleration of granulation and epithelization of the wound surface and a decrease in microbial contamination were observed. The drug is easy to use, does not cause adverse reactions and can be recommended as a local antibacterial and wound healing agent for widespread use in clinical practice in patients with trophic ulcers of the lower extremities.
REFERENCES 1. Briskin B.S., Proshin A.V., Kuznetsov E.V. et al. Main directions in complex therapy of patients with complicated forms of diabetic foot //International Medical Journal. 2001. No. 8. P. 49-52. 2. Dibirov M.D., Briskin B.S. Surgical treatment of complications of diabetic angiopathy // Moscow. 2001. 327 p. 3. Kirienko V.Yu., Bogachev V.Yu., Bogdanets L.I. Treatment of trophic ulcers of venous etiology // Consilium medicum. 2000. pp. 22-26. 4. Savelyev V.S., Kirienko A.I., Bogachev V.Yu. Venous trophic ulcers // Phlebolymphology. 2000. No. 11. P. 5-10. 5. Svetukhin A.M., Zemlyanoy A.B. Purulent-necrotic forms of diabetic foot syndrome // Consilium medicum. 2002. T. 4. No. 10. P. 537-544. 6. Boyko EJ, Lipsky BA Infection and diabetes. In: Harris (ed) Diabetes in America, 2nd Ed. Bethesda, Md., National Institutes of Health Publication 1995:95 – 1468. 7. Gerding DN Foot infections in diabetic patients: the role of anaerobes. Clin. Infect. Dis 1995;20(Suppl. 2):283- 8. Lipsky EA Infections problems of the foot in diabetic patients. Levin and O'Neal's The Diabetic Foot. Eds. Bowker JH, Pfeifer MA St. Louis, C. V. Mosby, 6th Ed. 2001. 467-80.
Polyclinic No. 2 2006 (14-19)
Dosage regimen
Apply externally.
After surgical treatment of the wound and removal of necrotic tissue, the ointment is applied to the damaged surface in a thin layer of 2-4 mm (under a bandage or open method) 1-2 times a day. The maximum single dose is 300 g. The duration of treatment is determined individually, depends on the nature of the disease and the effectiveness of the treatment used and, as a rule, is up to 3 weeks.
If the use of the drug was missed, apply the ointment as quickly as possible and continue use at the usual time, without doubling the dose.
If the patient feels that the effect of the drug is too strong or weak, the doctor or pharmacist should be informed.
Contraindications
Hypersensitivity (including to other sulfonamides), congenital deficiency of glucose-6-phosphate dehydrogenase, early childhood (newborns and infants up to 2 months, premature infants) due to the risk of developing kernicterus.
Not recommended for use during pregnancy. During breastfeeding, the drug can be prescribed only if the burn surface does not exceed 20% of the body surface, and the therapeutic benefit to the mother is greater than the possible risk to the child.
Side effect
Local reactions: burning and itching at the site of application, impaired skin pigmentation, allergic skin reactions, skin necrosis.
Systemic reactions: erythema multiforme, interstitial nephritis, leukopenia, which is characterized mainly by a decrease in the number of neutrophils. The maximum decrease in the number of leukocytes is observed 2-4 days after the start of treatment; normalization of the number of leukocytes is observed on days 2-4, while continued treatment with the drug does not affect the process of restoring the number of leukocytes.
With long-term use on large wound surfaces: systemic side effects characteristic of sulfonamides, incl. hematopoietic disorders (agranulocytosis, aplastic and hemolytic anemia, thrombocytopenia, leukopenia), skin and allergic reactions, incl. Stevens-Johnson syndrome and exfoliative dermatitis; dyspepsia, hepatitis, hepatocellular necrosis, dysfunction of the central nervous system and toxic nephrosis.
The degree of absorption of the drug depends on the size of the burn surface and the degree of tissue damage.
Pharmacokinetics
The silver salt of sulfathiazole contained in the drug has low solubility, as a result of which, after local application, the concentration of the drug in the wound is maintained at the same level for a long time. Due to minimal resorption of the drug, it does not have a toxic effect. Only a small amount of sulfathiazole silver salt ends up in the bloodstream, after which it undergoes acetylation in the liver.
In urine it is found in the form of inactive metabolites and partially unchanged. Absorption of sulfathiazole increases after use of the drug on large wound surfaces.
Contraindications for use
- pregnancy;
- lactation period;
- severe deficiency of glucose-6-phosphate dehydrogenase;
- children under 1 year of age;
- hypersensitivity to sulfonamides.
The drug should not be used to treat deep purulent wounds and burn surfaces with heavy exudation.
With caution: renal/liver failure, glucose-6-phosphate dehydrogenase deficiency (risk of hemolysis).
Before using the medicine, we recommend that you consult your doctor online
Indications for the drug Argosulfan®
Burns of varying degrees, of any nature (thermal, solar, chemical, electric shock, radiation, etc.), frostbite.
Bedsores, trophic ulcers of the leg of various origins (including chronic venous insufficiency, obliterating endarteritis, circulatory disorders due to diabetes, erysipelas, etc.).
Purulent wounds, minor household injuries (cuts, abrasions).
Infected dermatitis, simple contact dermatitis, complicated by impetigo, microbial eczema, streptostaphyloderma.
special instructions
When treating patients with liver and/or renal failure, it is necessary to regularly monitor the concentration of sulfonamides in plasma.
Silver salts, when reacting with atmospheric oxygen, metals and other chemical components, especially under catalytic heat, darken, so the drug should be stored in a closed container and away from heat sources.
It is recommended to protect parts of the body treated with the drug from direct sunlight.
Impact on the ability to drive vehicles and machinery
The drug does not affect the ability to drive vehicles or engage in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.