The main purpose of ultrasound of the abdominal aorta is to identify an aneurysm or atherosclerotic lesion of the aorta and damage to its large branches: splenic, hepatic, renal and mesenteric arteries. Ultrasound of the abdominal aorta is a non-invasive diagnostic method that has high value in identifying many vascular diseases. The results of ultrasound are very dependent on the examination technology, the quality of the equipment and the qualifications of the specialist. Today, the low price of ultrasound of the aorta and abdominal organs, the simplicity and safety of the study make it indispensable for the primary detection of abdominal aortic aneurysm.
The innovative vascular center specializes in vascular surgery, so we strive to diagnose vascular pathology at the highest level. Our center has excellent stationary and mobile ultrasound machines that allow us to study in detail the structure of the aortic wall and its branches, as well as identify aneurysms. The specialists of our medical center are dedicated to working specifically with vascular pathology, therefore they identify it much better than general ultrasound doctors.
What is the aorta
The aorta is the largest vessel in the human body, which carries blood from the heart to the organs and limbs. The upper section of the aorta runs inside the chest, this section is called the thoracic aorta . The lower part is in the abdominal cavity and is called the abdominal aorta . It delivers blood to the lower part of the body. In the lower abdomen, the abdominal aorta divides into two large vessels - the iliac arteries , which carry blood to the lower extremities.
The aortic wall consists of three layers: internal (intima), middle (media), external (adventitia).
Interpretation of ultrasound data of the abdominal aorta
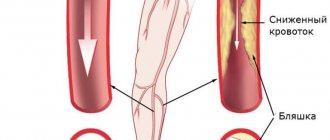
During an ultrasound of the aorta and abdominal vessels, the doctor examines the size of the aorta and its lumen, how evenly it is colored during Doppler mapping. Dilatation of the abdominal aorta of more than 4 cm speaks in favor of an aneurysm. Ultrasound diagnostics allows you to assess the condition of the arteries of the kidneys, intestines, liver and stomach. It is possible to detect dilation of the arteries of internal organs. With complicated aneurysms, it is possible to detect a retroperitoneal hematoma due to rupture, fluid in the abdominal cavity, thrombosis of the aorta or visceral arteries. Often, a good ultrasound scanner can detect dissection of the vessel wall, its tears and atherosclerotic plaques. Ultrasound of the abdominal aorta and visceral branches lasts about 25-40 minutes. After the examination, you can immediately return to normal activities.
Abdominal aortic aneurysm
Abdominal aortic aneurysm is a chronic degenerative disease with life-threatening complications. An abdominal aortic aneurysm is defined as an increase in its diameter by more than 50% compared to the norm or a local bulging of its wall. Under the pressure of blood flowing through this vessel, the dilatation or bulging of the aorta may progress. The diameter of a normal aorta in the abdominal region is approximately 2 cm. However, at the site of an aneurysm, the aorta can be dilated to 7 cm or more.
Why is an aortic aneurysm dangerous?
An aortic aneurysm poses a major health risk as it can rupture. A ruptured aneurysm can cause massive internal bleeding, which in turn leads to shock or death.
An abdominal aortic aneurysm can cause other serious health problems. Blood clots (thrombi) often form in the aneurysm sac or parts of the aneurysm tear off, which move with the blood flow along the branches of the aorta to the internal organs and limbs. If one of the blood vessels becomes blocked, it can cause severe pain and lead to organ death or loss of a lower limb. Fortunately, if an aortic aneurysm is diagnosed early, treatment can be timely, safe and effective.
Abdominal aorta
The aorta is considered to be a straight artery, which at the same time is a large blood vessel in the systemic human circulation. The aorta has three sections: two parts of the aorta, and its arch. The lower part of the aorta can be divided into sternal and peritoneal zones. The abdominal aorta is considered a continuation of the thoracic aorta. It is located on the frontal part of the lumbar vertebrae, or rather literally a few millimeters moving away to the left from the medial line. This aorta for the most part has a length of 13 cm and a diameter of 17 mm. Its origin lies in the area of the twelfth thoracic vertebra. After this, it reaches almost the fifth lumbar vertebra by number. At this point the aorta divides into the iliac arteries. To the right of the abdominal aorta is the inferior vena cava. The abdominal aorta in its frontal zone has the splenic vein, the pancreas, the lower surface of the duodenum is also found here, the renal vein is attached in the same place, or rather its left part, the root of the mesentery, the parietal leaf of the abdominal cavity. The thoracic duct cistern is located behind the first surface of the abdominal aorta. Along the path of the abdominal aorta, the parietal and splanchnic blood veins diverge.
By parietal vessels we mean the lower artery of the diaphragm, as well as the arteries related to the lower back. The inferior phrenic artery is the largest blood branch, which has its own pair, but at the same time supplies blood to the lower zone of the diaphragm and the adrenal glands. The lumbar arteries in our body are represented by four paired arteries, which are connected to each other, but also to two epigastric arteries. They deliver blood to fiber, muscles in the abdomen and back, skin and spinal cord.
The internal branches are divided into two sets, which can be called paired and unpaired. The arteries included in the paired group include the middle adrenal artery, which supplies the adrenal gland; the parenchyma of the gland is connected by two branches of the adrenal arteries. The renal artery, moving behind the inferior vena cava, reaches the parenchyma of the kidney and at the portal of the kidney separates a branch, namely the inferior adrenal artery, which delivers blood to the adrenal gland. And the testicular artery, which supplies blood to the ovaries and their appendages. In women, such an artery is called the ovarian artery. It saturates important female organs with blood.
The group of unpaired arteries contains the celiac trunk and both mesenteric arteries. This trunk is a small and fairly short vessel, the length of which reaches only two centimeters. It begins at the aorta in the region of the 12th vertebra of the sternum and is divided into three branches. On the gastric artery on the left, which supplies blood to the lesser curvature and body of the stomach, the human esophagus due to the esophageal branches extending from it, another single hepatic and splenic arteries. The hepatic artery brings blood to such important organs as the liver, gall bladder, stomach walls and even the greater omentum. The splenic artery allows blood to flow to the spleen, the wall of the stomach, the greater omentum, and some part of the pancreas.
The abdominal aorta, namely the superior mesenteric artery, is formed in the area of the second lumbar vertebra, or rather in the area of the head of the pancreas, then it is located on the anterior surface of the ascending region of the duodenum, and then reaches the iliac fossa. The superior mesenteric vessel has its own branch, called the pancreaticoduodenal artery, colonic artery, and various types of colonic arteries.
The inferior mesenteric artery begins at the third lumbar vertebra, and then moves behind the peritoneum slightly down and to the left. On its way, it creates several branches, namely the colon artery on the left, the sigmoid artery, and the rectal artery at the top. The artery that is located on the left to the descending zone of the intestine and the transverse region of the intestine is the blood. The sigmoid colon artery supplies blood to the sigmoid colon. The superior artery supplies blood to the walls of the sigmoid colon and a certain lobe of the rectum.
Types of aortic aneurysms
There are “true” and “false” aortic aneurysms. A true aneurysm develops due to the gradual weakening of all layers of the aortic wall. A false aneurysm is usually the result of trauma. It is formed from the connective tissue surrounding the aorta. The cavity of the false aneurysm is filled with blood through a crack in the aortic wall. The aortic walls themselves do not participate in the formation of an aneurysm.
Depending on the form there are:
- saccular aneurysm - expansion of the aortic cavity on only one side;
- spindle-shaped (fusiform) aneurysm - expansion of the aneurysm cavity on all sides;
- mixed aneurysm - a combination of saccular and fusiform forms.
How is an ultrasound of the abdominal aorta and its branches performed?
The principle of ultrasound scanning of the abdominal cavity is to process the ultrasound signal reflected from the organs. This allows you to evaluate the structure and size of this organ. Ultrasound examination of the abdominal aorta is not dangerous and does not cause any discomfort. The diagnostic process itself includes only a few steps:
- In the ultrasound diagnostic room, the patient sits on the couch to the right of the doctor and opens his stomach.
- The doctor lubricates a special sensor and the patient’s abdomen with a transparent gel, which reduces tissue resistance and helps the ultrasound wave penetrate inside.
- The specialist then slowly moves the sensor along the abdominal wall and records the results of the observations.
The capabilities of ultrasound devices allow not only to assess the size, shape and structure of the vessel wall, but also to study the characteristics of blood flow. This is achieved using Doppler ultrasound and color Doppler mapping. Dopplerography is based on recording the ultrasonic signal from moving red blood cells and changing the speed of this signal depending on the approach or distance of these particles to the sensor. The speed of blood flow, determined by Doppler ultrasound, is an indicator of the patency of blood vessels below the study site or in areas of narrowing of the vessel. In narrowed places it is significantly strengthened; if there is an obstacle to the outflow of blood below the test site, then the speed decreases.
Causes and risk factors for the development of abdominal aortic aneurysm
The causes of the development of abdominal aortic aneurysms are very diverse. The most common cause of aneurysm development is atherosclerosis. Atherosclerotic aneurysms account for 96% of the total number of all aneurysms. In addition, the disease can be either congenital (fibromuscular dysplasia, Erdheim's cystic medianecrosis, Marfan syndrome, etc.) or acquired (inflammatory and non-inflammatory). Inflammation of the aorta occurs when various microorganisms invade (syphilis, tuberculosis, salmonellosis, etc.) or as a result of an allergic-inflammatory process (nonspecific aortoarteritis). Non-inflammatory aneurysms most often develop with atherosclerotic lesions of the aorta. Less commonly, they are the result of injury to its wall.
Risk factors for developing an aneurysm
- Arterial hypertension;
- Smoking;
- The presence of aneurysms in other family members. Which indicates the role of hereditary factors in the development of this disease;
- Gender: men over 60 years of age (abdominal aortic aneurysms occur less frequently in women).
Symptoms and signs of abdominal aortic aneurysm
In most patients, abdominal aortic aneurysms occur without any symptoms and are an incidental finding during examinations and operations for other reasons.
When signs of an aneurysm develop, the patient experiences one or more of the following symptoms:
- A feeling of pulsation in the abdomen, similar to a heartbeat, an unpleasant feeling of heaviness or fullness.
- Dull, aching pain in the abdomen, in the navel area, usually on the left.
Indirect signs of abdominal aortic aneurysm are important :
- Abdominal syndrome. Manifested by the appearance of belching, vomiting, unstable stool or constipation, lack of appetite and weight loss;
- Ischioradic syndrome. Manifested by lower back pain, sensory disturbances and movement disorders in the lower extremities;
- Syndrome of chronic ischemia of the lower extremities. Manifests itself in the appearance of pain in the muscles of the lower extremities when walking, sometimes at rest, coldness of the skin of the lower extremities;
- Urological syndrome. It manifests itself as pain and heaviness in the lower back, difficulty urinating, and the appearance of blood in the urine.
Harbingers of rupture may be increased abdominal pain.
When an aneurysm ruptures, the patient suddenly feels an increase or appearance of abdominal pain, sometimes “radiating” to the lower back, groin area and perineum, as well as severe weakness and dizziness. These are symptoms of massive internal bleeding. The development of such a situation is life-threatening! The patient needs emergency medical care!
Classification of forms of the disease:
Celiac stenosis (supplies blood to the liver, spleen, stomach, pancreas)
This is a condition in which the lumen of the celiac trunk narrows, can be acquired - develops when the vessel is damaged by atherosclerosis, or congenital - when compressed from the outside by the arcuate ligament of the diaphragm (much less often - with inflammatory diseases, aortic aneurysms, congenital malformations, compression by neoplasms of the abdominal cavity). The first reason is often combined with damage to other arteries (coronary - intracardiac arteries, carotid, arteries of the lower extremities), the second reason is a congenital condition, the manifestations of which develop at a young age. The main organs experiencing a lack of blood supply are the stomach, liver and pancreas, but the intestines also suffer due to the “steal syndrome”. Significant narrowing of the lumen of the artery is currently considered to be more than 50% of the original diameter. Symptoms of the disease - abdominal pain, bloating, stool disorders in the form of alternating diarrhea and constipation, nausea, weight loss - are combined into a single syndrome - the syndrome of “chronic abdominal ischemia” (chronic ischemic disease of the digestive organs, abdominal ischemic disease).
The cause of the narrowing of the vessel can be determined using:
- duplex scanning of abdominal vessels,
- performing angiography or multislice computed tomography angiography (MSCT angiography).
When establishing indications and choosing a method of surgical treatment, the patient’s age, the severity of complaints, the effectiveness of conservative treatment (without surgery), and the degree of compensation for the functions of the involved organs are taken into account. Indications for surgical treatment, according to modern standards, should be established jointly by a gastroenterologist and a vascular surgeon.
There are the following types of operations:
- Endovascular balloon angioplasty with celiac axis stenting.
This intervention is performed through a puncture in the femoral, and less commonly, in other arteries. Using special thin instruments, the narrowed section of the celiac trunk is expanded from the inside until the normal diameter of the lumen is restored, and a stent is installed - a thin “frame” made of inert alloys, which subsequently prevents re-narrowing of the artery. It is most often used when the celiac trunk is damaged by atherosclerosis. - Laparoscopic decompression of the celiac trunk.
The operation is performed minimally invasively using separate punctures. This method allows you to incise the ligament of the diaphragm, “releasing” the celiac trunk from its pressure. In this case, the artery straightens, eventually restoring its normal diameter. Previously, such operations were performed on the open abdominal cavity, which was sometimes accompanied by a difficult postoperative period, characteristic of open operations, so their prevalence was limited. The development of laparoscopic surgery has made it possible to perform these interventions with good postoperative and cosmetic results. - Shunt operations for narrowing/blockage of the celiac trunk or its prosthetics.
They are performed in advanced stages of atherosclerosis, when it is not possible to install a stent or remove an atherosclerotic plaque from a vessel. The essence of the operations is to create a bypass blood flow in addition to the affected celiac trunk, or to replace it with an artificial prosthesis. These interventions are technically complex, are performed only in the open abdominal cavity and require highly qualified vascular surgeons.
Stenosis of the superior mesenteric artery
It is much less common than celiac stenosis. The most common causes of the disease are atherosclerotic narrowing of the lumen of the superior mesenteric artery (against the background of systemic atherosclerosis) and a congenital disorder of the structure of the artery wall - fibromuscular dysplasia. The superior mesenteric artery branches into many smaller vessels that supply the small intestine and part of the colon. The disease often occurs without any symptoms and is difficult to diagnose until serious complications occur—complete blockage of the superior mesenteric artery or its branches. In this condition, patients are admitted to a surgical hospital with signs of transient necrosis of a section of the intestine deprived of blood supply, which is sometimes very difficult to distinguish from other acute surgical diseases of the abdomen. In this case, an emergency operation is required - resection of a non-viable section of the intestine.
You can make a diagnosis in the early stages using:
- Doppler ultrasound of the abdominal aorta and its branches (diagnostic efficiency is about 50%),
- magnetic resonance imaging (diagnostic efficiency is about 80%),
- angiography of the abdominal aorta and its branches (allows us to determine the presence of vessel narrowing in 90% of cases).
Treatment for early detection of stenosis of the superior mesenteric artery is similar to the treatment of systemic atherosclerosis, however, with significant narrowing of the artery, surgical intervention - endovascular angioplasty - is possible.
Renal artery stenosis
Narrowing of the renal arteries develops as a result of atherosclerotic lesions, as well as with a more rare disease - fibromuscular dysplasia. Violation of blood flow to one or both kidneys is accompanied by a general negative reaction of the body. A kidney experiencing a blood deficiency receives false “information” about the total blood volume, and begins to react as if the total amount of blood in the body has decreased. The processes of hormone synthesis are intensified, aimed at retaining water in the body to maintain a constant volume of fluid in the general bloodstream. This mechanism is pathological, since the amount of blood remains the same, and, due to the production of renal hormones, an additional volume of water from the cells enters the bloodstream. As a result, persistent renal arterial hypertension develops - an increase in blood pressure above normal levels, which is difficult to reduce with medications. Swelling and cardiac dysfunction appear. This type of arterial hypertension is usually recognized in time by attending physicians, and ultrasound examination can often detect damage to the renal arteries. Open surgery to restore blood flow through the renal artery - bypass, prosthetics (replacement) of the affected area is now being performed less and less often, they are being replaced by minimally invasive endovascular methods - angioplasty and stenting.
Diagnosis of abdominal aortic aneurysms
Most often, abdominal aortic aneurysms are detected by ultrasound examination of the abdominal organs. Typically, the discovery of an aneurysm is an incidental finding. If a doctor suspects a patient has an aortic aneurysm, modern diagnostic methods are used to clarify the diagnosis.
Methods for diagnosing abdominal aortic aneurysm
- Computed tomography in angio mode;
- Magnetic resonance imaging in angio mode;
- X-ray contrast aorto- and angiography;
- Ultrasound duplex or triplex angioscanning of the abdominal aorta.
If necessary, the abdominal and thoracic aorta is examined.
Preparing for the study
To successfully perform an ultrasound of the abdominal cavity, preparation is necessary aimed at reducing the amount of gases in the intestines that interfere with seeing the retroperitoneal organs, including the aorta. The preparation rules for examining the abdominal aorta and its branches using ultrasound are simple:
- 2 days before the examination, exclude legumes, potatoes, cabbage, melon, dairy products, soda and all foods high in carbohydrates from the diet. These products may cause increased gas formation.
- On the eve of the ultrasound, start taking medications to improve bowel function. For these purposes, taking espumisan or regular activated carbon is suitable.
- It is advisable to skip dinner the evening before the procedure, and breakfast in the morning.
Treatment methods for aortic aneurysm
There are several methods for treating aortic aneurysm. It is important to know the advantages and disadvantages of each of these techniques. Approaches to the treatment of abdominal aortic aneurysms:
Monitoring the patient over time
If the aneurysm is less than 4.5 cm in diameter, the patient is recommended to be monitored by a vascular surgeon, since the risk of surgery exceeds the risk of rupture of the aortic aneurysm. Such patients should undergo repeated ultrasound examinations and/or computed tomography at least once every 6 months.
When the aneurysm diameter is more than 5 cm, surgical intervention becomes preferable, since as the size of the aneurysm increases, the risk of aneurysm rupture increases.
If the size of the aneurysm increases by more than 1 cm per year, the risk of rupture increases and surgical treatment also becomes preferable.
Open surgery: aneurysm resection and aortic replacement
Surgical treatment is aimed at preventing life-threatening complications. The risk of surgery is associated with possible complications that include heart attack, stroke, limb loss, acute intestinal ischemia, male sexual dysfunction, embolization, prosthetic infection, and renal failure.
The operation is performed under general anesthesia. The essence of the operation is to remove the aneurysmal expansion and replace it with a synthetic prosthesis. The average mortality rate for open procedures is 3-5%. However, it may be higher if the renal and/or iliac arteries are involved in the aneurysm, as well as due to the patient’s concomitant pathology. Observation in the postoperative period is carried out once a year. Long-term treatment results are good.
Endovascular repair of aortic aneurysm: installation of a stent graft
Endoprosthetics of aortic aneurysm is a modern alternative to open surgery.
The operation is performed under spinal or local anesthesia through small incisions/punctures in the groin areas. Through the above approaches, catheters are inserted into the femoral artery under X-ray control. According to which, in the future, the endoprosthesis will be brought to the aneurysmal extension. An endoprosthesis or stent-graft of the abdominal aorta is a mesh frame made of a special alloy and wrapped in synthetic material. The last stage of the operation is the installation of a stent graft at the site of the aneurysmal expansion of the aorta. Eventually, the aneurysm is “switched off” from the bloodstream and the risk of rupture becomes unlikely. After aortic replacement, the patient is observed in the hospital for 2-4 days and discharged.
This technique allows to reduce the incidence of early complications, shorten the length of patient stay in the hospital and reduce the mortality rate to 1-2%. Observation in the postoperative period is carried out every 4-6 months using ultrasound techniques, CT angiography, X-ray contrast angiography. The endovascular treatment method is certainly less traumatic. About 40,000 such operations are performed annually in the United States alone.
Thus, the choice of treatment method for abdominal aortic aneurysm is based on the individual characteristics of the patient.
Diagnostics of abdominal ultrasound:
Doppler ultrasound OR ultrasound of the abdominal cavity is done if there is a feeling of heaviness and pulsation, bloating and pain. If the cause of persistent pain is unknown, this examination will help identify the cause. To identify pathology, waves of different frequencies are used. The result is shown on the screen in the form of graphic images.
Doppler ultrasound of the abdominal region and its branches helps to identify blood flow disturbances and pathological lesions.
For example, you can determine atherosclerosis, which develops due to damage to the arteries. Cholesterol plaques form in them and clog blood vessels. Aneurysms when the vessels are dilated by more than two mm. Narrowing of the celiac trunk. It occurs because the arteries in the abdominal cavity narrow and the blood supply to the liver and kidneys is blocked. Atherosclerotic damage to blood vessels and the resulting blood obstruction. Blood clots in the abdominal aorta. Congenital bending, elongation, tortuosity of the aorta. An aorta that is dissecting due to an aneurysm. Ultrasound examination of the celiac trunk is done as soon as there is a suspicion of the disease. Because the pressure increases and the aorta can rupture. Severe bleeding will occur and death is possible. If the symptoms are bothering you for the first time and are not very pronounced, then you can do a duplex scan. This examination contains ultrasound and Doppler scanning. It is possible to do color Doppler ultrasound. View the lumen of the vessel, the structure of the walls, the degree and extent of the disturbance in blood flow. Spectral Doppler sonography is done to make a final diagnosis.