Diacerein-SZ
The duration of treatment, depending on the result achieved, can be long. In the period preceding the development of the therapeutic effect, the drug Diacerein-SZ can be taken simultaneously with analgesics and non-steroidal anti-inflammatory drugs.
Periodic monitoring of blood levels, liver enzymes, and urine is necessary. If kidney function worsens, the doctor should reduce the dose of the drug.
The use of diacerein is not recommended for rapidly progressing osteoarthritis of the hip and knee joints due to the slow development of the clinical effect of the drug.
Diarrhea
Taking diacerein often leads to the development of diarrhea (see section "Side effects"), which can cause dehydration and hypokalemia.
If diarrhea develops, stop taking the drug and contact your doctor immediately to discuss alternative treatment.
Caution should be exercised if the patient is concomitantly receiving diuretics, as dehydration and hypokalemia may occur.
Particular caution should be exercised in case of hypokalemia in patients receiving cardiac glycosides (digitoxin, digoxin) (see section “Interaction with other drugs”).
The simultaneous use of laxative drugs should be avoided.
Hepatotoxicity
During post-registration monitoring, cases of increased activity of liver enzymes in the blood serum and symptomatic acute liver damage were identified (see section “Side Effects”).
Before starting treatment, the patient should be asked about concomitant, current and history of liver diseases, and an examination should be carried out to identify violations of the functional state of the liver. Liver diseases are a contraindication to the use of diacerein (see section “Contraindications”).
It is necessary to monitor laboratory and clinical manifestations of liver damage, and observe precautions when used simultaneously with other drugs with a characteristic risk of developing hepatotoxic reactions. Patients should be advised to limit alcohol consumption while using diacerein.
Treatment with diacerein should be discontinued if an increase in liver enzyme activity is detected or the development of symptoms of liver damage is suspected. The patient should be informed of the signs and symptoms of hepatotoxicity and advised to consult a physician immediately if symptoms of liver damage are suspected.
Diacerein in the treatment of osteoarthritis of the knee joints: results of a comparative study
Osteoarthritis is one of the most common joint diseases, occurring mainly in middle and older age groups. As the world continues to experience an increasing number of older people, osteoarthritis is becoming an increasingly significant health problem. In recent years, the pathogenesis of osteoarthritis has been actively studied, with a significant role being given to pro-inflammatory mechanisms of disease development and, in particular, cytokine regulation. In this regard, the very definition of this nosological form is discussed - most authors suggest using the term “osteoarthritis,” which we will use in the future. The main clinical manifestation of osteoarthritis (OA) is pain in the affected joint, the intensity of which depends both on the severity of inflammatory changes and on the stage of OA (structural disorders of cartilage tissue, subchondral bone and soft tissue surrounding the joint). The disease is characterized by both significant heterogeneity in terms of clinical manifestations and varying rates of progression of structural abnormalities, therefore the main tasks currently facing clinicians and researchers are the identification of a group of patients with rapidly progressing variants of OA and the development of an optimal effective therapeutic algorithm. The role of pro-inflammatory cytokines in the development of osteoarthritis
Despite significant progress in understanding the pathogenetic mechanisms of OA development, cause-and-effect relationships in the process of its development and progression have not been fully established. There is a consensus understanding that OA is a heterogeneous disease with various risk factors for its development and its further course. In this case, the most important task is to establish the mechanisms of rapid progression of OA of large joints (with severe structural damage to articular tissues) and the possibilities of pharmacological correction of such disorders, since this category of patients, as a rule, often requires surgical treatment after 5–7 years . In a healthy joint, cartilage and bone homeostasis is maintained due to the balance of anabolic and catabolic processes, which are regulated by pro- and anti-inflammatory mediators, including interleukins (IL-1, -2, -6, etc.), tumor necrosis factor-α ( TNF-α) and others [1]. In OA, hyperproduction of IL-1 leads to a shift in the balance towards catabolic and anti-anabolic processes, resulting in a decrease in the synthesis of cartilage matrix components, increased degradation and remodeling of the subchondral bone. In particular, the ability of IL-1 has been proven to enhance the formation of catabolic factors by chondrocytes - matrix metalloproteinases (MMP) and nitric oxide (NO), as well as to reduce the expression of specific enzymes - tissue inhibitors of metalloproteinases (TIMP)), inhibiting the activity of MMP [ 2, 3]. IL-1 also has the ability to induce the synthesis of enzyme activators, one of which is urokinase-like plasminogen activator. Plasminogen, in turn, activates pro-MMP, which leads to subsequent degradation of the cartilage matrix [2]. It has been proven that IL-1 indirectly induces apoptosis of chondrocytes and synoviocytes, and also plays a key role in the induction of inflammatory reactions, which results in impaired functional activity of chondrocytes and a decrease in the volume of cartilage tissue in OA [1]. Along with stimulating the production of other pro-inflammatory cytokines, IL-1, through a positive feedback mechanism, induces increased own production by producer cells. Thus, the signal transmitted to the IL-1 receptor causes activation of the transcription factor and nuclear factor κB (NF-κB), which, in turn, activate the expression of the IL-1 gene, which leads to further formation of the cytokine with the development of a whole cascade of pathophysiological reactions : cartilage degradation, subchondral bone remodeling and progression of inflammatory changes [4]. Thus, taking into account the pathogenetic significance of IL-1 in the induction and maintenance of the inflammatory process in OA by influencing the mechanisms of chondrocyte apoptosis, bone remodeling, reducing the activity of anabolic processes in cartilage tissue, leading to degradation of the extracellular matrix and progression of the disease, it should be noted that drugs , affecting the production and activity of IL-1, may potentially help slow down the progression of OA.
Diacerein – a component of pathogenetic therapy of osteoarthritis
One of the symptomatic slow-activ drugs for the treatment of OA (SYSADOA - Symptomatic slow-activ drug in osteoarthritis) is diacerein, the mechanism of action of which is to inhibit the production and pathophysiological effects of IL-1. Numerous studies have demonstrated that significant positive effects from its use occur within 2–4 weeks. from the start of taking the drug with clinically significant differences from placebo at 4–6 weeks. [5, 6]. An improvement in the symptoms of the disease is also observed some time after the end of the course of therapy (the so-called “aftereffect”), which is an important positive factor influencing the long-term treatment strategy for OA (taking into account the chronic course of the disease). Diacerein has a unique mechanism of action that distinguishes it from other drugs for the treatment of OA. In particular, numerous studies have shown effective inhibition by diacerein of the production and activity of IL-1 and other catabolic cytokines that are expressed in OA, which was accompanied by a decrease in the degree of degradation of cartilage tissue [7, 8]. This was also facilitated by a decrease in the activity of plasmin, MMP and other proteases that have a negative effect on the cartilage matrix. In addition, in a study by N. Felisaz et al. (1999) demonstrated that diacerein has the ability to increase the expression of transforming growth factors (TGF-β1 and -β2) in cultured chondrocytes, which led to an increase in the number and activity of cells with increased production of hyaluronan, collagen and proteoglycans [9]. Thus, diacerein, having a pro-anabolic effect on cartilage, can be considered as an important pharmacological agent in the complex therapy of OA. This point of view is confirmed by the results of a study by M. Dougados et al. (2001), who assessed the structure-modifying effect of diacerein in patients with primary coxarthrosis [10]. The authors found that radiographic progression (narrowing of the joint space of the hip joint by at least 0.5 mm) in the group of patients taking diacerein was significantly less pronounced and developed later than in the group of patients taking placebo. An important advantage of diacerein is also the established fact of the presence of an aftereffect when using it, which was demonstrated in a double-blind, randomized, placebo-controlled study by K. Pavelka et al. [eleven].
Diacerein in the treatment of OA of the knee joints
The purpose
of this study was to study the clinical effectiveness, tolerability and safety of the drug diacerein (Diaflex) in comparison with chondroitin sulfate sodium in patients with OA of the knee joints during continuous use for 12 months, as well as to evaluate the “after-effect” effect. drugs.
Material and methods
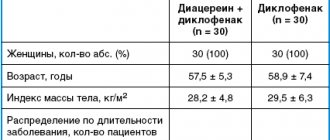
The study included 30 patients (28 women and 2 men) with OA of the knee joints stage II-III (according to Kellgren - Lawrence), meeting the criteria of the American College of Rheumatology (ACR, 1986). The average age of the patients was 60.4±6.2 years, the duration of the disease was 5.9±4.5 years. The study was conducted in accordance with the basic principles of good clinical practice. Participation in the study was allowed only after the patient voluntarily signed an informed consent and received permission from the local ethics committee. When including patients in the study, the following criteria were taken into account: • men and women aged 45–75 years; • primary tibiofemoral OA of the knee joint (according to the AKR criteria, 1986); • pain when walking > 40 mm on the visual analogue scale (VAS); • radiographic stage II–III (according to Kellgren – Lawrence). Exclusion criteria: • secondary gonarthrosis (including with rheumatoid arthritis, gout, after an intra-articular fracture, etc.); • intra-articular injections of glucocorticoids, hyaluronic acid preparations for 3 months. before the start of the study; • aseptic necrosis of the condyles of the femur and/or tibia; • previous surgical interventions on the knee joint; • concomitant severe diseases: stage III arterial hypertension, unstable angina, cardiovascular failure, type 1 diabetes mellitus, severe liver and kidney damage; • acute gastric ulcer (duodenal ulcer) during the last month before the study. The criteria for patient exclusion during the study were ineffectiveness of therapy (preservation or intensification of pain requiring a change in treatment tactics), development of serious adverse events, patient refusal from the study, or violation of the study protocol. The total duration of the study was 15 months. (12 months – taking medications and 3 months – observation). A total of 8 visits were planned: B.0 – screening, washout period (3–7 days) in case of previous use of non-steroidal anti-inflammatory drugs (NSAIDs); B.1 – randomization, initiation of therapy; B.2 – B.7 – scheduled visits after 2 weeks, 1.5, 3, 6, 9 and 12 months. after the start of therapy, respectively, and B.8 - final examination after 3 months. after the end of therapy (assessment of the aftereffect of drugs). To assess the effectiveness and safety of therapy, the following criteria were used: pain intensity according to VAS (mm), “Get up and walk” test (in seconds), WOMAC index (pain, stiffness, functional impairment), EQ-5D health questionnaire, need for analgesics , assessment of the effectiveness of therapy by the doctor and the patient, assessment of the tolerability of the therapy. All patients were randomized into 2 groups of 15 patients each: 1st group took diacerein (Diaflex) at a dose of 50 mg 2 times a day for 12 months, 2nd group took sodium chondroitin sulfate (Chondroxide) at a dose of 500 mg 2 rubles/day If the patient had pain in the first 7 days of therapy, paracetamol was allowed to be prescribed up to 2 g/day, and then on demand. The characteristics of the groups of examined patients are presented in Table 1. Almost all examined patients were diagnosed with comorbid conditions (Table 2).
Of the 30 patients included in the study, 26 (86.7%) completed the full course of treatment; During the study, 2 patients dropped out of each group: from the 1st - due to the development of side effects (diarrhea, skin rash), from the 2nd - as a result of low effectiveness of therapy. Statistical processing of the material was carried out using standard methods, including comparison in groups using the Wilcoxon method for quantitative indicators and χ2 for qualitative indicators.
results
The main complaints of patients suffering from OA are pain in the affected joint and subsequent disruption of its functional activity, and the disease itself is non-lethal, therefore very important criteria for evaluating combination therapy are the degree of pain relief and improvement in the functional activity of patients, which ultimately has an impact on the quality of life of patients. It was also important to study not only the time of onset of the analgesic effect, but also its duration. The results of the study indicate that patients taking the study drugs experienced a significant reduction in pain, which was expressed in a decrease in the VAS index (Table 3). It should be noted that, despite the absence of significant differences in the groups depending on the duration of therapy, the VAS (pain) score remained <30 throughout the entire period of active drug use. Patients with concomitant OA of the hands (forming Heberden's nodes were diagnosed in 4 patients of the 1st group and 2 of the 2nd group) noted a significant decrease in pain in the distal interphalangeal joints already 7–10 days from the start of taking Diaflex.
To assess the functional activity of patients, the “Get up and walk” test was used, which was performed on all patients before the start of treatment, during therapy and after 3 months. after completion of the course of pharmacotherapy. In accordance with the test protocol, we used a chair with armrests and a stopwatch. The patient was asked to get up from the chair, walk 5 m, walk around an object located on the floor, return and sit on the chair. The time was recorded with a stopwatch. This test well reflects the patient’s real capabilities in everyday life, since depending on the severity of the initial pain in the affected knee joint and the intensity of the pain in general, the patient’s functional abilities can be assessed. According to the presented data (Fig. 1), over time, in the examined patients, the time to perform this test was reduced, which indicates an increase in functional activity and a decrease in the severity of starting pain. There was no significant difference between the groups. It should be noted that the results of this test remained stable even after the end of pharmacotherapy (period B.7 - B.8).
When analyzing the total WOMAC index (pain, stiffness, functional joint insufficiency), patients in group 2 showed an almost linear decrease throughout the entire observation period, while in patients in group 1 (who took Diaflex), the dynamics of this indicator were significantly different (Fig. 2). So, in the first 6 months. therapy, there was a pronounced decrease in the WOMAC index, followed by its stabilization and the formation of a “plateau” at a fairly low level until visit 8. When studying individual indicators of the WOMAC index (assessment of pain, functional joint insufficiency) in the examined patients in 2 groups, the same trend was observed – a more pronounced clinical effect, including the speed of its development, when using Diaflex (Fig. 3, 4). Thus, it can be stated that the analgesic effect when using Diaflex is more pronounced and develops earlier than when using sodium chondroitin sulfate.
The overall assessment of the effectiveness of therapy with the study drugs also correlated with the presented data (Fig. 5). Thus, “significant improvement” and “improvement” were stated by 11 patients taking Diaflex, and “no effect” or “deterioration” by 2 (in group 2 – 9 and 4 patients, respectively). During the use of the study drugs, the overall need for paracetamol in patients of both groups decreased, while the analgesic was completely canceled in 7 (46.7%) patients taking Diaflex, and in 3 (20%) taking chondroitin sulfate sodium.
It can be stated that patients taking Diaflex generally assessed the effectiveness of therapy better than patients in group 2, which may have been associated with subjective sensations from faster pain relief. At the same time, as noted earlier, when comparing the final results of various indicators both at the end of the therapeutic phase (B.7 - 12 months) and during the follow-up period (B.8 - 15 months) there were no significant differences between groups were not received. Tolerability of the study drugs was satisfactory. Over the entire period, 4 patients dropped out of the study: 2 patients from group 1 - due to intolerance to the study drug and 2 patients from group 2 - due to ineffectiveness of therapy (deterioration of condition requiring intra-articular injections - patients were excluded at visits B.6 and B.7 respectively). Two patients of group 1 were excluded from the study at visits 2 and 4 (B.2 and B.4) due to the development of diarrhea (reducing the dose of the drug to 50 mg/day, as recommended in such cases in the instructions for use of Diaflex, was not provided for by the protocol), also 3 (20%) patients from this group noted a slight darkening of the urine (metabolites of the drug are predominantly excreted in the urine).
Conclusion
The results of the study indicate that long-term use of symptomatic slow-acting drugs (SYSADOA) - Diaflex and chondroitin sulfate sodium is an effective method of treating OA of the knee joints, taking into account their effect on pain and functional activity of patients. Since OA is essentially a non-lethal disease, various currently existing therapeutic methods (pharmacological and non-drug), which have minimal side effects with a high therapeutic index, can be considered as the most promising in these patients for long-term use. An analysis of the results of a 12-month use of Diaflex and chondroitin sulfate sodium in patients with knee OA showed their effectiveness in relieving the clinical symptoms of the disease (pain, stiffness, limitation of movements) against the background of discontinuation of NSAIDs and a reduction in the dose (or complete withdrawal) of paracetamol. However, taking into account the data of the study, the use of Diaflex may be preferable in patients with OA of the knee joint due to a more rapid increase in the clinical effect, as well as in patients with polyosteoarthritis with developing Heberden nodes due to the good analgesic effectiveness of the drug against small hand joints. Taking Diaflex in the examined patients was accompanied by a positive clinical effect after 2–3 weeks. from the start of taking the drug and increased throughout the entire treatment period. So, already by the 4th week. The patients showed positive dynamics of all clinical symptoms studied: the severity of pain, including starting pain, stiffness, and joint function. The presented results are consistent with literature data indicating that diacerein significantly improves the symptoms of the disease compared to placebo, has a pronounced aftereffect and does not cause severe adverse events, and therefore it is recommended as a drug for long-term therapy of OA [12].
conclusions
1. The use of symptomatic slow-acting drugs - Diaflex and chondroitin sulfate sodium in patients with OA of the knee joints has demonstrated high clinical effectiveness, safety, good tolerability, and a rare occurrence of adverse reactions. 2. Diaflex demonstrated a faster (after 2–4 weeks) clinical effect on OA symptoms, including those affecting small joints of the hands, which is probably due to the peculiarities of the drug’s mechanism of action. 3. Prescribing drugs from the SYSADOA group allows minimizing the development of side effects in comorbid patients by reducing the dose (duration of prescription) of NSAIDs and other drugs. 4. Therapeutic courses lasting 6 months are more preferable. or more, and the presence of an aftereffect in these drugs allows for course therapy for OA. 5. A more pronounced aftereffect was observed when using Diaflex, which confirms the increase in the positive dynamics of the WOMAC index even after the end of the 12-month course of therapy. We associate the results obtained with the mechanism of action of diacerein.