“The condom broke, I’m very afraid that I got pregnant. What to do?" — women’s forums were filled with such questions just a few years ago.
Today, many people know about the emergency contraception method, which will help avoid unwanted pregnancy if used within 1-3 days after the incident. Such measures include hormonal drugs including antigestagens and gestagens, as well as the introduction of an intrauterine device into the vagina.
However, there is one “but”: since emergency contraceptives can have a negative impact on health, doctors do not recommend using them yourself. It is recommended to consult a gynecologist, who will take into account your health condition and individual characteristics of the body before prescribing the drug.
There may be another reason to visit a doctor: with unprotected contact, there is a high risk of contracting sexually transmitted infections. Completing special tests will eliminate this possibility. At the Best Clinic multidisciplinary medical center, you can see a specialized doctor every day to get competent advice on your issue.
In what cases is emergency contraception acceptable?
Under no circumstances should you resort to emergency contraception all the time. Whatever the situation, we are talking about a powerful drug. However, you can use the “magic pill” once only if you have received the approval of your gynecologist. Situations in which the drug may be taken may be as follows:
- in case of complete rape, when the victim wants to get rid of any reminders of the event;
- in case of unprotected sexual intercourse, if pregnancy is not part of your immediate plans;
- in case of improper interruption of sexual intercourse, when sperm enters the vagina;
- if the condom is damaged or slips off the penis during sex.
Attention! You can take emergency contraceptives a maximum of 1-2 times a year, but it is better to do it much less often.
Pain and other problems with sex after childbirth
When resuming sexual activity after childbirth, a woman may encounter the following problems:
Vaginal dryness
After childbirth, most women, especially those who are breastfeeding, experience a sharp decrease in the level of female sex hormones - estrogens. As a result, the amount of natural vaginal lubrication produced decreases. For this reason, sexual intercourse can be uncomfortable and even painful for a woman. In this case, you should stock up on special lubricant in advance, which can be bought at any pharmacy. You just need to carefully monitor the composition of these lubricants and not use those that contain hormones if a woman is breastfeeding.
Pain during sexual intercourse
Pain during sexual intercourse may also be associated with the presence of sutures and scars on the perineum and vaginal walls; sometimes, due to sutures, the configuration of the vagina may change. Pain may also be observed in the area of the scar on the anterior abdominal wall after a cesarean section. Any suture during healing can cause some discomfort. This is due to changes in the sensitivity of the injured when the nerve endings are cut or ruptured. To avoid or eliminate pain in the suture area, during sexual intercourse you need to choose a position in which minimal pressure is applied to the scar. As the nerve endings adapt, over time, the discomfort in the suture area will pass. You can consult with your gynecologist, who will recommend local medications to speed up tissue restoration in the scar area. These drugs can also be used by nursing mothers.
Changes in vaginal muscle tone
Changes in the tone of the vaginal muscles can leave their mark on the sensations during the first sexual intercourse. However, the weakening of muscle tone and vaginal enlargement is temporary and this problem will go away within a few months, especially if the woman can find a few minutes a day to perform Kegel exercises. Kegel exercises involve contracting the pelvic muscles that support the vagina. These muscles contract when a woman stops urinating or tightens her vagina. During the exercises, the muscles contract strongly for one or two seconds, then relax; To achieve the effect, it must be repeated several times a day for 5-30 contractions. Ideally, it is better to practice such exercises during pregnancy: the woman will come to childbirth more prepared, and after the birth of the baby, the muscles will tone up faster.
Breast problems
Some problems during sex after childbirth may arise with the breasts. Firstly, touching the nipples of the mammary glands can be unpleasant and sometimes even painful. Secondly, during orgasm, due to the release of the hormone oxytocin, milk is released from the nipples. To avoid this, it is best to choose a time about an hour after feeding the baby, then the possibility of milk appearing from the breast is the least, but if this still cannot be avoided, it is worth having a towel on hand.
It must also be said that many women after childbirth do not experience any problems with sex - on the contrary, they say that the attraction to their husband has become stronger and the orgasm is brighter.
Hormonal emergency contraception
As emergency hormonal drugs, drugs of different generations can be used: from long-used to the latest tablets. Each product has its own recommendations for use and is designed for a certain period after sexual intercourse, during which you can drink it. As a rule, this period is 72–96 hours, although there are also drugs with a longer period of administration.
The action of these drugs is aimed at reducing progesterone, the pregnancy hormone. Due to its deficiency, the capillaries of the placenta are destroyed. The walls of the uterus lose their ability to hold the fertilized egg, which causes its evacuation. After taking the pills, menstrual irregularities and heavy bleeding may occur.
If you have resorted to emergency contraception, contacting a gynecologist is mandatory in any case. Before the next scheduled period, or if there is no menstruation while taking the pills, you should visit the clinic. Attention! In case of pain and excessive blood loss, this must be done urgently!
Unwanted pregnancy remains a serious problem for women. An alternative to terminating pregnancy is to prevent it. To prevent unwanted pregnancy, there are many methods of contraception, including emergency ones.
Emergency contraception was first used as a means of preventing unwanted pregnancies among rape victims in the mid-1960s. Since then, the range of indications for its use has expanded, and emergency contraception is recommended for women who are at risk of pregnancy as a result of unprotected sex (when no contraceptive method was used or when protection has failed, such as when a condom breaks). An emergency contraception method is considered acceptable if it can be used within a few days after unprotected sexual intercourse.
Despite its important role in preventing pregnancy, emergency contraception is not widely used, due to a lack of information about this method among women and sometimes among doctors.
As already stated, emergency contraception should be recommended as an emergency measure to protect against unwanted pregnancy in women who have been raped; if there are doubts about the effectiveness of contraception (displacement of the diaphragm during sexual intercourse, etc.); during expulsion of intrauterine devices (IUD); if you miss taking oral contraceptives; in cases where the planned methods of contraception cannot be used for some reason. Patients who are rarely sexually active and in whom an unwanted pregnancy may occur after sexual intercourse without the use of contraceptives also need to be prescribed postcoital contraception [2, 3].
The mechanism of action of emergency hormonal contraception is to suppress or delay the ovulation process, disrupt the fertilization process, transport the fertilized egg and its implantation.
The risk of pregnancy after unprotected intercourse ranges from 0 to 26% throughout the entire menstrual cycle and from 7 to 30% during the peri- or ovulatory period of the menstrual cycle [7]. Considering that the viability of sperm in a woman’s reproductive tract lasts from 3 to 7 days, and that of an unfertilized egg for 24–72 hours, it is advisable to carry out emergency contraception in the first three days after sexual intercourse [7].
For emergency hormonal contraception, mainly estrogen-gestagen and gestagen-containing drugs are used.
Until recently, one of the common methods of emergency contraception was the use of increased doses of oral contraceptives - the so-called Yuzpe method (named after the Canadian doctor who first used it). The method consists of twice using 200 mcg of ethinyl estradiol and 1 mg of levonorgestrel within 72 hours after sexual intercourse, with a break of 12 hours. The advantage of this method is that for the purpose of emergency contraception, you can use any combined contraceptives, including low-dose ones, while the number of tablets varies depending on their composition and doses of hormones. However, it has been proven that the effectiveness of this method is reduced if unprotected intercourse occurs immediately before ovulation. In addition, the incidence of side effects such as headaches, nausea, vomiting, and menstrual dysfunction occurred in 21.3% of cases, i.e., in almost every fourth patient [1, 3].
Contraindications to the use of the Yuzpe method are determined mainly by the presence of an estrogen component in the tablets. These include a history of thrombolism, severe liver disease, breast and endometrial cancer. Its use is also undesirable for women over 35 years of age, heavy smokers (more than 15 cigarettes per day), as well as women who have been subjected to sexual violence, against which complications often develop.
Currently, one of the most common effective and affordable methods of emergency contraception is the use of gestagens. The most commonly used testosterone derivatives are divided into levonorgestrel and norethisterone derivatives. Their chemical structure is close to natural progesterone. From this group of drugs, the Hungarian drug Postinor is widely known in our country, containing 0.75 mg of levonorgestrel in one tablet, which is recommended for use according to the following scheme: one tablet no later than 72 hours after sexual intercourse, another one 12 hours after the first.
Levonorgestrel is a synthetic compound, structurally similar to norethisterone, binds strongly and selectively to progesterone receptors and exhibits biological activity without any preliminary transformations. This is the most active substance in the series of 19-norsteroids. Levonorgestrel has the longest half-life because it does not have a first-pass effect through the liver, which makes its biological activity maximum.
Levonorgestrel has no estrogenic effect and has a slight androgenic effect on the woman's body. It is characterized by the greatest affinity for progesterone receptors, which explains such a pronounced progestational effect of levonorgestrel, in particular on the endometrium.
Gestagens suppress the mitotic activity of endometrial cells, initiate their early secretory activity, and cause early secretory transformation of the endometrium, which prevents the implantation of a fertilized cell. In addition, gestagens help reduce contractile activity and the threshold of excitability of muscle cells, which explains one of the mechanisms of emergency contraception - disruption of egg transport. Gestagens have an inhibitory effect on the secretion of gonadotropic hormones and, as a result, prevent ovulation.
In 1998, a randomized controlled trial of levonorgestrel versus the Yuzpe method was conducted under the auspices of WHO. 1998 healthy women with a regular menstrual cycle were examined in 21 centers in different countries: 997 of them were prescribed the Yuzpe method, 1001 - levonorgestrel. The analysis of the study results was carried out based on data from 979 women who used the Yuze method according to the standard method, and 976 who received 0.75 mg of levonorgestrel no later than 72 hours after unprotected intercourse with a repeat dose after 12 hours. The effectiveness of levonorgestrel was higher than that of the Yuzpe method - 98.9 and 96.8%, respectively. In terms of tolerability, levonorgestrel was also superior to the Yuzpe method: nausea was observed in 23.4 and 50.5% of women, respectively, vomiting in 5.6 and 18.8%, dizziness in 11.2 and 16.7%, fatigue in 16 .9 and 28.5% (the differences are statistically significant). Differences in the incidence of other side effects (headache, mastalgia, lower abdominal pain, intermenstrual bleeding) were not statistically significant. Thus, the efficacy of levonorgestrel was higher and the tolerability was better than that of the Yuzpe method.
According to the authors of the study, this is due to the peculiarities of the interaction of estrogens and gestagens, as well as a lower dose of levonorgestrel when using the Yuzpe method. The following conclusion was drawn: the Yuzpe method can be replaced by the use of levonorgestrel, which is more effective and has a lower incidence of side effects. Severe menstrual irregularities with the use of levonorgestrel, which were previously noted in other studies, were not observed in this study [4, 8, 11].
Given the increased interest in emergency contraception methods, which is explained by a number of biological and social factors (early puberty, early onset of sexual activity), the development of effective methods and regimens for taking hormonal drugs has continued in recent years. In mid-1998, a large multicenter, randomized, double-blind study was initiated to compare the efficacy and side effects of 10 mg mifepristone and two regimens of levonorgestrel (0.75 mg twice or 1.5 mg once) for emergency contraception within 120 hours of unprotected use. sexual intercourse. Based on the studies conducted, a new regimen of levonorgestrel was developed - 1.5 mg once [18, 19].
This became the basis for the creation of the drug Escapelle, containing 1.5 mg of levonorgestrel in one tablet, which provides an excellent contraceptive effect and provides greater reliability in preventing pregnancy. Escapelle can be effectively used as a first-choice drug for emergency contraception as an alternative to abortion. Currently, Escapelle has appeared in Russia.
The effectiveness and safety of a single dose of 1.5 mg of levonorgestrel, the dose contained in Escapelle, was confirmed by the results of a WHO study in which more than 4,000 women from 14 countries took part. The Emergency Contraception Consortium recommends this regimen as the first choice [17–19].
If the recommended dosage regimen is followed, levonorgestrel does not significantly affect blood clotting factors, fat and carbohydrate metabolism [16]. When taken orally, it is quickly and completely absorbed from the gastrointestinal tract. The maximum concentration of levonorgestrel in the blood serum after taking 1 tablet of Escapel is achieved after 2 hours. At the recommended dose, levonorgestrel causes inhibition of ovulation if sexual intercourse occurs in the preovulatory phase of menstruation. In addition, the drug-induced regression of endometrial proliferation prevents blastocyst implantation. The effectiveness of contraception decreases as the time elapses between sexual intercourse and taking the drug increases.
If the time of sexual intercourse is unknown or more than 96 hours have passed since unprotected sexual intercourse, the likelihood of pregnancy is high. If menstruation is delayed by more than 7 days, as well as when menstruation that occurs on time is unusual or pregnancy is suspected for some other reason, a gynecological examination should be performed to exclude pregnancy.
If vomiting occurs within 3 hours after taking the Escapel tablet, the effectiveness of the drug is reduced, in which case barrier contraceptives (for example, a condom) should be used until the next menstruation. Repeated use of Escapella tablets during the same menstrual cycle should be avoided to avoid cycle disturbances.
In women with a history of ectopic pregnancy or pelvic inflammatory disease, the use of levonorgestrel may serve as an additional risk factor for ectopic pregnancy. The latter should be excluded if there is pain in the lower abdomen, fainting and the above-mentioned anamnestic data. The use of Escapel, as a rule, does not interfere with the regularity and nature of menstruation. In cases where this drug was used due to an error in regular hormonal contraception and subsequent
There is a 7-day break, there is no menstruation, pregnancy should be excluded. It must be remembered that emergency contraception does not protect against sexually transmitted diseases.
Thus, it should be emphasized that emergency contraception is a one-time measure aimed at preventing unplanned pregnancy. Emergency contraception cannot be recommended for chronic use. However, in certain situations, emergency contraception is the only option to prevent unwanted pregnancy and is an alternative to abortion.
Contraindications to hormonal emergency contraception
You cannot use emergency contraception with specialized medications if you have:
- severe liver damage;
- uterine bleeding in earlier periods;
- migraines, attacks of severe uncontrollable headaches;
- if you exceed the age threshold of 35 years;
- long history of active smoking.
Taking emergency contraception has a number of possible side effects. These include dizziness, nausea and vomiting, pain in the mammary glands, head, lower abdomen, menstrual irregularities, and thrombosis. It is noted that all side effects should disappear within the first two days after taking the drug. Be that as it may, emergency contraception should only be used in rare cases of force majeure.
When can you start having sex after childbirth?
In the first 6-8 weeks after childbirth, gynecologists do not recommend having sex. This is due to the fact that the body is recovering at this time after 9 months of pregnancy. Immediately after the end of the third stage of labor, that is, the birth of the placenta, the early postpartum period begins. It continues for 2 hours. Then comes the late postpartum period. This period lasts 6-8 weeks. During this time, there is a reverse development (involution) of all organs and systems that have undergone changes in connection with pregnancy and childbirth. The exception is the mammary glands, the function of which reaches its peak in the postpartum period.
The most pronounced involutional changes occur in the genital organs, especially in the uterus. The rate of involutional changes is most pronounced in the first 8-12 days. The uterus and cervix are significantly reduced in size. After the birth of the placenta, a large wound surface remains in the uterus, which takes approximately 4-6 weeks to heal. During this period, the placental area in the uterus bleeds, spotting - lochia - is bloody in nature in the first days, gradually its color changes from red to reddish-brown, brownish, by the 4th week the discharge almost stops and soon disappears completely. Sexual contact at this time can facilitate the penetration of infection through the slightly open cervix into the uterus; blood and an open wound surface will only contribute to the rapid progression of inflammation.
After vaginal birth, complications can often occur in the form of incisions or tears in the perineum, vaginal walls or cervix. It also takes time for stitches to heal after childbirth. Even if there were no ruptures during childbirth, the tone of the muscles of the vagina and perineum after natural childbirth is significantly reduced. The process of reverse development of the vaginal muscles depends on the tone of these muscles before pregnancy, on whether the woman trained them during pregnancy, on age, and genetic characteristics.
In patients who have undergone a planned cesarean section, there are no changes in the vaginal walls, but restoration of the size of the uterus occurs more slowly. In addition, it takes time for healing and the formation of a full-fledged scar on the anterior abdominal wall. This takes about a month on average.
So, 6-8 weeks after birth, it is recommended to visit a gynecologist
who will examine the condition of the uterus, cervix, sutures on the perineum or vaginal walls, a scar on the abdominal wall after a cesarean section, take a smear on the flora to identify signs of inflammation, and then give the go-ahead to resume intimate relationships.
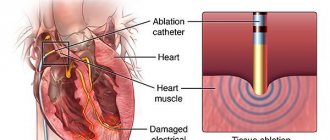
Emergency intrauterine contraception
The technology is based on the introduction of a special intrauterine device into the vaginal cavity in the first 5–7 days after sexual intercourse, during which there is a risk of unplanned pregnancy. The spiral blocks the implantation of a fertilized egg, while being more effective than the previous method.
However, this means of emergency contraception cannot be used if we are talking about a young nulliparous woman. In addition, there are a number of contraindications to its use, which a qualified doctor can recognize.
If you have unplanned sexual contact without the proper level of protection, contacting a specialist is the only correct option. Call Best Clinic Medical Center to make an appointment. Or create an online request for a call back from the operator by filling out a special form on the website.