Mediastinitis is a disease characterized by inflammation in the mediastinal organs, resulting in compression of blood vessels and nerves. In practical medicine, any inflammation that leads to mediastinal syndrome is called mediastinitis.
- Classification
- Causes
- Pathogenesis
- Symptoms
- Diagnostics
- Treatment
The inflammatory process is generalized due to the following conditions:
- constant volumetric and spatial movements of loose fiber
- absence of fascial barriers
According to the anatomical structure of the mediastinum, mediastinitis is divided into anterior and posterior. Each of these types can be:
- top
- median
- total
- lower
According to the course, the disease is divided into acute and chronic. Aseptic mediastinitis, which is caused mainly by nonspecific or specific microflora, is rarely recorded. It can enter in various ways, mainly through trauma to the esophagus due to diverticulum rupture, chemical burns, etc. Less commonly, the spread occurs along the fascial sheets from the neck or from adjacent tissues.
Classification
Depending on the location of the inflammation of the mediastinal tissue, mediastinitis is divided into:
- front upper
- rear lower
- rear upper
- total rear
- total front
- front upper
It is rare that the anterior and posterior mediastinum are affected simultaneously, because before this form develops, a person dies from intoxication and septic shock. The stages of development of mediastinitis, depending on the clinic, are as follows:
- serous
- purulent
Most often, mediastinal phlegmon is diagnosed, in which the mortality rate reaches from 25 to 45%. If the causative agent is anaerobic flora, then the mortality rate reaches 68-80%. A more favorable form of mediastinitis is considered to be a mediastinal abscess. With this diagnosis, there are 15-18 deaths per 100 cases.
Depending on the location of the primary source of infection, there are primary and secondary mediastinitis. The disease is considered primary if the mediastinal tissue is initially infected.
Causes
The two most common causes are median sternotomy and esophageal rupture. Esophageal rupture may be a complication of placement of a Sengstaken-Blackmore tube or Minnesota tube, as well as a complication of esophagoscopy. Also occurs with vomiting (Berhaave syndrome). Mediastinitis in 1% of cases is a complication of median sternotomy.
Chronic fibrosing mediastinitis is caused by histoplasmosis or tuberculosis, but can occur with silicosis, sarcoidosis, and fungal infections. An intense fibrotic process is typical, which leads to compression of the mediastinal structures, which can cause tracheal stenosis, superior vena cava syndrome, etc.
The cause of primary posterior mediastinitis in most cases is mechanical damage to the thoracic esophagus by foreign bodies or instruments. Causes of iatrogenic esophageal injuries may include bougienage of esophageal strictures, fibroesophagoscopy, insertion of a probe, and cardiac dilatation. In 1-2% of cases, the cause of posterior purulent mediastinitis is necrosis of the esophageal wall due to chemical burns. The cause of this form may be a spontaneous rupture of the esophagus, when, as a result of gagging or minor physical activity, a longitudinal rupture of the left wall of the esophagus is formed in the supradiaphragmatic region. Such cases are almost never diagnosed early. The reflux of stomach contents into the pleural cavity in a short time causes pleural empyema and sepsis. The mortality rate is very high, reaching from 60 to 90%.
Surgeons most often record secondary posterior mediastinitis, which is formed as a result of the spread of a purulent process from the cellular spaces of the neck. The reason is mechanical and chemical damage to the pharynx and cervical esophagus.
Possible causes of secondary posterior mediastinitis:
- odontogenic phlegmon of the floor of the mouth and submandibular spaces
- cervical adenophlegmon
- retropharyngeal abscess
- tonsillogenic phlegmon of the peripharyngeal space
Secondary posterior purulent mediastinitis develops with the participation of non-clostridial anagrobes, which settle in the gingival pockets, oral cavity and tonsil crypts. Primary anterior mediastinitis is a consequence of infection of the anterior mediastinum after sternotomy in patients with cancer or cardiac surgery, and in rare cases with a closed sternum injury, when chest fractures suppurate. The causative agents of the purulent process are gram-positive cocci (most cases), epidermal or Staphylococcus aureus.
Secondary anterior mediastinitis is caused by the spread of tonsillogenic, odontogenic phlegmon of the neck. In some cases, it is a consequence of suppuration of the soft tissues of the anterior chest wall on the anterior mediastinum. Factors that contribute to the development of the process are instability of the sternum with suppuration of the superficial layers of the wound. With inadequate drainage, wound discharge may accumulate in the anterior mediastinum, which also plays an important role in pathogenesis. Risk factors for the development of anterior mediastinitis after cardiac surgery:
- diabetes
- obesity
- use of bilateral mammary coronary bypass surgery
- long-term surgery under artificial circulation
It is generally accepted that purulent inflammation of the mediastinal tissue was first described by K. Galen [14]. In a young man with an anterior mediastinal abscess and chest wall fistula, he removed fragments of the sternum and part of the pericardium involved in the process. The postoperative wound healed successfully.
However, upon careful study of the works of A.K. Celsus [53], who lived 100 years before C. Galen, in the chapter on the signs of approaching death, we found a description of the clinical picture, which in modern language can be interpreted as odontogenic purulent mediastinitis.
Abu Ali ibn Sina [4] introduced the term, which was translated from Arabic into Latin as Inflammatio velaminis, and established that the severity of the condition and prognosis depend on the location of the “putrefactive tumor”. The term “mediastinitis” appeared in the literature in the 12th century thanks to the works of Ibn Zor, who himself suffered from this disease and recorded its clinical signs [Cit. according to 22].
All these observations concerned anterior mediastinitis, which is explained by the tendency of abscesses of this localization to break out independently and easy accessibility for emptying by trephination of the sternum.
In the Middle Ages and up to the 18th century, individual casuistic observations were described. In 1786, G. Gumet’s book “The Initial Foundations of Medical Science in the City of St. Peter” [19] appeared in Russia, where in the section “On thoracic puncture” there is a description of the inflammation of the “mid-thoracic obstruction.” A more detailed work in this area belongs to I. Bush [10], who in 1807 outlined the technique of trephination of the sternum. In subsequent years [63, 68, 79, 83], individual reports on clinical observations of anterior purulent mediastinitis were published.
An important stage in the history of mediastinitis surgery was the works of N.I. Pirogov [35], in which he cited observations of posterior mediastinitis after gunshot wounds of the esophagus and sharply criticized a certain Strohmeier, who denied the possibility of the purulent process spreading from the neck to the mediastinum. Highlighting a more benign form of mediastinitis - “abscess” (abscess) and a more dangerous one - “acute edema” (phlegmon), he pointed out the pattern of phlegmon spreading from the neck to the mediastinum and for the first time called this process “descending” (which corresponds to the modern terminology of foreign authors ).
At the same time, until the end of the 19th century, posterior purulent mediastinitis remained unstudied due to the anatomical features of this zone, which created great difficulties for surgical intervention without the help of painkillers. In 1895, the famous European surgeon G. Ziembicki [87] wrote: “Phlegmon of the posterior mediastinum is a dark spot in modern surgery.” This is confirmed by publications on fatal outcomes in the gangrenous form of posterior mediastinitis due to perforation of the esophagus [43, 44].
Progress in the surgical treatment of posterior purulent mediastinitis in these years is associated with the names of Russian surgeons. In 1888 I.I. Nasilov [30] published a short article in the journal “Vrach” in which he substantiated the possibility of posterior extrapleural access. In 1888, the text of this article appeared in the English press. Somewhat later, our foreign colleagues presented their observations of the use of this access, while some referred to the experience of I.I. Nasilova [73, 77, 81], while others do not, claiming authorship [65, 82]. Subsequently, access via I.I. Nasilova, despite its traumatic nature and the emergence of alternative developments, was used until the 60s of the 20th century [5, 78, 86].
A major step forward in the surgery of posterior mediastinitis was the development of a transcervical extrapleural approach, the author of which in Russia is considered to be V.I. Razumovsky, abroad - V. Hacker. IN AND. Razumovsky in 1897 successfully used anterior longitudinal collotomy to drain the posterior mediastinum in a 12-year-old boy with a gunshot wound. He published the surgical technique in 1899 [37]. In the same year, L. Heidenhain [74] published his observation of the use of a transverse approach in the neck. V. Hacker [73], speaking at the XXX Congress of German surgeons in 1901, reported on 3 observations known to him: V.I. Razumovsky, L. Heidenhain and his own.
However, it would be unfair to keep silent about the fact that 7 years before V.I. Razumovsky, in 1890, zemstvo surgeon V. Sheboldaev [55] successfully used longitudinal collotomy to drain the mediastinal abscess.
The first decades of the 20th century were devoted mainly to a detailed study of the anatomical formations of the mediastinum, cellular spaces and fascia, the ethnopathogenesis of various forms of purulent mediastinitis, and the ways of spread of putrefactive infection in odonto- and tonsillogenic phlegmons of the face and neck [6, 17, 51, 56].
Of great importance for understanding the ways of contact spread of odonto-, oto- and tonsillogenic phlegmons to the mediastinal tissue were the “Essays on Purulent Surgery” published in 1934 by V.F. Voino-Yasenetsky [13].
The greatest experience abroad in the 30s of the 20th century was H. Pearse [80], who published data on 64 observations of purulent mediastinitis with a mortality rate of 56.2%, as well as H. Killian [75].
The results of surgical treatment remained poor due to the ineffectiveness of drainage of narrow and upward canals using transcervical approaches. H. Lilienthal's proposal [76] to use an active drainage method with washing and aspiration did not gain popularity due to the imperfection of the equipment. According to [48], much later, in 1941, Frink published an observation of successful treatment of mediastinitis in a patient with spontaneous esophageal rupture by using aspiration through drainages of the mediastinum and pleural cavity. Another attempt to use the active drainage method was made by R. Adams [60]: in 1946, he used this method in 7 patients, all recovered, but this fact did not make an impression on the surgical community.
A major event in the first half of the 20th century in Russian surgery was the meeting of the Leningrad Society of Surgeons named after. N.I. Pirogov in 1926, in which G.F. Petrushevskaya [34] reported on the experience of using transcervical mediastinotomy in the treatment of posterior purulent mediastinitis, and V.L. Rokitsky [42] mentioned his use of a transperitoneal extrapleural approach to the posterior mediastinum in one case, without providing details.
The next stage in the development of methods for drainage of the posterior mediastinum was the work of A.G. Savinykh and B.S. Rozanova. A.G. Savinykh [46] developed in detail the method of transperitoneal sagittal diaphragmotomy for access to the lower parts of the posterior mediastinum for esophageal cancer, and B.S. Rozanov [39–41] modified this approach for drainage of the mediastinum with purulent mediastinitis, outlining the successful experience of many years of use in his monograph, which has not lost its relevance in the 21st century.
During the Great Patriotic War, the attention of surgeons was focused on the treatment of mediastinitis of gunshot origin [12, 16, 18, 23, 26, 31, 45]. In 1947 in Tomsk, at the V Plenum of the Academic Council of the Ministry of Health of the RSFSR, A.A. made reports on the main provisions of the treatment of acute purulent mediastinitis. Vishnevsky [12] and A.A. Gehrke [15].
Progress in the diagnosis of mediastinitis, starting from the first reports by O. Dehn [69], was facilitated by research into the capabilities of the x-ray method [20, 38].
In connection with the development of planned thoracic surgery in the 50s of the 20th century, the first publications appeared on the diagnosis and treatment of posterior purulent mediastinitis, which arose due to the failure of the sutures of the esophageal-gastric anastomoses [8]. At the same time, publications were published about secondary forms of mediastinitis developing with tuberculosis, tularemia, influenza, and erysipelas. The diagnosis in such cases was rarely made antemortem, and the therapeutic guidelines of that time [54] listed such signs of mediastinitis as the appearance of hyperemia and fistulas on the anterior chest wall.
In 1954, in the doctoral dissertation of A.Ya. Ivanov [22] was the first to comprehensively study the problem of purulent mediastinitis of various origins, localization and clinical course. He published the main provisions of this work in the form of a monograph [21]. In 1960, the manual of B.V. was published. Petrovsky “Surgery of the mediastinum” [33], where a separate section was devoted to purulent mediastinitis.
In the last quarter of the 20th century, the number of studies of anterior postoperative mediastinitis sharply increased due to the rapid development of cardiac surgery, which is accompanied by a high level of purulent complications [9, 28, 62]. Russian and foreign authors sound the alarm in their publications: according to [49], mortality in anterior mediastinitis reached 54.8%, according to [84] - 52%. At the same time, the not very correct term “sternomediastinitis” appeared [70]. The most fundamental work of those years on the problem under study is considered to be the manual edited by T. Salm [85].
Regarding the history of surgery for mediastinitis in Russia, one cannot fail to note the role of researchers from the Research Institute of Emergency Medicine named after. N.V. Sklifosovsky. The pioneer in the study of this problem, starting in the 30s, was B.S. Rozanov [39-41]. In the 50s, the works of E.N. became widely known. Popova [36] and M.K. Shcherbatenko [57]. The next stage in the development of surgery for purulent mediastinitis is associated with N.N. Kanshin [24, 25], who in 1971 developed, on a fundamentally new basis, a method of active drainage of the mediastinum using flow-fractional lavage with long-term aspiration.
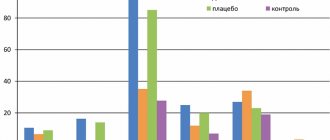
In the 70s, in Russia and throughout the world, the number of observations of purulent mediastinitis due to iatrogenic damage to the esophagus, associated with the widespread introduction of instrumental diagnostic and therapeutic technologies, increased sharply. During these years at the Research Institute named after. N.V. Sklifosovsky surgeons, together with specialists in maxillofacial surgery, otorhinolaryngologists, immunologists and resuscitators, developed a program for early diagnosis and surgical treatment of mediastinitis using complex intensive care, based on the experience of treating more than 500 patients with traumatic, odonto-, tonsillogenic and postoperative mediastinitis. This reduced overall mortality from 33% in 1976 to 11% in 1986 [3]. Progress in the early diagnosis of mediastinitis is associated with the introduction of X-ray computed tomography into practice [66, 67, 71]. In Russia, the results of a study of CT semiotics of various forms of purulent mediastinitis were published in 2001 [1].
However, in the 1990s the number of late admissions increased sharply. Against the backdrop of a decrease in the general immune background of the population due to the socio-economic catastrophe and the lack of opportunity in hospitals to use expensive drugs and treatment methods, mortality in purulent mediastinitis increased almost 2 times and in 2000 amounted to 18.9% [3].
In the first and second decades of the 21st century, there were no significant breakthroughs in methods of diagnosis and treatment of purulent mediastinitis. In Russia, with odonto- and tonsillogenic mediastinitis, it remains at the level of 27.5-54.5% [11, 52, 54], with perforation of the esophagus - 20.2% [32] and with anterior postoperative mediastinitis - 8.3% [ 27].
According to the European Association of Cardiothoracic Surgeons (2017), overall mortality in purulent mediastinitis continues to remain high - from 10 to 47%, depending on the form of mediastinitis [59, 64, 72]. Against this background, the International Classification of Diseases, 10th revision (ICD-10), is paradoxical, where the concepts of “mediastinitis” and “mediastinal phlegmon” are absent. A rarer and milder form of the disease is mentioned - mediastinal abscess (J 85.3), in which the mortality rate is several times lower than with putrefactive-necrotic phlegmon of the mediastinum.
Thus, completing the historical review of the difficult and unresolved problem of mediastinitis surgery, it should be concluded that significant obstacles to progress are the disunity of doctors of various specialties involved in the diagnosis and treatment of mediastinitis, the lack of uniform approaches to methods of surgical treatment, immune and antibacterial therapy, as well as the lack in some cases of economic opportunities to provide this therapy.
The author declares no conflict of interest.
The author declare no conflict of interest.
Information about authors
Abakaumov M.M.
- Doctor of Medical Sciences; prof.; https://orcid.org/0000-0001-6112-9404
Pathogenesis
After the moment of infection, the mediastinal tissue swells 4-6 hours later, which is called serous meningitis. The swelling spreads to the neck, subglottic area, epiglottis, etc. The person’s voice becomes hoarse, it becomes difficult to breathe, and the process of swallowing becomes difficult. Swelling of the mediastinal tissue causes increasing pain in the interscapular region and behind the sternum. Breathing becomes frequent and shallow, the body lacks oxygen. Blood flow to the right side of the heart becomes more difficult, central venous pressure increases, stroke volume and pulse arterial pressure decrease.
Body temperature reaches subfebrile values, hyperleukocytosis with a shift of the leukocyte formula to the left, and compensated metabolic acidosis are recorded. The content of carbohydrates, protein and electrolytes in the blood plasma remains almost unchanged. In case of perforation of the esophagus, coccal microflora, the presence of cicatricial changes in the mediastinal tissue after previously suffering post-burn esophagitis, the stage of serous inflammation can last 2-4 days. When the purulent process spreads to the unchanged tissue of the posterior mediastinum, after 6-8 hours morphological signs of phlegmonous inflammation appear.
With purulent mediastinitis, at the stage of generalization of the process, decompensated metabolic acidosis develops, and all parts of the immune system are suppressed. Severe disturbances of central hemodynamics accompany ARDS and progression of respiratory failure. After 3-4 days, the process spreads to the pleural cavities and the pericardial cavity, intoxication becomes very strong, maximum. Heart rhythm disturbances are typical at this stage of the disease. A person takes from 28 to 30 inhalations per minute, the temperature is 38.5-39 ° C. Consciousness is preserved, but the patient is noted to be lethargic.
A poor prognosis is indicated by such signs as sudden changes in CBS and severe lymphopenia (below 5%). The concentration of creatinine and urea increases, with hypoproteinemia and oliguria. If treatment is not started, death occurs within 1-3 days.
Symptoms
Symptoms of mediastinitis depend on the underlying process and the level of compression. There are also common manifestations that are caused by occlusion of the superior vena cava and innominate vein:
- feeling of heaviness and pain in the chest and back
- dizziness
- dyspnea
- headache
- neck thickening
- dysphagia
- puffiness of the face
- hoarseness of voice
- blueness of the hands, neck and face
- nosebleeds
- bradycardia
- asymmetry of the chest, etc.
When the esophagus ruptures, the disease begins acutely, starting with severe chest pain and shortness of breath, which are caused by infection and inflammation in the mediastinum.
Acute mediastinitis
Characterized by a sudden onset and rapid development. The patient's condition quickly deteriorates as intoxication syndrome forms and develops. The manifestations of this form depend on the nature and localization of mediastinitis, as well as on how involved the trachea, esophagus, sympathetic trunk, phrenic nerve, etc. are involved in the process. The following symptoms may be noted:
- suffocation
- dysphagia
- hoarseness of voice
- persistent cough
- hiccups
- arrhythmias
- Bernard-Turner syndrome
- intestinal paresis
Chronic mediastinitis
The disease is caused by proliferative processes in the mediastinum and a specific infection. For a long time there may be no manifestations at all. Later the following symptoms appear:
- cough
- pain in the side
- weakness
- dyspnea
- difficulty swallowing
- feeling of tightness in the chest
With proliferative and fibrous mediastinitis, signs of compression of the superior vena cava are revealed: puffiness of the face, swelling of the arm, cyanosis and dilation of the chest veins.
Kinds
According to the nature of the origin of the disease, the following are distinguished:
- Primary – caused by injury in the mediastinal organs;
- Secondary - caused by the penetration of infection into the mediastinum from other areas.
According to the clinical course of the disease, they are divided into:
Lightning;
- Spicy;
- Chronic.
According to the type of inflammation there are mediastinitis:
- Anaerobic;
- Putrid;
- Serous;
- Gangrenous;
- Tuberculosis.
The chronic type of mediastinitis can be caused by aseptic or microbial causes.
Aseptic:
- Rheumatic;
- Posthemorrhagic;
- Idiopathic;
- Adipose sclerotic.
Microbial:
- Specific;
- Nonspecific.
The disease is also distinguished by the type of localization.
Diagnostics
The high mortality rate is explained by the impossibility of early diagnosis, especially if the disease is secondary. The purulent process moves to the mediastinum. Complex instrumental examinations are carried out. A general X-ray of the chest is taken in at least two projections. Perforation of the esophagus manifests itself as follows: darkening in the posterior mediastinum in the lateral projection, the presence of air in the mediastinum, “sympathetic” pyopneumothorax.
A cavity with a horizontal fluid level is detected with a mediastinal abscess. Mediastinal emphysema can be especially extensive when the esophagus is ruptured during fibroesophagoscopy with air insufflation into the lumen of the esophagus. In some cases, a contrast study of the esophagus with a suspension of barium sulfate is relevant. Ultrasound is used extremely rarely in the diagnosis of mediastinitis. EFGS is carried out. If the method does not detect perforations, contrast radiography of the esophagus and mediastinography are performed. MRI is also valuable in establishing the diagnosis of mediastinitis.
In some cases, thoracoscopy, cavography, and bronchoscopy are relevant. Diagnosis of mediastinitis due to esophageal rupture is often based on an analysis of symptoms. CT scan detects air bubbles in the mediastinum in such cases.
Short description
Mediastinitis is a serous or purulent inflammation of the mediastinal tissue. Occurs with inflammatory diseases or perforations of the mediastinal organs; lymphadenitis with abscess formation, pleural empyema, lung abscess with perforation into the mediastinum. In recent years, mediastinitis caused by instrumental perforations of the esophagus, trachea, and bronchi has become more frequent. The infection can also enter the mediastinum indirectly (lymphogenous) due to inflammatory changes in neighboring organs: lungs, ribs, neck. The main localization of the inflammatory process is the upper mediastinum. The main etiological factors are instrumental perforations and the spread of odontogenic phlegmon of the neck to the mediastinal tissue.
Code according to the international classification of diseases ICD-10:
- J98 Other respiratory disorders
Symptoms, course . The course of the disease is severe. Mediastinitis as a complication of a number of diseases is manifested by a deterioration of the condition of an already existing severe pathology. When mediastinitis occurs against the background of odontogenic phlegmon of the neck, the patient develops chest pain, high fever, chills, and tachycardia. When examining the neck, a sharply painful inflammatory infiltrate is noted, reaching the collarbone. If the phlegmon of the neck was previously opened, then a significant discharge leaves the wounds, sometimes with an unpleasant putrefactive odor. When tapping the sternum, the pain intensifies. In the blood - high leukocytosis with a shift to the left. X-ray examination reveals an expansion of the mediastinal shadow. With instrumental perforation of the esophagus, damage to the pyriform sinus often occurs. Due to air insufflation at the time of examination, the infection quickly spreads through the mediastinum. Signs of intoxication appear very early and progress rapidly. Often, immediately after the examination, subcutaneous crepitus in the neck, pain behind the sternum with radiation to the neck and interscapular space are noted. After a few hours, the temperature rises significantly, chills, profuse sweating, tachycardia appear, and there may be clinical manifestations of septic shock. In the blood - high leukocytosis with a shift to the left. X-ray - widening of the mediastinal shadow, emphysema of the mediastinal tissue, neck. When contrasting the esophagus (water-soluble contrast agents only), it is possible to identify the location and size of the perforation, but with microperforation, it is difficult to detect the flow of contrast beyond the esophagus.
Treatment
The purulent form of the pathology in question is treated with antibiotics. They are generally inclined towards de-escalation intravenous therapy with carbapenems for 7-10 days. At the same time, in case of a sutured rupture of the esophagus, in case of odontogenic, tonsillogenic infection, determining the sensitivity of the isolated microflora to antibiotics allows, in some cases, the effective use of cheaper drugs (IV generation cephalosporins, fluoroquinolones) in combination with metronidazole. This regimen gives the desired therapeutic effect if the causative agent is also coccal flora, which is typical for the postoperative anterior form of mediastinitis.
Detoxification therapy is carried out according to the same principles as for acute purulent diseases. Mediastinitis with rupture of the esophagus is treated with antibiotics administered parenterally. You can use clindamycin, which is administered intravenously every six hours at a dose of 450 mg, it is combined with ceftriaxone (2 g once a day for at least 2 weeks). In many cases, treatment requires an emergency revision of the mediastinum with primary suturing of the esophageal rupture and drainage of the pleural cavity and mediastinum.
Surgical treatment
The surgical method is the leading one in the treatment of purulent mediastinitis, since this is how complete drainage of the purulent focus is carried out. Access to the mediastinum is divided into extrapleural and transpleural. The first is resorted to in case of severe concomitant diseases, elderly patients, etc. Extrapleural approaches to the posterior mediastinum are combined with postoperative washing of the purulent focus with antiseptic solutions with aspiration of the contents in a vacuum mode in a system of the order of 10-40 cm of water. Art.
If the infected contents enter the posterior mediastinum through a defect in the pharynx, cervical, upper thoracic esophagus, then an additional drainage tube is installed with the end at the level of the perforation. The second option is suturing the defect. If gastric contents enter the mediastinum through a defect in the lower thoracic esophagus, the defect is also sutured.
Postoperative treatment
If the treatment is as intensive as possible, the treatment is successful in many cases. If this is the case, individual components of complex treatment are gradually abolished, which become irrelevant when laboratory, clinical, and instrumental manifestations return to normal.
Complex intensive treatment of mediastinitis:
- taking antibacterial drugs
- local effect on the source of purulent infection
- detoxification treatment
- immunocorrective therapy
- replenishment of the body's energy costs
Local treatment includes constant washing of the purulent focus in the mediastinum with an antiseptic solution while simultaneously using aspiration with a vacuum of about 10-40 cm of water. Art. After the cavity has collapsed and turned into a channel around the drains, the drains gradually begin to tighten and are eventually removed, replacing them with rubber outlets for several days.
If mediastinitis is a consequence of tuberculosis, appropriate anti-tuberculosis therapy is prescribed. If therapy fails, vascular stents can be installed to limit compression of some central vessels.