2018-01-09
- Source
- Manifestations
- Complications
- Vaccines
Chickenpox (varicella, chickenpox) is an acute and highly contagious disease. It is caused by a primary infection with the varicella zoster virus. Varicella outbreaks occur throughout the world and, in the absence of a vaccination program, affect a large proportion of the population by mid-life.
When did chickenpox start?
Chickenpox has been known since ancient times. For some time it was considered a mild form of smallpox, and only in 1772 was it identified as a separate disease. And in 1909, it was found that chickenpox and shingles have the same pathogen, which was later confirmed by laboratory tests. Subsequent study of the virus led to the development of a live attenuated varicella vaccine in Japan in the 1970s. The vaccine was licensed for use in the United States in March 1995.
Treatment
Treatment of chickenpox mainly involves preventing bacterial complications. To prevent the spread of the virus, careful hygiene must be observed, including showering daily and trimming young children's nails (to prevent scratching and breaking up the rash blisters).
The use of antiviral agents during treatment, such as acyclovir, is only justified for premature infants, patients with compromised immune systems and adults (due to the greater severity of the infection). The traditional means of “treating” chickenpox – “brilliant” – is not any effective remedy; baths and trays with a small addition of soda, antihistamines and pain-relieving ointments to relieve itching are much more effective.
What causes chickenpox and how can you get infected?
Varicella zoster virus (VZV) is a virus that causes chickenpox and belongs to the herpesvirus family. Like other viruses in this group, it has the ability to persist in the body after the initial infection.
After a person has had chickenpox, VZV does not leave the body but remains in the sensory nerve ganglia.
Thus, primary VZV infection leads to chickenpox, and herpes zoster is the result of reactivation of a latent infection of this virus, which is caused by decreased immunity due to various circumstances (hypothermia, stress, etc.) or concomitant diseases that are accompanied by immunodeficiency (malignant blood diseases, HIV etc.). Due to the presence of this property, the chickenpox virus belongs to the group of pathogens of slow infections. It is worth noting that the chickenpox virus itself has an immunosuppressive property.
VZV is thought to have a short survival time in the environment. All herpes viruses are sensitive to chemical and physical effects, including high temperature.
The source of infection is a person with chickenpox or herpes zoster. The virus is contained on the mucous membranes and in the elements of the rash. A patient is considered contagious from the moment the rash appears until crusts form (usually up to 5 days after the last rash).
The chickenpox virus is highly contagious, meaning it is very likely to be transmitted through respiratory droplets or direct contact with characteristic skin lesions of an infected person. This is due to the fact that most of the population becomes ill in childhood.
80-90% of cases occur under the age of 14 years. Chickenpox is also characterized by high susceptibility (90-95%).
Most countries tend to have higher incidence rates in urban areas (700-900 per 100,000 population) and significantly lower rates in rural areas. The epidemiology of the disease differs in different climatic zones, for example, a significant difference is observed in temperate and tropical climates. The reasons for these differences are poorly understood and may relate to properties of the virus (which are known to be heat sensitive), climate, population density, and exposure risk (eg, daycare or school attendance, or number of siblings in the household).
Why is chickenpox so relevant in the modern world?
The relatively mild course and low mortality rate have long been the reason for an extremely calm attitude towards this infection.
However, at the moment, as a result of numerous studies, it has been established that the pathogen can affect not only the nervous system, skin and mucous membranes, but also the lungs, digestive tract, and genitourinary system.
The virus has an adverse effect on the fetus when the disease occurs in pregnant women. It is worth remembering that the mother can transmit the infection to the fetus if she is sick with chickenpox or herpes zoster (the virus can penetrate the placenta throughout pregnancy).
Vaccines
The chickenpox vaccines currently available on the market are produced using the so-called Oka VZV strain, which has been modified through sequential propagation in different cell cultures. Various formulations of such live, attenuated vaccines have undergone rigorous testing and have been approved for use in Japan, the Republic of Korea, the USA, and several European countries. Some vaccines are approved for use at ages 9 months and older.
From a logistical and epidemiological point of view, the optimal age for chickenpox vaccination is 12-24 months. In Japan and several other countries, one dose of vaccine is considered sufficient, regardless of age. In the United States, 2 doses of the vaccine given 4-8 weeks apart are recommended for adolescents and adults, of whom 78% seroconverted after the first dose and 99% after the second dose.
According to the current US vaccination schedule, children receive 2 doses of the vaccine (1st dose at 12 months, 2nd at 6 years).
More about vaccines
What are the manifestations of chickenpox (chickenpox)?
The chickenpox virus enters through the respiratory tract and conjunctiva. It is believed that the virus multiplies in the mucous membrane of the nasopharynx and regional lymph nodes.
The initial entry of the virus into the blood occurs a few days after infection and contributes to the entry of the virus into the epithelial cells of the skin, where further reproduction of the virus and corresponding skin changes occur.
Then a secondary entry into the blood . It should be remembered that not only the skin epithelium can be affected, but also the mucous membranes of the gastrointestinal tract, respiratory tract, and genitourinary system. Considering that the virus is tropic to nervous tissue, degenerative and necrotic changes can develop in the nerve ganglia, sensory nerve roots and spinal cord.
Incubation period . The period from the virus entering the body to the onset of clinical manifestations ranges from 5 to 21 days after exposure, usually 1-2 weeks. The incubation period may be longer in immunocompromised patients.
Infected people may have a mild prodrome that precedes the onset of the rash. In adults, this may be 1 to 2 days of fever and malaise, but in children, a rash is often the first sign of illness.
The onset is most often acute . Fever lasts 2-7 days, longer in severe cases. Patients complain of an itchy rash, body aches, decreased appetite, sleep disturbance, and headache. Nausea and vomiting may occur.
The first elements of the rash appear on the face and torso, and then on the scalp and extremities; The greatest concentration of lesions is on the torso with the appearance of rashes within 4-6 days. In this case, elements of the rash are present at several stages of development (for example, redness and papules can be observed simultaneously and in the same area as vesicles and crusts).
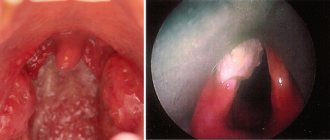
The rash can also occur on the mucous membranes of the oropharynx, respiratory tract, vagina, conjunctiva and cornea.
The rash elements usually have a diameter of 1 to 4 mm. Vesicles (bubbles) are superficial, single-chambered and contain clear liquid, surrounded by a red rim. Over time, they dry out and turn into crusts, after rejection of which temporary pigmentation and occasionally small scars remain.
The number of rash elements ranges from single to multiple. The vesicles may rupture or fester before they dry out and take on a crusty appearance. The rash is accompanied by severe itching.
In 20-25% of patients, rashes may occur on the mucous membranes of the mouth and gums. Usually they quickly open, form erosions and are accompanied by pain, burning and increased salivation.
About 2-5% of patients have elements of a rash on the conjunctiva.
Also, with chickenpox, as a rule, the lymph nodes (submandibular, cervical, axillary, inguinal) become enlarged.
Recovery from the initial chickenpox infection usually results in lifelong immunity. But recently, cases of recurrent chickenpox have become increasingly common. This is not common in a healthy person, and most often occurs in immunocompromised individuals.
What complications can occur with chickenpox?
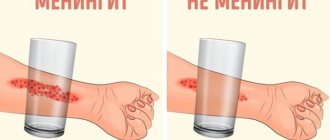
The disease is usually mild, but complications may occur, including bacterial infections (eg, bacterial skin lesions, pneumonia) and neurological infections (eg, encephalitis, meningitis, myelitis), which can be fatal.
Secondary bacterial skin infections , which are caused by streptococcus or staphylococcus, are the most common cause of hospitalization and outpatient medical visits. Secondary infection with invasive group A streptococci can cause abscesses and cellulitis.
Pneumonia after chickenpox is usually viral, but can also be bacterial. Secondary bacterial pneumonia is more common in children under 1 year of age. It is characterized by an increase in temperature up to 40⁰C, an increase in pallor and cyanosis of the skin, the appearance of a substernal dry cough and shortness of breath. Patients can take a forced position in bed.
Damage to the central nervous system in chickenpox ranges from aseptic meningitis to encephalitis. Cerebellar involvement followed by cerebellar ataxia is the most common presentation of central nervous system disorders but usually has a positive outcome.
Encephalitis is one of the most dangerous complications of chickenpox (10-20% of cases are fatal). This complication manifests itself as headache, nausea, vomiting, convulsions and often leads to coma. Diffuse brain involvement is more common in adults than in children. Chickenpox meningitis may occur together with encephalitis or independently .
Rare complications of chickenpox include Guillain-Barré syndrome, thrombocytopenia, hemorrhagic and bullous chickenpox, glomerulonephritis, myocarditis, arthritis, orchitis, uveitis, iritis and hepatitis.
Once infected, the virus remains hidden in nerve cells and can be reactivated, causing a secondary infection, herpes zoster. It usually occurs in adults over the age of 50 or with a weakened immune system and is associated with a painful rash that can cause permanent nerve damage.
What is herpes zoster?
Herpes zoster (shingles) occurs in people as a manifestation of the reactivation of a latent infection caused by a virus that was in the nerve ganglia after chickenpox. The localization of subsequent rashes will depend on which nerve ganglion the virus (VZV) was in a latent (dormant) state.
Localization of the rash in case of damage to the trigeminal nerve ganglion - on the scalp, in the forehead, nose, eyes, lower jaw, palate, tongue; if the virus is present in the spinal ganglia - on the neck, trunk, upper and lower extremities.
Features of the rash with herpes zoster are:
- vesicles are located on the skin in groups along the corresponding nerve,
- the disease most often begins with pain, followed by redness and corresponding rashes,
- over time the pain becomes less and less,
- the process is always one-sided,
- Usually the rashes are accompanied by fever, malaise, and weakness.
General information
Varicella (chickenpox) is an acute, highly contagious viral disease common throughout the world. Once one case occurs among susceptible individuals, it is very difficult to prevent an outbreak. While chickenpox is a relatively mild illness in childhood, it can become more serious in adults. It can be fatal, especially in newborns and those with weakened immune systems.
The causative agent, varicella zoster virus (VZV), is transmitted through respiratory droplets or direct contact, and patients are usually contagious for several days before the onset of the rash until the rash crusts over. Transmission of infection through third parties and household items is impossible.
VZV is a double-stranded DNA virus belonging to the herpes virus family. Only one serotype is known, and humans are its only reservoir.
The varicella zoster virus VZV enters the human body through the mucous membrane of the nasopharynx and almost without exception causes clinical manifestations of the disease in susceptible individuals. After infection, the virus remains latent in the nerve ganglia and, as a result of VZV activation, can cause herpes zoster (herpes zoster), a disease mainly affecting the elderly and those with weakened immune systems.
What methods exist for diagnosing chickenpox?
Usually the diagnosis is made on the basis of the clinical picture and an objective examination of the patient.
To confirm the diagnosis using laboratory methods, blood, cerebrospinal fluid, and the contents of vesicles and pustules are taken. Microscopy is used as an oriented method.
In modern practice, serological diagnostic methods are used (ELISA, RSK, RNGA, RIA). In this case, blood is taken twice: at the beginning of the disease and during the period of convalescence. The reaction is considered positive if the antibody titer increases 4 times or more.
It is worth noting that ELISA and PCR are the most commonly used. There is also a method for cultivating the virus, but due to labor intensity and high costs, it is not currently used.
How to treat chickenpox?
Patients with an uncomplicated course are most often treated at home. Elements of the rash are treated with a concentrated solution of potassium permanganate. The oxygen that is released as a result of this prevents the addition of a secondary infection and also reduces itching. For a small number of rashes, you can use brilliant green.
Only in severe or complicated cases is treatment directed at the pathogen necessary. These are drugs acyclovir, valacyclovir, famciclovir, which can only be taken after consulting an infectious disease specialist or family doctor. Antiviral treatment is mandatory for herpes zoster. Local application of acyclovir ointments is also possible.
If the itching is severe, those with chickenpox should take antihistamines. For severe pain in patients with herpes zoster - analgesics. If there is a high temperature and severe intoxication, detoxification therapy (intravenous administration of certain solutions) is indicated. Immunoglobulin is indicated for persons who have a reduced level of immunity.
Latest epidemics
The incidence of chickenpox is widespread in all countries of the world. In Russia, there is an annual increase in the number of diseases of this infection. From 1998 to 2007, the incidence of chickenpox increased 1.8 times annually; 500–700 thousand cases of chickenpox are registered every year.
An interesting fact: the chickenpox vaccine became available in the Russian Federation in 2009. From the end of 2013 to 2015 there was a break in the supply of vaccines to our country. According to Rospotrebnadzor, in 2015 there was an increase in the incidence of chickenpox by 16% compared to 2014.
How to prevent chickenpox?
Chickenpox can be prevented through vaccination. Specific prevention is carried out with live vaccines from a weakened varicella zoster virus (for example, the Belgian vaccine Varilrix). Vaccination is especially recommended for young children, and in the United States for the elderly, to prevent herpes zoster and postherpetic neuralgia.
In clinical trials, it was found that individuals who were vaccinated were either not susceptible to chickenpox or experienced it in a very mild form.
Chickenpox vaccines
Vaccination is necessary for those categories of people who have reduced immunity and, as a result, a high risk of severe and complicated course of the disease. These include the following categories:
- persons with malignant diseases,
- HIV-infected,
- those groups of people who have severe chronic pathology,
- patients taking glucocorticosteroids.
Vaccination indicated:
- for preventive purposes, especially recommended for high-risk categories: - routine vaccination at the age of 12-15 months, - routine second dose at the age of 4-6 years.
- for emergency prevention of those who have not had chickenpox and have not been vaccinated, but are in contact with patients.
The minimum interval between doses of varicella vaccine is 3 months for children under 13 years of age.
Although single-dose programs are effective in preventing severe varicella disease, as demonstrated by a study in Australia (one of the few countries to include varicella vaccination as part of its national immunization program), evidence suggests that it is not necessary to interrupt transmission of the virus. two doses are required. Emerging school outbreaks and high rates of chickenpox, although usually not severe, have prompted some countries to implement a two-dose vaccination schedule.
Vaccination is the most effective medical intervention ever invented by man.
Used materials
- https://www.cdc.gov/vaccines/pubs/pinkbook/varicella.html - etiology, pathogenesis, clinical features, prevention of chickenpox
- https://www.who.int/immunization/sage/meetings/2014/april/5_The_potential_impact_Varicella_vaccination_Low_Middle_Income_Countries_feasibility_modeling.pdf?ua=1&ua=1 – vaccination for chickenpox
- https://www.who.int/immunization/diseases/varicella/en/ - about the epidemiology of chickenpox and herpes zoster
- https://www.who.int/bulletin/volumes/92/8/13-132142/en/ - research on the effectiveness of vaccination against chickenpox and herpes zoster in Australia.
- https://www.who.int/immunization/position_papers/varicella_grad_effectiveness_2_doses.pdf?ua=1 - about the effectiveness of vaccination against chickenpox.
- https://www.who.int/wer/2014/wer8925.pdf?ua=1&ua=1 – epidemiology, diagnosis, treatment, some positions on vaccination for chickenpox and herpes zoster.
- Vozianova Zh. I. Infectious and parasitic diseases: In 3 volumes - K.: Health, 2000. - T. 1. - 904 p.
- Golubovskaya O. A. Infectious diseases. - M.: VSV "Medicine", 2012. - 728 p. + 12 s. color. on
Author: Anastasia Lishnevskaya, infectious disease doctor Source: MMK Formed
Effectiveness of vaccination
Other than vaccination, there are no countermeasures to control the spread of chickenpox or the incidence of herpes zoster in susceptible populations. Varicella-zoster immune globulin and herpes medications are very expensive and are mainly used as prophylaxis after exposure to infection or to treat chickenpox in people at high risk of developing severe disease. Due to the extreme contagiousness of chickenpox, almost all children and young adults in the world are affected. Each year from 1990 to 1994, before the chickenpox vaccine was available, there were about 4 million cases of the disease in the United States. Of this number, approximately 10,000 patients required hospitalization and 100 patients died.
Varicella vaccines using the Oka strain of VZV have been on the market since 1994. Positive results regarding safety, effectiveness and cost-effectiveness analyzes supported the rationale for their introduction into childhood immunization programs in a number of industrialized countries. After following study populations for 20 years in Japan and 10 years in the United States, more than 90% of immunocompetent individuals vaccinated in childhood were still protected against varicella.
About 95% of children will produce antibodies in response to vaccination, and 70-90% will be protected from infection for at least 7-10 years after vaccination. According to Japanese researchers (Japan is the first country in which the vaccine was registered), immunity against chickenpox lasts 10-20 years. It is safe to say that the circulating virus promotes “re-vaccination” of vaccinated people, increasing the duration of immunity.
Research suggests that emergency vaccination may also be effective - when the vaccine is given within 96 hours (preferably 72 hours) of exposure to VZV, at least 90% protective efficacy can be expected. Treatment for chickenpox in persons who have received the vaccine is much easier than in those who have not been vaccinated.
Historical information and interesting facts
Chickenpox was first described in the mid-16th century in Italy by doctors Vidus-Vidius and Ingranus. For a long time, chickenpox was not recognized as an independent disease and was considered a type of smallpox. After the causative agent of chickenpox was discovered in the contents of chickenpox vesicles in 1911, the disease began to be considered a separate nosological form. The virus itself was isolated only in 1958. The chickenpox virus infects only humans, and the only reservoir of infection is also humans.
First Comings
It is believed that smallpox originated in the region of Egypt (Middle East), however, in the numerous regional written sources that have reached us from that time, there is no mention of epidemics of this disease. Therefore, it is worth considering an alternative option related to the history of the ancient highly developed Indus (Harappan) civilization, which was discovered by archaeologists only in the 1920s. (Albedil, 1991).
"COOL" GODDESS
Shitala, the Hindu goddess of smallpox, occupies a very special place among the countless personifications of Devi, the variety of which is so rich in Hinduism. Her cult is widespread throughout almost the entire territory of Northern and Central India, from Sindh and Gujarat in the west of the country to Bengal, Assam and Orissa in the east, as well as outside the country - in Bangladesh and Nepal. Despite some variability in iconography, Sheetala is easily recognizable: she is depicted riding a donkey, naked or dressed as a married woman, often as an elderly Brahmin woman. She had a fan on her head, a broom and a vessel with water in her hands. The cult of this goddess obviously developed quite late - the first mentions of her appear in medical treatises of the 16th century, although descriptions of the disease itself are found in texts created long before the beginning of our era. Judging by many signs, the cult of Shitala is folk in origin and was not immediately included in Hindu religious ideas. Thus, there is no mention of Shitala in the early Brahminical texts, and its priests to this day are for the most part not Brahmins, but representatives of the low caste Malakars. In some places, blood sacrifices are still made to the goddess, although in general she prefers bloodless offerings - coconuts, cold rice, sweets and other “cooling” foods. The goddess, born from the cooled ashes of a sacrificial fire, hates heat and always seeks coolness, rewarding those who can appease her and punishing careless adherents with the heat of smallpox. It is not surprising that within these ideas, smallpox was seen not as a dangerous disease, but rather as the result of the manifestation of the presence of an angry deity. Therefore, treatment of a patient with smallpox primarily included procedures aimed at cooling the body of the unfortunate victim of divine rage: cold drink, fanning, wiping the body with ice water or wet leaves of the neem tree - the favorite plant of the goddess, truly known for its effectiveness against many skin diseases. All these actions were accompanied by chants addressed to Sheetala. The highest mortality rate from smallpox was recorded in India during the hot, dry months of the year, from February to April, decreasing sharply towards the beginning of the rainy season. Therefore, smallpox in India was often called a spring disease, and Shitala, accordingly, a spring goddess (the main holiday dedicated to her falls in mid-March). And today, during the holiday, in order to avoid the wrath of the “cool” goddess, any “warming” actions are prohibited - cooking hot food, eating spices, lighting fires in houses, as well as marital relations. Although the name of this goddess is primarily associated with smallpox, her character is very multifaceted. For example, Sheetala is also considered the protector of children and the giver of good fortune. But although the features of the cult may vary from place to place, the main characteristic of the goddess remains unchanged - she is always “cool” (this is how her name is literally translated from Sanskrit). Today, "cool" Shitala is more than a local deity protecting against smallpox: she serves as a symbol and constant living reminder of the need to maintain the correct balance of heat and cold in the human body. Violation of this balance, causing the wrath of the goddess, can lead to the emergence of a dangerous disease.
K. M. Vozdigan, senior specialist of the exhibition department of the Museum of Anthropology and Ethnography (Kunstkamera) RAS, St. Petersburg
About 2.5 thousand years BC. e. in a long river valley The largest cities of that time appeared on the Indus River, the population of which by the beginning of the 2nd millennium BC. e. was about 5 million people. However, for an unknown reason, 1.8-1.6 thousand years BC. e. these cities were depopulated. There is no evidence that they died as a result of wars or natural disasters; Moreover, during excavations of the largest city of Mohenjo-Daro, numerous human remains were found on the streets without visible wounds or damage, despite the fact that, as archaeologists have established, cremation of the dead was typical for this culture.
The most obvious explanation for the collapse of the Indus civilization, one of the three most ancient civilizations of mankind, along with the ancient Egyptian and Sumerian, may be an epidemic of a fatal disease. Since the time of occurrence of the smallpox virus (3.4 ± 0.8 thousand years ago) corresponds well to the period of a sharp decline in the population of the Indus Valley (3.8-3.6 thousand years ago), it can be assumed that it was smallpox in As a new deadly infection, it became the cause of mass epidemics among the local population, which had no immunity to it, which led to a sharp decrease in its population (Shchelkunov, 2009). The size of this human population appears to have prevented the infection from becoming endemic, and this highly virulent human infectious agent has disappeared.
However, its zoonotic progenitor (or a low-virulent variant of variola virus with a wide host range) apparently continued to circulate in a natural reservoir (rodents) over a large area. This situation is typical for any new highly lethal human infection: the most famous example is the Spanish flu epidemic in 1918-1919.
Researchers of ancient manuscripts, including the Talmud and the Bible, did not find in them descriptions of epidemics of a strictly anthroponotic infection with skin rashes resembling smallpox. However, if we use the assumption put forward above that the causative agent of smallpox originated from an orthopoxvirus with a wide range of hosts, which in the first stages of adaptation to humans of smallpox retained the properties of a zoonotic infection with little pathogenicity for humans, then in the text of the Bible we find the description we need, relating to the time of the exodus Jewish people from Egypt (14th century BC): “... and there was inflammation with boils on people and on livestock throughout the whole land of Egypt” (Exodus, the sixth plague of Egypt).
This indicates that in Egypt and the Middle East, already in ancient times, epidemics of zoonotic infection of people and domestic animals with skin rashes on the body, not accompanied by death, apparently occurred (Shchelkunov, 2011).
In modern times, smallpox showed its deadly power after the discovery of America by Europeans. During the XVI-XVII centuries. it was repeatedly brought to the New World from Europe and West Africa along with slaves. The indigenous population of America never encountered this infection, so smallpox became a terrible disaster for them - some tribes died out almost completely. It is known that in Mexico alone in 1520, smallpox claimed about 3.5 million lives! Only after powerful smallpox epidemics passed through both American continents did the disease become endemic with a low (less than 1%) mortality rate. The population of South and North America at the time of Columbus’s landing was about 70 million people, but as a result of similar epidemics and, to a much lesser extent, wars, by 1800 it had decreased to 600 thousand people
It is possible that the mysterious “catastrophe” of the Bronze Age in the Middle East and Eastern Mediterranean, dating back to 1.2-1.1 thousand years BC, is also connected with the smallpox epidemic, but with a high mortality rate. e. This period is characterized by a sharp decline in the human population of this vast region, the destruction of cities and catastrophic changes in social structure (Robbins and Manuel, 2001). And it was from this time that two of the three Egyptian mummies found with skin lesions characteristic of smallpox date back to this time (Fenner et al.
, 1988).
It can be assumed that during this period, in the region of the Middle East and Eastern Mediterranean, where several million people lived, a virus dangerous to humans re-emerged, but the insufficiently high human population again did not allow the new anthroponotic infection to become endemic and persist.
The next “coming” of smallpox occurred in the middle of 1 thousand years BC. e. on the Indian subcontinent. Here, in the Ganges Valley, by that time the largest (about 25 million people) and dense human population had formed. Obviously, this population size was already sufficient for the newly formed highly pathogenic strain of the virus to become endemic.
At this time, among the European countries, the most populous was Greece, whose population by 400 BC. e. was approximately 3 million people. In both Greece and the Middle East, smallpox apparently was not observed at that time: at least, there were no epidemics in the army of Alexander the Great on the way from the Mediterranean Sea to India. But during the stay of this army on the territory of the Indian subcontinent in 327 BC. e. There was an outbreak of the disease with skin lesions characteristic of smallpox.
The transition of smallpox to an endemic state in the Indian subcontinent ensured the persistence of this highly pathogenic agent for humans for many centuries, until the 20th century. From here, this disease gradually spread throughout the world, and it was possible to eliminate it on a global scale only in the second half of the last century with the help of special preventive vaccinations.