Pharmacological properties of the drug Paclitaxel
Antitumor drug of plant origin from the taxane group. Causes irreversible polymerization of microtubule proteins in the cell cytoplasm, as a result of which the dynamic equilibrium of the “polymerization-depolymerization” process, which ensures the normal functioning of intracellular structures throughout the entire life cycle of the cell, is disrupted. Paclitaxel induces the formation and accumulation of abnormal assemblies - microtubule bundles in interphase and numerous microtubule stars during mitosis, which leads to arrest of the cell life cycle in the G2 or M phase. After intravenous administration of paclitaxel, its concentration in the blood plasma is described by a two-phase curve. In vitro, 89–98% of paclitaxel is bound to blood proteins. Metabolism has not been fully studied. Only 1.3–12.6% of paclitaxel is excreted in the urine; It is believed that the main amount of paclitaxel is hydroxylated in the liver. The half-life ranges from 3 to 52.7 hours. The average volume of distribution at steady state varies from 198 to 688 l/m2. With increasing dose during a 3-hour infusion, the pharmacokinetics of paclitaxel becomes nonlinear. When the dose is increased by 30% (from 135 to 175 mg/m2), the maximum concentration and AUC values increase by 75 and 81%, respectively. There was no accumulation of paclitaxel during repeated courses of treatment.
Paclitaxel in chemotherapy of ovarian cancer
N
Despite the significant progress in chemotherapy of ovarian cancer achieved in the last decade of the last century and associated, to a large extent, with the emergence and widespread introduction into clinical practice of new antitumor drugs, the results of treatment of this disease today remain unsatisfactory.
The incidence of ovarian cancer has a steady upward trend
, and already in the first year from the moment of diagnosis, every third patient dies.
The use of only surgical treatment (subject to adequate staging) is possible for stage IAB in patients with a low risk of recurrence. In all other cases, chemotherapy (neoadjuvant and/or adjuvant) is necessarily included in the complex of treatment measures, and in case of stage IV of the disease or progression of the process it becomes the main method of treatment.
Today, in 80% of patients, the disease is diagnosed in late stages, and even with clinically established stage I, relapses and metastases subsequently occur in at least 25% of cases. Thus, the population of patients with ovarian cancer who need modern and adequate chemotherapy is extremely wide.
CP was considered the most active regimen
(cisplatin + cyclophosphamide).
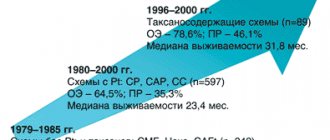
The emergence of taxanes, and primarily paclitaxel
, characterized by a unique mechanism of action, has made it possible to achieve significant results.
The first phase II clinical studies of paclitaxel revealed its high antitumor activity in ovarian cancer [2] (Table 1).
The most impressive results were from the Jon Hopkins Group. The effect was registered in 12 out of 41 patients. The main manifestation of toxicity was leukopenia, which required a dose reduction from 250 mg/m2 to 110 mg/m2 and became increasingly dose-limiting from course to course. Similar results were obtained by GOG and Alb. Einstein Group.
Preclinical tests conducted in vitro
on various human tumor cell lines showed that the suppression of the growth of malignant cells under the influence of paclitaxel is dose- and regimen-dependent [4,21].
However, in in vivo
, the maximum antitumor effect was achieved at doses lower than the maximum tolerated [42]. Taking into account these data and the phase II results establishing the high hematological toxicity of paclitaxel at doses > 200 mg/m2, a study of lower doses of 110–200 mg/m2 was initiated. At the same time, paclitaxel was initially considered as a 2nd-line drug, giving in monochemotherapy a fairly high rate of objective effect in platinum-resistant patients (up to 20–30% for a duration of 3 to 6 months).
Table 2 shows the design of the randomized Euro-Canadian phase III trial in disseminated ovarian cancer, which included 382 patients previously treated with cisplatin [11]. This protocol compared two doses of paclitaxel, 135 mg/m2 and 175 mg/m2, and two administration regimens, a 3-hour and a 24-hour infusion.
The overall effectiveness was independent of the duration of infusion and was slightly higher when using a dose of 175 mg/m2 compared with 135 mg/m2 (20% and 17%, respectively, the differences were not statistically significant). However, the time to disease progression at a dose of 175 mg/m2 in a 3-hour infusion mode (group B) turned out to be significantly longer (19 weeks) than in groups A, C and D (14 weeks each). In addition, longer 24-hour infusions were associated with more severe granulocytopenia compared with 3-hour infusions (74% and 17%, respectively, p < 0.0001).
The results of subsequent studies of paclitaxel alone in platinum-resistant patients are presented in Table 3.
The effectiveness of treatment ranged from 13 to 38%, median survival - from 9.6 to 13.2 months.
Thus, the use of paclitaxel at a dose of 175 mg/m2 as a 3-hour infusion once every 3 weeks was considered optimal for ovarian cancer. This mode is now considered standard and is widely used in practice. Due to the fact that the drug is mainly inactivated in the liver and excreted in the bile, if liver function is impaired, its dose should be reduced to 135 mg/m2 and lower (75–50 mg/m2) [42]. Less than 10% of paclitaxel is excreted by the kidneys, so there is no indication of the need for dose reduction in renal failure [35].
The next stage of clinical research was the study of paclitaxel in first-line combination chemotherapy in patients with disseminated ovarian cancer
. The experiment found that the sequence of administration of cytostatics is very important: paclitaxel infusion should be carried out before cisplatin [20]. This is explained by the fact that platinum derivatives increase the number of cells in the S phase, and the subsequent administration of paclitaxel, which acts in the G2|M phase, is ineffective. In addition, administration of cisplatin before paclitaxel increases the toxicity of the latter by reducing its plasma clearance. This may be due to the modulating effect of cisplatin on cytochrome P450 enzymes [18,28].
The results of four randomized international trials comparing paclitaxel + cisplatin (TP) with the then standard cyclophosphamide + cisplatin (CP) regimen are presented in Table 4.
In the
GOG-111
, 386 patients with stage III–IV ovarian cancer after suboptimal cytoreductive operations received 6 cycles of polychemotherapy in the
TP
(paclitaxel - 135 mg/m2 24 h + cisplatin 75 mg/m2) or
CP
(cyclophosphamide 750 mg/m2 +) cisplatin 75 mg/m2). A significant advantage of the TP regimen over the CP regimen was demonstrated in both immediate and long-term results: the overall effectiveness was 73% and 60%, the median time to progression was 18 months. and 13 months, median survival – 38 months. and 24 months respectively.
In the OV-10
similar results were obtained, confirming the advantage of the combination of paclitaxel + cisplatin as the first line of chemotherapy, after which this regimen was widely introduced into clinical practice.
Next study ( GOG-132
) was aimed at assessing the role of each of the cytostatics and compared the TR regimen with monochemotherapy with paclitaxel and cisplatin (“3 arms”). The data obtained did not reveal any significant differences between the compared groups. Further analysis showed that as patients progressed in subsequent lines of treatment, they received crossover drugs. This, apparently, led to the same long-term results.
In the international study ICON 3
, including 2000 patients, compared 3 chemotherapy regimens: paclitaxel 175 mg/m2 + carboplatin AUC 6; one carboplatin AUC 6 and a combination of CAP (cisplatin 50 mg/m2 + doxorubicin 50 mg/m2 + cyclophosphamide 500 mg/m2). The median time to progression and overall survival were approximately the same (16.2–17.7 and 36–38 months, respectively, Table 4). However, as in the previous study, more than 30% of patients who progressed during chemotherapy with carboplatin or SAR subsequently received paclitaxel, which could affect the leveling of indicators in the compared groups. Overall, these reports supported the hypothesis that sequential use of platinum and paclitaxel is equivalent to their simultaneous use.
Attempts to improve treatment results by increasing the total number of courses did not produce the expected results. In the GOG-114
[24] compared the standard TR regimen with a more intensive one: 2 courses of carboplatin AUC 9, then 6 courses of paclitaxel 135 mg/m2 infusion over 24 hours + cisplatin intraperitoneal 100 mg/m2. The standard regimen was slightly inferior in terms of median time to progression, but overall survival was similar.
Considering the nephro-, oto- and neurotoxicity of cisplatin, the next stage of the work was to evaluate the possibilities of replacing cisplatin with carboplatin in combination with paclitaxel. Three international randomized studies (GOG 158, the German-Austrian AGO group and the Danish-Dutch group) compared the regimens of paclitaxel + cisplatin and paclitaxel + carboplatin in the first line of chemotherapy in patients with ovarian cancer (Table 5).
In all three studies, both regimens demonstrated equal efficacy in both immediate and long-term results, with significantly higher toxicity in combination with cisplatin.
Thus, in the USA and European countries, the combination of paclitaxel 175 mg/m2 + carboplatin AUC 5–7
(once every 3 weeks, 6 cycles in total) is currently recognized as
the “gold standard” of first-line chemotherapy for ovarian cancer
.
Randomized trials for the treatment of recurrent ovarian cancer in platinum-sensitive patients also clearly demonstrated the advantages of combinations with paclitaxel compared with platinum derivatives alone in both immediate and long-term results (Table 6).
The ICON4/OVAR2.2 protocol included 802 patients with late relapses of ovarian cancer (6 months after the end of platinum-containing chemotherapy). Treatment was carried out with a combination of paclitaxel with platinum derivatives or platinum derivatives alone. 1-year progression-free survival and 2-year overall survival were significantly better in the paclitaxel group (49% and 59%) compared with cisplatin/carboplatin monotherapy (40% and 50%), p = 0.006 [19].
Similar data on the advantage of the combination of paclitaxel + carboplatin compared with carboplatin alone in the treatment of recurrent ovarian cancer in platinum-sensitive patients were presented by the Spanish group [13]. The overall effectiveness of treatment was significantly higher when using the combination (74.4%; CR - 23.1%) compared with carboplatin alone (52.6%; CR - 21%).
Given the meta-analysis data showing that the addition of anthracyclines to first-line chemotherapy without taxanes significantly improves long-term treatment outcomes [43], a number of randomized studies (EORTC-NSGO-NCIC and German-Franco-Austrian) were conducted comparing the combination of TCb (carboplatin AUC–5+ paclitaxel 175 mg/m2 3 hours) with the triple combination of TECb (carboplatin AUC–5+ paclitaxel 175 mg/m2 3 hours + epirubicin 60 mg/m2 before paclitaxel). When assessing the effectiveness of treatment, a certain advantage of the three-component regimen was noted (PR - 48% and 42%, PR - 38% and 32%, differences are not significant), however, it was characterized by higher myelotoxicity, which required a reduction in doses of cytostatics and an increase in the intervals between courses [9] .
Reports of new two- and three-component paclitaxel-based regimens for advanced ovarian cancer deserve close attention.
of paclitaxel + platinum drugs + topotecan is very promising
. When using the regimen of topotecan 1 mg/m2 on days 1, 2, 3 + paclitaxel 175 mg/m2 3 hours on day 3 + carboplatin AUC–5 on day 3 (6 courses every 3 weeks), the overall effectiveness was 88. 2%, of which pathomorphologically confirmed complete remission is in 23.5% of patients [6]. The main toxicity was hematological (grade 3–4 neutropenia – 40%, grade 3–4 anemia – 45%).
In a study by Engelholn S. et al., 2000 (the regimen featured 6-day oral administration of topotecan), the effectiveness of this combination as a 1st line reached 100%
.
The same 100% effectiveness reported by Herben et. al. (1999), achieved using the combination of paclitaxel 110 mg/m2 24 hours 1st day + cisplatin 75 mg/m2 2nd day + topotecan 0.3 mg/m2 120 hours (days 1–6) as the first line in patients with stage III–IV ovarian cancer, but the regimen required the administration of hematohormones.
A phase III multicenter randomized trial comparing the combination of paclitaxel/carboplatin and topotecan/paclitaxel/carboplatin in patients with stage III (suboptimal) and stage IV ovarian cancer is currently underway [37]. Group A receives paclitaxel 175 mg/m2 + carboplatin AUC–5 once every 3 weeks; group B – topotecan 1 mg/m2 on days 1, 2, 3 + paclitaxel 175 mg/m2 on day 3 + carboplatin AUC–5 on day 3 once every 3 weeks.
The results of the combination paclitaxel + carboplatin + altretamine, developed in the chemotherapy department of the Russian Cancer Research Center named after. N.N. Blokhin, as 2–3rd lines of treatment: 70.4% overall effectiveness and 29.6% complete regressions [1].
An important direction is the development of modes for the sequential use of various combinations. Table 7 presents the results of such studies.
In addition to the standard regimen, since the mid-90s, the interest of researchers in short infusions of paclitaxel, carried out once a week, has increased significantly. The fact is that paclitaxel is a phase-specific cytostatic agent that acts on tumor cells in the G2|M phase of the cell cycle. Repeated administration of the drug once a week leads to an increase in the number of dividing cells exposed to paclitaxel in the G2|M phase and, accordingly, their death increases [23].
In addition, longer exposure to the cytostatic agent resulting from its weekly administration may enhance the effect by enhancing the antiangiogenic effect and increasing tumor cell apoptosis [27].
Studies by European scientists have shown that for ovarian cancer, short weekly infusions of low doses (60–90 mg/m2) are as effective as standard treatment regimens. The randomized Swedish-Finnish study included 208 patients with ovarian cancer who had previously received platinum-based therapy [3,36]. Group I received paclitaxel by 3-hour infusion once every 3 weeks. 200 mg/m2. Group II also received paclitaxel for 3 hours, but weekly, at an average dose of 67 mg/m2, while the course dose for 3 weeks was almost 210 mg/m2. The effectiveness of treatment was approximately the same (37% and 35%, respectively) with a median overall survival of 14.7 and 13.6 months. The toxicity of the standard regimen was significantly higher: grade 3–4 neutropenia 45% versus 18%, grade 3 neuropathy 29% versus 11%, alopecia 79% versus 46%.
Kern J. et al. (2000) used weekly administrations of paclitaxel 80 mg/m2 as a 1-hour infusion in 31 patients. The overall effectiveness was 55%, stabilization was achieved in another 20%.
At the 14th International Congress on Anticancer Therapy in Paris in 2003 [32], it was emphasized that paclitaxel
in a weekly regimen, it is currently
the most active drug for second-line monochemotherapy in platinum-resistant patients
(overall effectiveness - 33-47%), significantly superior to gemcitabine (19%), oral etoposide (27%), liposomal doxorubicin (10%) and topotecan (10%).
At the State Scientific Research Center named after. N.N. Blokhin RAMS, GUN Research Institute of Oncology named after. prof. N.N. Petrov Ministry of Health of the Russian Federation and the Sverdlovsk Regional Oncology Center of the Oncology Scientific and Practical Center are conducting a clinical trial of paclitaxel, manufactured by Dr. Reddy's Laboratories Ltd. called Mitotax
®
.
Its structure is identical to the antitumor drug paclitaxel and has similar activity. The drug is available in convenient packaging in bottles of 30 mg/5 ml, 100 mg/16.7 ml and 250 mg/41.7 ml. Composition: active substance: paclitaxel, 1 ml of concentrate contains 6 mg of active substance. Excipients: polyoxyl 35, castor oil, absolute alcohol. In a preliminary analysis of the experience of using Mitotax in patients with ovarian cancer, the spectrum of antitumor activity and toxicity is completely similar to paclitaxel, which allows us to recommend the drug for widespread use in clinical practice [1]. The premedication regimen used for weekly infusions is noteworthy. Before the first injection, 8–10 mg of dexamethasone is used, then its dose is progressively reduced to 8, 6 and 4 mg. In some cases, if no hypersensitivity reactions were observed, dexamethasone was even discontinued.
In conclusion, it should be noted that the combination of paclitaxel 175 mg/m2 + carboplatin AUC 5–7 (once every 3 weeks, 6 cycles in total) is the “gold standard” of first-line chemotherapy for ovarian cancer, and paclitaxel in a weekly regimen is currently day is the most active drug for second-line monotherapy for resistance to platinum derivatives.
The inclusion of paclitaxel in a second-line combination during progression of ovarian cancer should be mandatory for both platinum-sensitive and platinum-resistant patients. Use of Mitotax® (paclitaxel) manufactured by Dr. Reddy's Laboratories Ltd. allows you to make treatment economically accessible without compromising its quality. Literature:
1. Blumenberg A.G. Paclitaxel and its new possibilities in the treatment of patients with ovarian cancer. // Rus. Honey. Zhurn., 2003, T.11, No. 11, pp. 648–651.
2. Manzyuk L.V. Doses and modes of administration of Taxol. // N.I. Perevodchikova (ed.) Taxol in clinical practice. – Moscow: “Polina”. – 2001. – P. 25–54.
3. Anderson H., Boman K., Ridderhein N. et al. An updated analysis of randomized study of single agent paclitaxel (P) given weekly versus every 3 weeks to patients with ovarian cancer treated with prior platinum therapy. //Proc. ASCO. – 2000. – 19. – 380a, abs. 1505.
4. Arbuck SG, Canetta R., Onetto N., Christian MS Current dosage and schedule issues in the development of paclitaxel (Taxol). // Semin. Oncol. – 1993. – V. 20 (Suppl. 3). – P.31–39.
5. Bolis G., Parazzini F., Scarfone G. et al. // Ginecol. Oncol., 1999, 72: 60–64.
6. Bolis G., Scarfone G., Sciatta C. et al. Phase II study of topotecan, carboplatin (C) and paclitaxel as front line treatment in suboptimal advanced epithelial ovarian cancer (AEOC). Proc. ASCO, 2000, abs.1543.
7. Colombo N. et al. Randomized trial of paclitaxel and carboplatin vs control arm of carboplatin or CAP: the trial international collaborative Ovarian Neoplasm Study (ICON 3). //Proc. ASCO. – 2000; 19:379a (abs. 1500).
8. DuBoi A., Richter B., Warm M. et al. Cisplatin/Paclitaxel vs Carboplatin/Paclitaxel as 1st–line treatment in ovarian cancer. //Proc. ASCO 1998; 17, 1395(abs.).
9. DuBoi A., Weber B., Pfaisterer J. et al. Epirubicin/Paclitaxel/ Carboplatin vs Carboplatin/Paclitaxel in First–line treatment of ovarian cancer FIGO stages IIb–IV. Intergroup phase III trial. //Proc. ASCO, 2001; 20: 805(abs.).
10. Einzig AI, Wiernik P, Sasloff J et al. Phase II stage of taxol in patients with advanced ovarian cancer. //Proc. Am. Assoc. Cancer Res. – 1990. – 31. – 1114.
11. Eisenhauer E. A., ter Bokkel Huinink W. et al. European–Canadian randomized trial of paclitaxel in relapsed ovarian cancer: high–dose versus low–dose and long versus short infusion. //J.Clin.Oncol. – 1994. – V. 12. – P. 2654–2666.
12. Engelholn S., Hovarth G. et al. Revers–schedule oral topotecan, paclitaxel and carboplatin in primary advanced OC: a phase I dose–randing study. // 25 ESMO Congress 13–17 oct. 2000, Ann. Oncol., 11 (suppl. 4): 81 (abs. 361o).
13. Gonzales Martin A.A., Calvo E., Bover I. et al. Randomised phase II study of carboplatin (C) versus paclitaxel–carboplatin (PC) in platinum–sensitive (PS) recurrent ovarian carcinoma (AOC) with assessment of quality of life (QOL): a GEICO study (Spanish Group for investigation on ovarian carcinoma Proc ASCO, 2003, 22: 451, abs.1812.
14. Harries M., Moss C., Perren T. et al. Carboplatin followed by sequential weekly paclitaxel and gemcitabine as first–line treatment for women with ovarian cancer. Proc. ASCO, 2003, 22: 450, abs.1808.
15. Herben VM, Panday VR et al. Phase I pharmacologic study of the paclitaxel, cisplatin and topotecan administered intravenously every 21 days as first–line therapy in patients with advanced OC. // J. Clin. Oncol., 1999, 17 (3) < p. 747–755.
16. Hoskins P., Eisenhauer E., Fisher B. et al. Sequential couplets of cisplatin/topotecan and cisplatin/paclitaxel as first–line therapy for advanced epithelial ovarian cancer: an NCIC Clinical Trials Group Phase II study. Proc. ASCO, 1999, 18: 357a (abs.1378).
17. Kern J., Trope C., Baekelandt M. et al. A study weekly Taxol in patients with recurrent platinum resistant ovarian cancer. 25th ESMO Congress. 13–17 Oct. 2000. Hamburg. Germany. Annals of Oncology, V. 11, suppl. 4, P. 83, abs. 379p.
18. LeBlanc GA, Sundseth SS, Weber GF, Waxman DJ Platinum anticancer drugs modulate P–450 mRNA levels and differentially alter hepatic drug and steroid hormone metabolism in male and female rats. Cancer Res 1992, 52:54–57.
19. Ledermann JA Randomized trial of paclitaxel in combination with platinum chemotherapy versus platinum–based chemotherapy in treatment of relapsed ovarian cancer. Proc. ASCO, 2003, 22: 446, abs.1794.
20. Liebmann JE, Fisher J, Teague D et al. Sequence dependence of paclitaxel (Taxol) combined with cisplatin or alkylators in human cancer cells. Oncol. Res., 1994, 6: 25–31.
21. Lopes NM, Adams EG, Pitts TW, Bhuyan BK Cell kill kinetics and cell cucle effects of taxol on human hamster ovarian cell lines. Cancer Chemother. Pharmacol 1993, 32:235–242.
22. Maenpaa J., Jalkanen J., Kuoppala T. et al. Sequential gemcitabine–carboplatin (GC) and paclitaxel–carboplatin in first–line chemotherapy for advanced epithelial ovarian cancer (OC). Proc. ASCO, 2003, 22: 464 (abs.1865).
23. Manfredi JJ, Parness J., Horwitz SB Taxol binds to cellular microtubules. J Cell Biol 1982, 94: 688–696.
24. Markman M., Bundy B., Benda J. et al. Randomized phase III study of intravenous cisplatin/paclitaxel versus moderately high dose carboplatin followed by iv paclitaxel and intraperitoneal cisplatin in optimal residual cancer: an intergroup trial. Proc. ASCO; 1998; 17:361a.
25. McGuire WP, Rowinsky EK, Rosenchein NB et al. Taxol: a unique antineoplastic agent with significant activity in advanced ovarian epithelial neoplasm. Ann Int Med 1989, 111: 273–279.
26. McGuire WP, Hoskins WJ, Brady MP et al. Cyclophosamide and cisplatin compared with paclitaxel and cisplatin in patients with III and IV ovarian cancer. // N. Engl. J. Med. – 1996. – V. 334. – P. 1–6.
27. Milross CG, Mason KA, Hunter NR et al. Relationship of mitotic arrest and apoptosis to antitumor effect of paclitaxel. // J.Nat.Cancer Inst. – 1996. – V. 88. – P. 1308–1314.
28. Monsarrat B., Alvinerie P., Wright M. et al. Hepatic metabolism and biliary excretion of taxol in rats and hummans. Monogr. Nat. Cancer Inst. 1993, 15: 39–46.
29. Muggia F., Brady M., Sutton G. et al. Phase III trial of cisplatin or paclitaxel versus their combunation in suboptimal stage III and IV epithelial ovarian cancer. Gynecologic Oncology Group study # 132. // Proc. ASCO 1997; 16:352a.
30. Neijt JP, Hansen M, Hansen SW et al. Randomized phase III study in previously unrelated epithelial ovarian cancer FIGO stage IIB, IIC, III, IV comparing paclitaxel–cisplatin and paclitaxel–carboplatin. //Proc. ASCO 1997; 16:352a (abs. 1259).
31. Ozols R., Bundy B., Fowler J. et al. Randomized phase III study of cisplatin versus carboplatin in optimal stage III ovarian cancer: a Gynecologic Oncology Group study. //Proc. ASCO. – 1999; 18:356a.
32. Ozols RF Management of recurrent ovarial cancer. 14th International Congress on Anti-Cancer treatment, 1st–4th feb. 2003. – Proc. Book – P.124–130.
33. Pectasides D., Papadopoulou M., Vartbalitis J. et al. // Oncology. – 1998. – V. 55. – P. 228–34.
34. Potamianou P., Polyzos A., Andoulakis N. et al. Sequential combination of paclitaxel–carboplatin and paclitaxel–liposomal doxorubicin as a 1st line treatment in patients with ovarian cancer: a multicenter phase II trial. Proc. ASCO, 2003, 22: 483 (abs.1941).
35. Ramanath RK, Capozzoli MG, Trump DL Escalating doses of weekly paclitaxel in combination with cisplatin: a phase I study in advanced malignances. //Proc. ASCO. – 1999. – 18. – abs. 638.
36. Rosenberg P., Anderson H., Boman K. et al. A randomized multicenter study of single agent paclitaxel (Taxol) given weekly versus every 3 weeks to patients with ovarian cancer treated with prior platinum therapy. Proc. ASCO, 1999, 18: abs. 1420.
37. Scarfone G., Bolis F., Parazzini F. et al. A multicenter, randomized phase III study of paclitaxel/carboplatin (PC) versus topotecan/paclitaxel/carboplatin (TPC) in patients with stage III (residual tumor > 1 CM–RT) and IV ovarian cancer (OC). //Proc. ASCO. –2003; 22: 450 (abs. 1807).
38. Stuart G., Bertelsen K., Mangioni C. et al. Updated analysis shows a highly significant improved overall survival (OS) for cisplatin–paclitaxel as a first line treatment of advanced ovarian cancer: mature results of the EORTC–GCCG, NOCOVA, NC 1C CTG and Scottish Intergroup Trial. //Proc. ASCO. – 1998. – 17:361a. – abs.1394.
39. Ten Bokkel Huinink W., Gore M., Carmichael C. et al. Topotecan versus paclitaxel for the treatmant of recurrent epithelial ovarian cancer. //J.Clin.Oncol. – 1997. – V. 15. – P. 2183–93.
40. Thigpen T., Blessing J., Ball H. et al. Phase II trial of taxol as a second–line therapy for ovarian carcinoma: a Gynecologic Oncology Group study. //Proc. ASCO. – 1990. – 9. – 604.
41. Trope C., Hogberg T., Kaern J. et al. Long–term result from a phase II study of single agent paclitaxel (Taxol) in previonsly platinum treated patients with advancad ovarian cancer: the Nordic experience. //Ann. Oncol. – 1998. – V. 9. – P. 1301–1307.
42. Venook AP, Egorin M, Brown TD et al. Paclitaxel (Taxol) in patients with liver dysfunction. (CALGB 9264). //Proc. ASCO. – 1994. – 13. – 139, abst.350.
43. Vermorken JB, Harper PG, Buyse M. The role of antracyclines in Epithelial ovarian cancer. Ann. Oncol., 1999; 10 (suppl. 1): 43–50.
Indications for use of the drug Paclitaxel
Non-small cell lung cancer in patients for whom radical surgical treatment and/or radiation therapy is not indicated. Common form of ovarian carcinoma (as monotherapy or as part of combination antitumor therapy):
- for primary treatment of ovarian cancer in patients with an advanced form of the disease or with residual tumor (more than 1 cm) after surgical treatment in combination with treatment with cisplatin;
- for the treatment of recurrent ovarian cancer with metastases when standard therapy is ineffective.
Metastatic breast carcinoma when standard therapy is ineffective.
Use of the drug Paclitaxel
Usually prescribed at a dose of 175 mg/m2 as a 3-hour infusion once every 3 weeks, provided that the number of platelets in the peripheral blood is at least 100,000 per 1 mm3, neutrophil granulocytes - at least 1500 per 1 mm3; otherwise, the next course of treatment is carried out only after normalization of hematological parameters. If, after the previous course of treatment, the patient developed severe neutropenia (the number of neutrophil granulocytes less than 500 per 1 mm3), lasting 7 days or more or accompanied by the development of infectious complications, as well as severe peripheral neuropathy, the dose of paclitaxel for subsequent administrations is reduced by 20%. Before administering paclitaxel, all patients are given premedication to prevent hypersensitivity reactions. Premedication includes the administration of corticosteroids (dexamethasone 20 mg or its equivalent intramuscularly or orally 12 and 6 hours before infusion), antihistamines (diphenhydramine 50 mg IV as a bolus 30 minutes before infusion), H2-receptor blockers (cimetidine 300 mg or ranitidine 50 mg IV 30 minutes before infusion).
Paclitaxel
The use of paclitaxel should be under the supervision of a physician experienced in the use of anticancer chemotherapy drugs. Paclitaxel should be used as a diluted solution.
Before administering Paclitaxel, patients should be premedicated with glucocorticosteroids, H1 and H2 histamine receptor blockers.
If Paclitaxel is used in combination with cisplatin, Paclitaxel should be administered first followed by cisplatin.
Anaphylaxis and serious hypersensitivity reactions
In less than 1% of patients, despite premedication, serious hypersensitivity reactions were observed during treatment with Paclitaxel. The frequency and severity of such reactions did not depend on the dose or schedule of administration of the drug. With the development of severe reactions, the most frequently observed symptoms were suffocation, hot flashes, chest pain, tachycardia, as well as abdominal pain, pain in the extremities, increased sweating, and increased blood pressure (BP).
If severe hypersensitivity reactions develop, administration of Paclitaxel should be stopped immediately and, if necessary, symptomatic treatment should be prescribed; in such cases, repeated courses of treatment with the drug should not be prescribed.
Reactions at the injection site
During intravenous administration of the drug, the following usually mild reactions at the injection site were observed: swelling, pain at the injection site, erythema, tenderness at the injection site, induration at the injection site, hemorrhages, which can lead to the development of cellulite. Such reactions were observed more often with a 24-hour infusion than with a 3-hour infusion. In some cases, the onset of such reactions was observed both during the infusion and 7-10 days after it.
Myelosuppression
Bone marrow suppression (mainly neutropenia) is dose- and dosage-dependent and is the main dose-limiting toxicity. For example, when cisplatin is administered at a dose of 75 mg/m2 and Paclitaxel at a dose of 175 mg/m2 as a 3-hour infusion, severe neurotoxicity is observed more often than when Paclitaxel is administered at a dose of 135 mg/m2 as a 24-hour infusion. , i.e. The duration of infusion has a greater influence on the risk of developing myelosuppression than the dose.
In patients with a history of previous radiotherapy, neutropenia developed less frequently and to a milder extent, and did not worsen as the drug accumulated in the body.
In patients with ovarian cancer, the risk of renal failure is higher when using the combination drug Paclitaxel + cisplatin compared to cisplatin monotherapy.
Infections were very common and sometimes fatal, including sepsis, pneumonia and peritonitis. Urinary and upper respiratory tract infections were reported as the most common complicated infections. At least one opportunistic infection has been reported in immunosuppressed patients, patients with HIV infection, and patients with AIDS-related Kaposi's sarcoma.
The use of maintenance therapy, including granulocyte colony-stimulating factor, is recommended for patients who have experienced severe neutropenia.
A decrease in the platelet count below 100,000/μl was observed at least once during the entire duration of therapy with Paclitaxel, sometimes the platelet count was below 50,000/μl. There were also cases of bleeding, most of which were local, and the frequency of their occurrence was not associated with the dose of Paclitaxel and the administration schedule.
When using the drug Paclitaxel, it is necessary to regularly monitor your blood count. The drug should not be prescribed to patients with a neutrophil count of less than 1500/μL and less than 1000/μL in patients with Kaposi's sarcoma due to AIDS, and with a platelet count of less than 100,000/μL (75,000/μL in patients with Kaposi's sarcoma due to AIDS).
If severe neutropenia (less than 500/μl) or severe peripheral neuropathy develops during treatment with Paclitaxel, it is recommended to reduce the dose by 20% during subsequent courses of treatment (in patients with AIDS-related Kaposi's sarcoma, by 25%).
Effect on the cardiovascular system
The decrease, increase in blood pressure (BP) and bradycardia observed during the administration of Paclitaxel are usually asymptomatic and in most cases do not require treatment. A decrease in blood pressure (BP) and bradycardia were usually observed during the first 3 hours of infusion. ECG abnormalities were also noted in the form of repolarization disorders such as sinus tachycardia, sinus bradycardia and early extrasystole. In severe cases, treatment with Paclitaxel should be suspended or discontinued.
Monitoring vital signs is recommended, especially during the first hour of drug infusion. If Paclitaxel is used in combination with trastuzumab or doxorubicin for the treatment of metastatic breast cancer, monitoring of cardiac function is recommended.
Cases of severe cardiac conduction disturbances have been reported during treatment with Paclitaxel. If symptoms of cardiac conduction disturbances are detected, patients should be prescribed appropriate therapy along with constant ECG monitoring of the cardiovascular system.
Effect on the nervous system
The incidence and severity of nervous system disorders were generally dose-related. Peripheral neuropathy, usually moderate, was often observed during treatment with Paclitaxel. The incidence of peripheral neuropathy increased as the drug accumulated in the body. Cases of paresthesia were often observed in the form of hyperesthesia.
If severe neuropathy is noted, it is recommended to reduce the dose by 20% in subsequent courses of treatment (in patients with Kaposi's sarcoma due to AIDS - by 25%).
Peripheral neuropathy may be a reason to discontinue therapy with Paclitaxel.
Symptoms of neuropathy decreased or completely disappeared within several months after stopping drug therapy.
The development of neuropathy during previous therapy is not a contraindication for the use of Paclitaxel.
Rarely, abnormal optic nerve evoked potentials have been reported in patients with permanent optic nerve damage.
The possible exposure to ethanol contained in Paclitaxel should be taken into account.
Effect on the gastrointestinal tract
Mild and moderate cases of nausea/vomiting, diarrhea, and mucositis were very common in all patients.
Cases of mucositis depended on the drug administration regimen and were more often observed with a 24-hour infusion than with a 3-hour infusion.
Rare cases of neutropenic enterocolitis (typhlitis), despite co-administration of granulocyte colony-stimulating factor, have been observed in patients using Paclitaxel alone and in combination with other chemotherapy drugs.
Liver failure
Patients with liver failure are at risk for toxic side effects, especially grade 3-4 myelosuppression. Careful monitoring of the patient's condition should be established and, if necessary, consideration should be given to adjusting the dose of the drug.
Radiation pneumonitis has been reported with concomitant radiation therapy.
Patients should use reliable methods of contraception during treatment with Paclitaxel and for at least 3 months after the end of therapy.
Vaccination
When used together, Paclitaxel and live viral vaccines may potentiate the replication of the vaccine virus and/or may increase side effects when using vaccines, since normal protective mechanisms may be inhibited due to the use of Paclitaxel. Vaccination with live viral vaccines in patients using the drug Paclitaxel can lead to the development of severe infections. The patient's immune response to such a vaccine may be reduced.
The use of live vaccines should be avoided in such patients and specialist advice should be obtained.
Fertility
Taking into account the possible mutagenic effect of Paclitaxel, patients of both sexes should be advised to use effective contraception during therapy with Paclitaxel and for 6 months after the end of therapy. Also, due to a possible decrease in fertility in men, cryopreservation of sperm may be recommended for the possibility of conceiving a child in the future.
Side effects of the drug Paclitaxel
Myelosuppression - severe neutropenia (27%), thrombocytopenia (6%), severe thrombocytopenia (1%), anemia (62%), severe anemia (6%); allergic reactions: skin rash (14%), hot flashes (28%), angioedema, bronchospasm, generalized urticaria (2%); arterial hypotension (22%), bradycardia (3%), AV block, ventricular tachycardia, tachycardia in combination with bigeminy (2%), peripheral edema (10%), extremely rarely - myocardial infarction, congestive heart failure (noted during combination chemotherapy, in particular when using anthracyclines); peripheral neuropathy, manifested mainly by paresthesia (64%, and in 4% of patients the symptoms when using the drug in recommended doses were severe), rarely - grand mal attacks and encephalopathy, extremely rarely - muscle weakness, paralytic ileus, optic nerve damage, impairment of visual fields (luminous scotomas), especially with overdose (these effects are usually reversible); reversible alopecia (82%); arthralgia and myalgia (54%, of which in 14% of cases in severe form); nausea and vomiting (44%), diarrhea (25%), anorexia (25%), mucositis (20%), constipation (18%), intestinal obstruction (4%), increased AST activity (18%), alkaline phosphatase ( 18%), hyperbilirubinemia (4%), isolated cases of liver necrosis and hepatic encephalopathy with a fatal outcome, neutropenic and ischemic enterocolitis and intestinal perforation; nail damage and isolated cases of radiation-like dermatitis; local reactions: hyperemia, thrombophlebitis at the injection site (4%). Extravasation with IV administration can lead to the development of edema, tenderness, erythema, infiltration and cellulite; Skin discoloration may occur. Paclitaxel is a potential mutagenic, embryotoxic and fetotoxic agent.
Introduction
Lung cancer is the most common cause of death from cancer in men.
About 80% of lung cancer cases are non-small cell lung cancer (NSCLC). Up to 60% of NSCLC patients have stages IIIb (locally advanced NSCLC) and IV (metastatic NSCLC) at the time of diagnosis. Since NSCLC at these stages is an incurable disease, the goal of therapy in these patients is to maximize life expectancy and improve its quality [1, 2, 6, 7]. The combination of paclitaxel and carboplatin is one of the main combination chemotherapy regimens used in the first line of treatment of advanced NSCLC [1, 3, 7, 10]. Taking into account the high cost of these drugs, the question of the therapeutic equivalence of imported and more affordable domestic chemotherapy drugs is of considerable interest.
In 2009, a clinical trial of the drugs Taxacad (paclitaxel) and Carboplatin began, in which the assessment of safety and effectiveness is carried out in accordance with international criteria. The drugs Taxacad and Carboplatin are produced by Biocad CJSC (Russia) from substances of its own production in a modern plant that complies with GMP (Good Manufacturing Practice) standards.
This paper presents the interim results of a study assessing the safety and effectiveness of therapy with Taxacad and carboplatin in patients with stage III–IV NSCLC.
Material and methods
47 patients from 8 centers were screened for the open multicenter clinical trial.
To be included in the study, the patient had to meet the following criteria:
- age at least 18 years;
- providing written informed consent;
- confirmed diagnosis of NSCLC stages III–IV;
- presence of measurable foci of disease;
- ECOG (Eastern Oncology Cooperative Group) index value 0–1 point inclusive;
- life expectancy greater than 20 weeks;
- the level of bilirubin is less than 25.7, creatinine is less than 133.0 µmol/l, transaminases are not higher than three times the maximum normal values (in the presence of metastases in the liver - no higher than five times).
The patient was not eligible for inclusion in the study in the following cases:
- carrying out cytostatic therapy before inclusion in the study;
- neutropenia;
- thrombocytopenia;
- presence of signs of peripheral neuropathy of the second or higher degrees;
- metastatic brain damage;
- the presence of diseases that can affect the assessment of the severity of symptoms of the underlying disease;
- the presence of other malignant diseases noted over the past 5 years;
- presence of signs of chronic renal failure;
- presence of signs of epilepsy or a convulsive syndrome of another origin in the anamnesis;
- any acute or active chronic infections;
- any signs of mental illness;
- a history of allergies to substances included in the study drugs (Taxacad, Carboplatin);
- drug addiction, alcoholism, HIV infection;
- simultaneous participation in other clinical trials;
- the presence of obstacles to the administration of chemotherapy drugs in the form of intravenous infusions.
Due to non-compliance with inclusion criteria, two patients dropped out of screening. One patient dropped out before the administration of study drugs due to the development of acute myocardial infarction. One patient withdrew his consent to participate in the study before administration of the study drugs. Within 2 weeks after inclusion in the study, one patient had brain metastases, and two had clinical signs of rapid disease progression, which was regarded as non-compliance with the inclusion criteria and resulted in discontinuation of participation in the study.
Therefore, the analysis included 40 patients (31 men and 9 women) who met the study inclusion criteria and received at least one dose of Taxacad and Carboplatin. The average age of the patients was 58 years (range 34 to 74 years).
In this study, Taxacad and Carboplatin, pharmaceutically equivalent to the original drugs, were used. On the first day of each cycle, patients included in the study received Taxacad at a dose of 175 mg/m2 as a 3-hour intravenous infusion after standard premedication, followed by a 30-minute intravenous infusion of Carboplatin at a dose corresponding to AUC = 6. The cycles were repeated. every 21 days.
With the development of grades III–IV neutropenia and/or febrile neutropenia after chemotherapy, a course of daily subcutaneous injections of the granulocyte colony-stimulating factor (G-CSF) drug Leukostim (filgrastim, Biocad, Russia) was prescribed at a dose of 5 mcg/kg/day until the number of neutrophils reached > 2 × 109/l.
The antitumor effect was assessed based on RECIST criteria (Response Evaluation Criteria in Solid Tumors) after the 3rd and 6th courses of chemotherapy. Further evaluation of the effectiveness of therapy in these patients was carried out 6, 9 and 12 months after the start of treatment.
The first step at the statistical processing stage was to determine the type of features available and the nature of their distribution. To describe quantitative continuous characteristics, the distribution of which corresponded to the law of normal distribution, the mean value (M), standard deviation (SD) and/or 95% confidence interval (CI) were used. To describe qualitative ordinal characteristics, the median (Me) and interquartile range (25–75%) were used.
results
20.0% of patients were diagnosed with stage IIIa NSCLC, 12.5% with stage IIIb, and the majority (65.0%) of patients with stage IV. Most patients were diagnosed with multiple distant metastases: pleura – 3 cases, liver – 4, adrenal glands – 5, kidneys – 2, bones and spine – 6, distant lymph nodes – 5; damage to the other lung occurred in 12 cases, metastases to the ipsilateral lobe - in 7.
From 1 to 6 cycles of chemotherapy were carried out (1 course - 2 patients, 2 courses - 3, 3 courses - 12, 4 courses - 1, 5 courses - 3, 6 courses - 19; in total - 177 courses). Safety data were analyzed for all patients who received at least one dose of the study drug.
The assessment of the safety and tolerability of the drugs Taxacad and Carboplatin was based on data on the frequency and severity of side effects of chemotherapy, including deviations in clinical and biochemical blood tests (according to the NCI CTC - National Cancer Institute-Common Toxicity Criteria, version 2.0.), results of assessment of general somatic status according to the Karnofsky scale as modified by ECOG and assessment of neurological status. Data on toxicity assessment based on laboratory parameters are presented in table. 1.
. Overall toxicity (proportion of patients who experienced these changes).
During the entire observation period, grade III anemia was observed in 5% of patients; there were no cases of grade IV anemia. A transient decrease in the number of leukocytes was noted to a level corresponding to grades I–II toxicity in 60% of patients. Only 10% of patients had grade III leukopenia. There were no cases of grade IV leukopenia. There was a transient decrease in the number of neutrophils to the level of I–II degrees of toxicity in 35% of patients, and in 40% of patients neutropenia of III–IV degrees was noted. However, only 35% of cases required the administration of G-CSF. The proportion of patients who experienced grades III–IV neutropenia reached 29.2% by the 4th course of chemotherapy (Fig. 1). Thrombocytopenia of III degree (without clinical manifestations) was registered in 2.5% of cases. There were no cases of severe thrombocytopenia grade IV.
Laboratory studies did not reveal a single case of severe hepatic-renal toxicity. The NCI CTC toxicity criteria, version 2.0, were also used to assess the severity of peripheral neuropathy, one of the most common side effects of paclitaxel and carboplatin. During screening (before the start of treatment), signs of peripheral neuropathy were absent in all patients. In total, during the observation period, the development of neuropathy of degrees I–II was noted in 25% of cases; cases of the development of severe forms (grades III–IV) were not registered.
General somatic status was assessed using the ECOG scale. When screening before treatment, the ECOG score was 0 in 16 (40%) patients and 1 in 24 (60%). After 3 courses of chemotherapy (day 64), data are available for 35 patients. The ECOG score was 0 in 12 (34.3%) patients, 1 in 19 (54.2%), 2 in 3 (8.6%) and 3 in 1 (2.9%). After 6 courses of chemotherapy (day 126, data available for 19 patients), the ECOG score was 0 in 3 (15.8%) patients, 1 in 15 (78.9%) and 3 in 1 (5 .3%). Deterioration of general somatic status according to the ECOG scale was associated with progression of the underlying disease or concomitant pathology.
One serious side effect has been reported: cardiomyopathy due to anemia after 4 cycles of chemotherapy, resulting in death. A relationship with the study treatment was assessed by the investigator as unlikely.
In addition, the following side effects were observed (in addition to the laboratory abnormalities described above):
- 50% (n = 20) of patients had alopecia of degrees II–III; relationship with study therapy was assessed as probable;
- 17.5% (n = 7) of patients had cases of myalgia, arthralgia and ossalgia of mild to moderate severity; assessed by investigators as related to drug intake;
- 15% (n = 6) of patients had episodes of mild to moderate asthenia; assessed by investigators as related to drug intake;
- 10% of patients (n = 4) experienced mild to moderate nausea, sometimes accompanied by vomiting; assessed by researchers as drug-related;
- 10% (n = 4) experienced allergic reactions (eosinophilia, Quincke's edema, reactions during infusion); were assessed by the researchers as being related to the drug. Two patients dropped out of the study due to the development of these side effects;
- 17.5% (n = 7) of patients had pain of various localizations, which was regarded by the researchers as not related to the study therapy. Most likely, the pain was caused by manifestations of the underlying disease;
- 10% (n = 4) had shortness of breath, cough, and hemoptysis, which, in the opinion of the researcher, were not related to taking the drug;
- 1 (2.5%) case of bilateral fungal pneumonia was registered. Considered by the investigators to be unrelated to the study drugs and not a serious side effect that did not affect the regimen/dose of the study drugs. Pneumonia was completely cured as a result of antimycotic therapy;
- in 1 (2.5%) case, leukocyturia was observed 20 days after the start of therapy. Considered by investigators to be unrelated to drug intake. Completely relieved by antibacterial therapy;
- in 1 (2.5%) case, febrile temperature was observed even before the start of treatment and persisted throughout the entire observation period. Considered by investigators to be unrelated to study therapy.
To evaluate the effectiveness, computed tomography with contrast was performed. Evaluation of the effectiveness of the treatment based on RECIST criteria was performed in 35 patients; 3 patients were not included in the effectiveness analysis because they dropped out before the first assessment (2 due to allergic reactions, 1 due to disease progression unconfirmed by instrumental methods); two were not included in the efficacy analysis because they were withdrawn from the study after 2 cycles of chemotherapy due to clinical deterioration, although stabilization was noted when assessed by RECIST criteria.
8 patients dropped out of the study due to verified disease progression after 2–3 cycles of chemotherapy (in 1 of 8 patients with disease progression, the assessment was carried out after 2 courses of chemotherapy due to the need to confirm clinical signs of progression), 2 patients with significant tumor regression (stabilization and partial response) after 3 courses of chemotherapy, radical surgical interventions were performed, 7 patients dropped out before re-evaluating the effectiveness (2 due to the development of side effects, 3 for reasons not related to the study drug). In 20 patients, efficacy was re-evaluated in accordance with RECIST criteria (in 19 - after 6, in 1 - after 5 courses of chemotherapy).
According to RECIST criteria, partial response was observed in 7 (20.0%) patients, stabilization in 20 (57.1%) and progression in 8 (22.9%) patients.
Discussion
In accordance with international experience in registering generic drugs based on active substances of a chemical nature, they are considered therapeutically equivalent to the original drugs if there is evidence of their pharmaceutical equivalence and bioequivalence. Pharmaceutical equivalence implies the identity of the content of the active substance and the characteristics of the dosage form of the original and generic drugs, as well as compliance of the generic drug with pharmacopoeial quality criteria. A generic drug is considered bioequivalent to the original drug if its bioavailability (the speed and extent with which the active substance is absorbed and appears in the systemic circulation) does not differ significantly from the original drug. Bioequivalence studies cannot be applied to intravenously administered drugs, since bioavailability is always 100% when administered intravenously. As a result, generic drugs administered intravenously, including most cytostatics, are approved for medical use based only on evidence of pharmaceutical equivalence obtained during the state quality examination.
However, the best evidence of therapeutic equivalence has been and remains clinical studies that assess the safety and effectiveness of the drug. Given that the combination of paclitaxel and carboplatin in NSCLC has been well studied, the scope of clinical trials of generic drugs may be limited. Thus, when conducting a clinical trial of generics using protocols whose design replicates previously conducted international multicenter studies, it is possible to compare the results obtained with retrospective data, and the sample size can be significantly reduced.
Due to the high relevance of the issue of import substitution of expensive drugs with more affordable domestic analogues and taking into account international experience in the study of generic drugs, we developed a protocol for a clinical study of the drugs Taxacad and Carboplatin, the preliminary results of which are presented in this work.
For the purpose of comparative analysis of data on the incidence and severity of side effects, we analyzed literature data [3, 4, 5, 8, 10] on the most typical side effects in patients who received from 6 to 10 cycles of combination chemotherapy with paclitaxel and carboplatin (Table 2). In addition, severe cardiotoxicity has been reported in rare cases, ranging from 0.5% [4] to 3.0% in the ECOG study [10]; stomatitis [5]; ototoxicity, including severe, in 3% of cases [8].
. Safety and toxicity profile of the combination of paclitaxel and carboplatin, according to foreign clinical studies.
Comparative data on the frequency of side effects in this and international clinical studies [5, 8] are presented in Fig. 2. Data on severe (corresponding to toxicity grades III-IV, according to NCI CTC criteria, version 2.0) hematological toxicity are presented in Fig. 3 [5, 8].
Thus, the side effects observed with the use of Taxacad and Carboplatin (alopecia, nausea, arthralgia/myalgia, asthenia, neutropenia) are expected. The frequency and severity of side effects did not exceed those recorded in international multicenter clinical studies. Moreover, the incidence of some adverse events in this study was lower compared to the literature, which may be due to the shorter duration of treatment, lower course dose of chemotherapy, and the smaller number of patients included in the study to date.
In order to evaluate the effectiveness of the drugs Taxacad and Carboplatin, we compared the results of evaluating the effectiveness according to RECIST criteria with literature data on the rate of objective response and stabilization when using similar chemotherapy regimens in the treatment of advanced NSCLC. Thus, in a study by Kosmidis P. et al. [5] the use of paclitaxel at a dose of 175 mg/m2 (as a 3-hour intravenous infusion) and carboplatin at a dose corresponding to AUC = 6 every 3 weeks allowed achieving a complete response in 6.7% of cases, a partial response in 18.9 %, stabilization – in 38.9% [5].
In a multicenter, randomized, comparative phase III clinical trial [8] using the regimen of paclitaxel 200 mg/m2 as a 3-hour intravenous infusion and carboplatin at a dose corresponding to AUC = 6, with an interval of 21 days, a complete response was achieved in 1% patients, partial – in 24%, stabilization – in 40%.
In a comparative randomized clinical trial conducted by ECOG [10], one of the groups used a regimen of paclitaxel at a dose of 225 mg/m2 as a 3-hour intravenous infusion and carboplatin at a dose corresponding to AUC = 6, with an interval of 21 days. The proportion of patients who achieved a complete response was less than 1%, partial – 19%, stabilization – 21%. In a study by Scagliotti G. et al. [9] conducted a comparative assessment of the effectiveness of three platinum-containing regimens. In 1 (n = 204) of the groups, patients received paclitaxel 225 mg/m2 and carboplatin AUC = 6 on day 1 every 3 weeks. According to the study results, the rate of achieving an objective effect and stabilization in the described group was 68.5%. In a comparative randomized phase III study conducted by the Southwest Oncology Group Trial [3], one of the groups used a similar design. After 6–10 cycles of chemotherapy, a complete response was recorded in 1% of cases, a partial response in 24%, and stabilization in 33%.
The results of a preliminary assessment of the effectiveness of Taxacad and carboplatin in terms of the overall response rate (complete and partial response; Fig. 4), as well as objective effect and stabilization (Fig. 5) are consistent with data from international multicenter clinical trials.
Conclusion
Thus, the results of this study suggest that the safety and effectiveness of combination chemotherapy based on the generic drugs Taxacad and Carboplatin are not significantly different compared to the safety and effectiveness of a similar regimen based on the original drugs paclitaxel and carboplatin.
Research into the effectiveness and safety of Taxacad and Carboplatin is currently ongoing. The goal of the second phase of the study is to study the drugs in a group of 100 patients to determine the rate of objective clinical response, progression-free survival and overall one-year survival.
It should be noted that the presented work is the first and so far the only Russian clinical study in the field of oncology that evaluates the effectiveness of domestic generic drugs in accordance with RECIST criteria.
Information about the authors: Marenich Alexander Fedorovich – senior researcher, Russian Cancer Research Center named after. N.N. Blokhin RAMS. Tel.; Reutova Elena Valerievna – Russian Cancer Research Center named after. N.N. Blokhin RAMS. Tel.; Sheveleva Lyudmila Petrovna – head of the CT department, Volgograd Regional Clinical Oncology Dispensary No. 1. 8; Karaseva Nina Alekseevna – Candidate of Medical Sciences, Head of the Thoracic Department, City Oncology Dispensary, St. Petersburg. Tel.; Bogdanova Natalya Viktorovna – head of the CTO polyclinic, Moscow Scientific Research Oncology Institute named after. P.A. Herzen Rosmedtekhnologii; Uskov Dmitry Albertovich – oncologist, Moscow Regional Oncology Dispensary of the Ministry of Health of the Moscow Region. Tel.; Khasanov Rustem Shamilevich – chief physician, Clinical Oncology Dispensary, Kazan. Tel.; Mukhametshina Guzel Zinurovna – Clinical Oncology Dispensary, Kazan; Tuzikov Sergey Aleksandrovich – Doctor of Medical Sciences, head of the department of thoracoabdominal oncology, Oncology Research Institute of the Tomsk Scientific Center of the Siberian Branch of the Russian Academy of Medical Sciences. Tel.; M iller Sergey Viktorovich – Doctor of Medical Sciences, senior researcher at the Department of Thoracoabdominal Oncology, Research Institute of Oncology, Tomsk Scientific Center of the Siberian Branch of the Russian Academy of Medical Sciences. Khorinko Andrey Vitalievich – head of the 1st chemical technical department, Perm regional oncology dispensary. Tel.
Special instructions for the use of Paclitaxel
Do not allow the undiluted concentrate to come into contact with polyvinyl chloride containing a plasticizer, from which devices for transfusion of infusion solutions can be made. To minimize the risk of ingestion of plasticizer (di-[2-ethylhexyl] phthalate), which may be extracted from polyvinyl chloride containers or infusion sets, diluted solutions of paclitaxel should be prepared and stored in glass, polypropylene or polyolefin containers and administered through an infusion system with an internal surface made of polyethylene. The paclitaxel infusion system must have a membrane filter with a pore diameter of no more than 0.22 µm. If severe hypersensitivity reactions occur, paclitaxel should be discontinued immediately and not re-administered. When using paclitaxel, regular monitoring of peripheral blood composition, blood pressure, heart rate, and ECG is indicated, especially during the 1st hour of drug infusion. If a patient develops myocardial conduction disturbances during treatment with the drug during repeated administrations, continuous ECG monitoring should be performed. Caution must be exercised when handling paclitaxel; Medical personnel should use protective gloves. If paclitaxel solution gets on the skin or mucous membranes, they should be washed immediately with plenty of running water. Upon local contact with paclitaxel, a tingling, burning sensation, as well as skin hyperemia is noted; Accidental inhalation of paclitaxel vapor may cause shortness of breath, chest pain, burning sensation in the eyes, sore throat and nausea.
Similar drugs:
- Metoject Solution for injection
- Wartec Cream for external use
- Letrozole Oral tablets
- Medroxyprogesterone acetate Substance-powder
- Imuran Oral tablets
- Zoladex Capsule
- Paclitaxel Substance-powder
- Lomustine Oral tablets
- Votrient Oral tablets
- Cyclophosphan Substance-powder
** The Drug Directory is intended for informational purposes only. For more complete information, please refer to the manufacturer's instructions. Do not self-medicate; Before you start using Paclitaxel, you should consult your doctor. EUROLAB is not responsible for the consequences caused by the use of information posted on the portal. Any information on the site does not replace medical advice and cannot serve as a guarantee of the positive effect of the drug.
Are you interested in the drug Paclitaxel? Do you want to know more detailed information or do you need a doctor's examination? Or do you need an inspection? You can make an appointment with a doctor - the Euro lab is always at your service! The best doctors will examine you, advise you, provide the necessary assistance and make a diagnosis. You can also call a doctor at home . Euro lab clinic is open for you around the clock.
** Attention! The information presented in this medication guide is intended for medical professionals and should not be used as a basis for self-medication. The description of the drug Paclitaxel is provided for informational purposes only and is not intended for prescribing treatment without the participation of a physician. Patients need to consult a specialist!
If you are interested in any other drugs and medications, their descriptions and instructions for use, information about the composition and form of release, indications for use and side effects, methods of use, prices and reviews of drugs, or you have any other questions and suggestions - write to us, we will definitely try to help you.