Cefotaxime is better for premature newborns, with jaundice or the need for calcium administration, and for adults it is necessary to choose Ceftriaxone for bleeding, ulcerative colitis, concomitant heart disease, in the 2nd and 3rd trimester of pregnancy (under medical supervision).
Treatment with Ceftriaxone is cheaper and simpler, since only 1 injection is needed (at the same cost of vials), and there is no need to change the dose in case of renal failure. There is no difference between these antibiotics in terms of the strength of their antibacterial action and the types of microbes they kill. Contraindications and a number of side effects differ.
Comparison of the effectiveness of Cefotaxime and Ceftriaxone
The effectiveness of Cefotaxime is quite similar to Ceftriaxone - this means that the ability of the drug to provide the maximum possible effect is similar.
For example, if the therapeutic effect of Cefotaxime is more pronounced, then using Ceftriaxone even in large doses will not achieve this effect.
Also, the speed of therapy - an indicator of the speed of therapeutic action - is approximately the same for Cefotaxime and Ceftriaxone. And bioavailability, that is, the amount of a drug reaching its site of action in the body, is similar. The higher the bioavailability, the less it will be lost during absorption and use by the body.
Combination "ceftriaxone + sulbactam" (Sulbactomax)
To prevent the emergence of resistant bacteria, a combination of a cephalosporin (ceftriaxone) with a blactamase inhibitor (sulbactam) has been proposed (Payasi et al., 2010). The drug Sulbactomax contains this combination and is an innovative antibiotic with an expanded spectrum of antibacterial activity; it is active against most infectious agents of various localizations, including strains of microorganisms producing broad-spectrum and extended-spectrum blactamases. It is important that ceftriaxone and sulbactam do not interact with each other and do not change each other’s pharmacokinetic parameters.
The area of clinical use of ceftriaxone/sulbactam does not differ from that of ceftriaxone, probably the most successful of the third generation cephalosporins (Bereznyakov, 2012). The addition of sulbactam, a synthetic penicillanic acid sulfone, increases the microbiological activity of the combination due to the binding of sulbactam to penicillin-binding proteins, which are not affected by ceftriaxone, and expands the spectrum of antibacterial activity due to microorganisms that produce cephalosporinases. First of all, this applies to ESBLs, the emergence and widespread distribution of which some authors hastened to declare the end of the era of cephalosporins. The addition of a blactamase inhibitor to ceftriaxone allows one to overcome resistance caused by extended-spectrum blactamases of group 2be, oxacillinases of group 2d, cephalosporinases of group 2e, and even carbapenemases that do not contain zinc ions in the active center (group 2f) (Bereznyakov, 2006).
Comparison of the safety of Cefotaxime and Ceftriaxone
The safety of a drug includes many factors.
At the same time, with Cefotaxime it is quite similar to Ceftriaxone. It is important where the drug is metabolized: drugs are excreted from the body either unchanged or in the form of products of their biochemical transformations. Metabolism occurs spontaneously, but most often involves major organs such as the liver, kidneys, lungs, skin, brain and others. When assessing the metabolism of Cefotaxime, as well as Ceftriaxone, we look at which organ is the metabolizing organ and how critical the effect on it is.
The risk-benefit ratio is when the prescription of a drug is undesirable, but justified under certain conditions and circumstances, with the obligatory observance of caution in use. At the same time, Cefotaxime does not have any risks when used, just like Ceftriaxone.
Also, when calculating safety, it is taken into account whether only allergic reactions occur or possible dysfunction of the main organs. In other matters, as well as the reversibility of the consequences of the use of Cefotaxime and Ceftriaxone.
Pneumonia is one of the most common infections. Community-acquired pneumonia annually affects every sixth of 1000 inhabitants of the planet [1]. Nosocomial (nosocomial) pneumonia develops in 0.5–1.5% of hospitalized patients and in 10–30% of patients on mechanical ventilation [2]. In the USA, 300 thousand cases of nosocomial pneumonia are registered annually [3], in the UK – 50 thousand [4]. In Russia, the incidence of pneumonia is 396.7 per 100 thousand population [5]; in certain categories of patients it significantly exceeds the average. For example, among elderly people the incidence of community-acquired pneumonia reaches 44/1000, and among those living in organized groups – 68–114/1000 [6]. A high incidence of community-acquired pneumonia is also observed in population groups suffering from chronic diseases, especially cardiovascular diseases, chronic obstructive pulmonary disease, alcoholism, HIV infection and other immunodeficiency conditions, and malignant neoplasms.
In 1999, 747,390 cases of pneumonia were officially registered in Russia, of which 486,785 were in adults, 30,422 were in adolescents aged 15–17 years, and 230,183 were in children under 15 years of age [5]. However, according to experts, taking into account the large number of unreported cases and diagnostic errors, the actual number of episodes of the disease was 1,882,409 in adults, and 2,533,971 in the general population [5].
Pneumonia occupies one of the first places in the structure of mortality. In economically developed countries, they are in 4th–5th place among all causes of death after cardiovascular, oncological, cerebrovascular diseases, as well as chronic obstructive pulmonary disease, and in 1st place among the causes of death from infectious diseases [7, 8]. The mortality rate in patients with mild community-acquired pneumonia usually does not exceed 5%, but in severe cases of the disease it can reach 25–50% [9, 10]. A particularly high mortality rate is observed in patients over 60 years of age and young children, and, according to WHO, in Russia the mortality rate of children under 1 year of age (25.1 per 1000 population) is 2–4 times higher than that in other economically developed countries [ eleven]. Despite the success of chemotherapy, mortality from community-acquired pneumonia is increasing. Over the past 30 years it has increased from 1 to 9%. Mortality rates for nosocomial pneumonia range from 16 to 80% [10, 12–14].
Pneumonia results in significant direct and indirect medical costs. They cause temporary disability lasting an average of 25.6 days (12.8–45) [15]. Costs associated with community-acquired pneumonia reach $24 billion per year in the United States [16]. The annual cost of antimicrobial agents alone for outpatients with community-acquired pneumonia in the country is approximately $100 million [17]. Respiratory tract infections, primarily pneumonia, account for about half of the costs of antibiotics in hospital intensive care units [18]. At the same time, the cost of antibacterial drugs is only a small part of the cost of treatment as a whole. For example, in the USA, 92% of all costs for community-acquired pneumonia are the cost of hospitalization [19]. In case of nosocomial pneumonia, the main part of the financial costs is due to an increase in the patient's length of stay in the hospital, in general, and in the intensive care unit, in particular. For example, in a study conducted in China, the treatment costs of one patient with nosocomial infection were approximately 90% higher than those of a control patient [20]. Additional costs in case of development of nosocomial infection largely depended on its location and were maximum in pneumonia. The cost of treating nosocomial pneumonia was more than 4 times higher than the cost of treating nosocomial urinary tract infections (31,940 versus 17,349 yuan). The development of nosocomial infection was associated with an extension of hospitalization by an average of 25.53 days.
Similar findings were found in studies conducted in other countries. In the USA, the average lengthening of hospitalization due to nosocomial pneumonia was 7–30 days [21], in Germany – 24.17 [22]. Moreover, in the latter case, 14.03 days were spent in the intensive care unit, where the cost of treatment is significantly higher than in therapeutic departments.
Thus, adequate initial treatment of respiratory tract infections can prevent the development of conditions requiring hospitalization and complications of the disease, leading to a reduction in days of disability and disability, as well as a significant reduction in direct and indirect economic costs.
Monotherapy is indicated for most patients with pneumonia. Indications for prescribing combination antibacterial therapy include [23]:
- pneumonia in the intensive care unit with a severe course due to an unknown pathogen, especially complicated by sepsis;
- pneumonia against the background of severe immunodeficiency;
- pneumonia caused by microbial associations beyond the spectrum of action of available antibacterial drugs;
- pneumonia caused by weakly sensitive strains of microorganisms;
- pneumonia caused by P. aeruginosa
.
When choosing a specific drug, the following factors must be taken into account [23]:
- antimicrobial activity (bactericidal drugs have an advantage);
- stability to beta-lactamases;
- portability;
- age-related changes in the pharmacokinetics of drugs (it is necessary to ensure good penetration of the drug into sputum and lung tissue);
- ease of use for the patient (it is advisable that the frequency of administration does not exceed twice a day, otherwise the risk of non-compliance with the treatment regimen increases).
Unfortunately, many antibacterial agents widely used to treat pneumonia do not meet these requirements [23]. Thus, natural penicillins are not active against a number of potential pathogens of pneumonia (staphylococci, gram-negative bacteria), and in recent years the level of resistance of pneumococci to them has increased significantly. Aminopenicillins (ampicillin, amoxicillin) are destroyed by beta-lactamases. First generation cephalosporins (cephalothin, cefazolin, cephalexin) are not active against most gram-negative pneumonia pathogens and are destroyed by beta-lactamases of gram-negative bacteria. Aminoglycosides penetrate poorly into the lung tissue and are characterized by high toxicity. Their activity decreases during purulent processes. Tetracyclines have a bacteriostatic effect, are potentially toxic and are poorly tolerated by patients. Sulfonamides are also bacteriostatic and have an unfavorable side effect profile. In addition, high levels of pathogen resistance to sulfonamides, including co-trimoxazole, are now widely observed.
Antibiotics that best meet the above requirements include third-generation cephalosporins, primarily ceftriaxone. Third-generation cephalosporins began to attract special attention in the era of the spread of an “epidemic” of antibiotic resistance in the world of one of the main causative agents of respiratory infections – Streptococcus pneumoniae
, which causes 15–35% of community-acquired pneumonia and 10–20% of nosocomial pneumonia [24].
Penicillin-resistant strains of S. pneumoniae, the prevalence of which in some regions has reached 80% or more [25], in most cases remain sensitive to cefotaxime and ceftriaxone [26, 27]. In addition, these drugs are active against other common pathogens of lower respiratory tract infections - Haemophilus influenzae, Moraxella catarralis
and methicillin-sensitive staphylococci.
One of the ceftriaxone preparations presented on the domestic pharmaceutical market is Novosef (Eczacibashi Pharmaceuticals, Turkey), which is available in bottles of 0.5 and 1 g for intramuscular and intravenous administration of each dosage.
Ceftriaxone differs from cefotaxime, another third-generation cephalosporin, by more favorable pharmacokinetic properties:
- long half-life, allowing it to be administered once a day, dose-dependent binding to plasma proteins;
- almost complete bioavailability when administered intramuscularly;
- very good tissue penetration (including through the blood-brain barrier);
- dual path of excretion, and therefore dose adjustment is required only in patients with simultaneous renal and hepatic insufficiency [28, 29].
Ceftriaxone is widely distributed throughout the body, reaching high concentrations in organs and tissues. For more than a day after administration, its concentrations far exceed the minimum inhibitory (MIC) for most sensitive microorganisms in more than 60 tissues and fluids, including the lungs and pleural fluid [30].
A wide spectrum of antibacterial activity, favorable pharmacokinetic properties, good tolerability and ease of use of ceftriaxone have made it, despite the parenteral route of administration, one of the most widely used antibiotics for the treatment of respiratory tract infections not only in hospitalized but also outpatients. In some countries, such as Italy, ceftriaxone is one of the most widely used antibiotics [31].
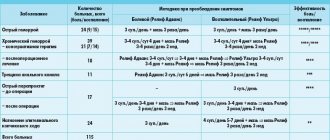
Ceftriaxone is highly effective against community-acquired pneumonia. In the recommendations of the All-Russian Society of Pulmonologists for the treatment of community-acquired pneumonia, it is considered as the drug of choice in hospitalized patients with both mild and severe cases of this disease [32]. In the latter case, ceftriaxone is recommended to be combined with macrolides. The place given to ceftriaxone in the treatment of community-acquired pneumonia in Russia is presented in Tables 1–3.
A significant place is given to third-generation cephalosporins, in particular ceftriaxone, in the updated version of the recommendations for the management of community-acquired pneumonia of the Infectious Diseases Society of America (IDSA), published in 2003 [34]. In combination with modern macrolides, it is recommended for patients hospitalized in the general ward, as well as for patients hospitalized in the intensive care unit, if they do not have risk factors for infection with P. aeruginosa
.
If the etiology of the disease is established, ceftriaxone is the drug of choice for infection caused by Escherichia coli
,
Haemophilus influenzae
, penicillin-resistant
S. pneumoniae
and strains of Klebsiella pneumoniae that do not produce extended-spectrum beta-lactamases [23].
In a number of countries (USA, Canada, Italy, etc.), ceftriaxone is widely used at home in the treatment of patients with severe pneumonia [35, 36]. This allows for excellent clinical results and high patient and physician satisfaction [35]. In addition, due to its ease of use, ceftriaxone is the drug of choice for the treatment of pneumonia in outpatients who, for whatever reason, cannot take antibiotics orally [32].
The effectiveness of ceftriaxone (as monotherapy or combination with other antibiotics) for community-acquired pneumonia of varying severity in adult patients and children has been shown in foreign and domestic clinical studies [35–42]. According to the results of an analysis of literature data on the use of ceftriaxone for lower respiratory tract infections (515 patients with pneumonia and 312 with other infections), published in 1987, the clinical effectiveness of the drug was 96%, bacteriological - 88% [43]. Side effects were observed in 4.6% of patients.
In another retrospective study of 1032 patients aged 16–100 years (mean age 71.9 years) with lower respiratory tract infections, ceftriaxone was the most effective (85.4%) of all antibiotics used [44]. The high efficacy and good tolerability of ceftriaxone in serious, difficult-to-treat community-acquired infections, including pneumonia, meningitis and acute otitis media (including those caused by strains with reduced sensitivity to beta-lactam antibiotics), was confirmed by the results of a recent analysis of randomized clinical trials. research [45].
Ceftriaxone is also widely used for the treatment of nosocomial pneumonia. Experts from the Commission on Antibiotic Policy under the Ministry of Health of Russia and the Russian Academy of Medical Sciences recommend its empirical prescription for pneumonia that developed in general departments in patients without risk factors (i.e., without previous antibiotic therapy or prophylaxis), and for “early” ventilator-associated pneumonia that occurred in patients in intensive care units [46].
The use of ceftriaxone may be limited by two factors: its relatively high price and the risk of the emergence and spread of antibiotic-resistant microorganisms. As for price, firstly, as mentioned above, the cost of an antibiotic for many respiratory tract infections is only a small part of the total cost of treatment. Secondly, the cost of parenteral drug therapy consists of the cost of a course dose of an antibiotic and the so-called “hidden” costs associated with its preparation and administration (solvents, syringes, needles, infusion systems, consumables, etc.), as well as the cost working hours of medical personnel.
A number of foreign pharmacoeconomic studies have shown that the costs associated with the preparation and administration of the drug can be equal to the cost of the drug itself or even exceed it [47]. The share of “hidden” costs in the total cost of treatment decreases with decreasing frequency of drug administration and is minimal with one injection per day [47]. In comparative pharmacoeconomic studies, the “hidden” costs of a single dose of ceftriaxone were 17–52% lower than those of short-acting antibiotics intended for 3–6 doses [48]. As a result, the cost of a course of treatment with ceftriaxone may be lower than the cost of a course of treatment with cheaper antibiotics - cefazolin, cefuroxime and cefotaxime [48, 49].
The higher clinical and/or cost effectiveness of ceftriaxone in patients with lower respiratory tract infections compared to second generation cephalosporins and cefotaxime has been shown in a number of foreign studies [50–53]. A study conducted in 9 therapeutic departments of Northern and Central Italy demonstrated that the use of ceftriaxone in patients with pneumonia and bronchopneumonia saves the hospital 15.18% of financial resources compared to the use of other third-generation cephalosporins and 14.76% compared to the use of broad-spectrum penicillins [53].
A Russian pharmacoeconomic study in elderly and senile patients with community-acquired pneumonia revealed an advantage of the ceftriaxone–amoxicillin/clavulanate regimen over a number of other antibiotics [42]. In moderate cases of the disease, this regimen was superior in cost effectiveness (cost-effectiveness ratio 42.3) to ampicillin (63.9, p
In patients with severe pneumonia, a Russian pharmacoeconomic analysis also confirmed the justification of using the ceftriaxone–amoxicillin/clavulanonate regimen, especially considering its high clinical efficacy (84.2%) and safety [42].
The cost of ceftriaxone treatment can be reduced by step therapy. A number of studies in adults and children with lower respiratory tract infections have shown the effectiveness of stepwise therapy, in which ceftriaxone was used at the first stage, and when the condition normalized, they switched to an oral cephalosporin - ceftibuten, cefpodoxime proxetil, cefetameta pivoxil [54–56]. Not inferior in clinical effectiveness to parenteral therapy, stepwise therapy made it possible to reduce the length of hospital stay and reduce treatment costs. For example, in one study, step therapy resulted in savings per patient of US$46.05 [55].
The use of ceftriaxone in severely ill patients on an outpatient basis reduces treatment costs by an average of 68–78% [57]. Interestingly, in Italy, where the practice of home treatment of various infections requiring parenteral antibiotic administration is widespread, and where ceftriaxone is used per capita much more often than in other countries, the level of bacterial resistance is lower than in the United States and most European countries [58].
Thus, during the 20 years that ceftriaxone has been on the global pharmaceutical market, its importance in the treatment of pneumonia not only does not decrease, but, on the contrary, increases.
Comparison of addiction between Cefotaxime and Ceftriaxone
Like safety, addiction also involves many factors that must be considered when evaluating a drug.
So, the totality of the values of such parameters as “syndrome o” in Cefotaxime is quite similar to the similar values in Ceftriaxone. Withdrawal syndrome is a pathological condition that occurs after the cessation of intake of addictive or dependent substances into the body. And resistance is understood as initial immunity to a drug; in this it differs from addiction, when immunity to a drug develops over a certain period of time. The presence of resistance can only be stated if an attempt has been made to increase the dose of the drug to the maximum possible. At the same time, Cefotaxime has a fairly low incidence of “syndrome”, just like Ceftriaxone.
Resistance problems
Third generation cephalosporins are powerful antibacterial drugs used to treat life-threatening infections. However, in recent years, resistance to these drugs has been increasingly reported, especially among members of Enterobacteriaceae (Kozlov et al., 2008), due to the continued spread of ESBLs. Numerous publications report the widespread spread of antibiotic resistance and the identification of pathogenic microorganisms resistant to all available antibacterial drugs (Bereznyakov, 2006, 2012). Multidrug-resistant (MDR) bacteria are no longer found only in hospitals, but also in community settings. Hydrolysis of blactam antibiotics by blactamases is the main mechanism of resistance to this class of antimicrobial agents in clinically important Gram-negative bacteria.
ESBLs are known to hydrolyze oxyiminocephalosporins (cefotaxime, ceftazidime, ceftriaxone, cefuroxime and cefepime) and monobactams (aztreonam), but not cephamycins (cefoxitin, cefotetan) or carbapenems. ESBLs are usually localized on large plasmids. Although the ability to produce ESBLs has been documented in many members of the family Enterobacteriaceae and P.aeruginosa, at the end of the last century ESBL production was most often observed in Klebsiella spp. In recent years, E. coli has become increasingly important among ESBL producers.
Comparison of side effects of Cefotaxime and Ceftriaxone
Side effects or adverse events are any adverse medical event that occurs in a subject after administration of a drug.
Cefotaxime has more adverse effects than Ceftriaxone. This implies that the incidence is low for Cefotaxime and low for Ceftriaxone. Frequency of manifestation is an indicator of how many cases of an undesirable effect from treatment are possible and registered. The undesirable effect on the body, the strength of influence and the toxic effect of drugs are different: how quickly the body recovers after taking it and whether it recovers at all. When using Cefotaxime, the body's ability to recover faster is higher than that of Ceftriaxone.
conclusions
Rational therapy of pulmonary infections is a difficult problem today due to the difficulty of verifying microbiological diagnosis and the increasing frequency of resistant microflora. The combined drug Sulbactomax seems to be a reasonable, significantly more effective alternative to unprotected cephalosporins in the treatment of patients with CAP of groups II, III and IV, both adults and children. The inhibitor-protected ceftriaxone Sulbactomax expands the medical arsenal in the treatment of problem patients, in particular with severe community-acquired and nosocomial pneumonia caused by ESBL producers.
Prepared by Konstantin Kremets
Comparison of ease of use of Cefotaxime and Ceftriaxone
This includes dose selection taking into account various conditions and frequency of doses. At the same time, it is important not to forget about the release form of the drug; it is also important to take it into account when making an assessment.
The ease of use of Cefotaxime is approximately the same as that of Ceftriaxone. However, they are not convenient enough to use.
The drug ratings were compiled by experienced pharmacists who studied international research. The report is generated automatically.
Last update date: 2020-12-04 13:48:30
When the doctor is faced with a choice - Cefepime or Ceftriaxone
The need to choose one of the cephalosporin antibiotics - Cefepime or Ceftriaxone - occurs when there is a bacterial infection:
- pneumonia;
- accumulation of pus in the pleura (empyema);
- acute bronchitis or exacerbation of chronic bronchitis with severe course;
- complicated forms of inflammation of the urinary tract (purulent urethritis, cystitis, pyelonephritis);
- suppuration of the skin and subcutaneous tissue;
- inflammation of bone tissue or joints caused by bacteria;
- in the abdominal cavity (peritonitis);
- inflammatory process in the pelvic organs (severe prostatitis, adnexitis, endometritis);
- salmonellosis;
- meningitis (inflammation of the vascular membranes of the brain);
- blood poisoning (sepsis);
- purulent-inflammatory diseases in patients with reduced immunity.
Since both drugs have a wide spectrum of antimicrobial action and only an injection form, they are used for severe or moderate infectious diseases.
Cefepime and Ceftriaxone should not be used without a doctor's prescription, since it is important not only to know the name of the antibiotic, but also to accurately select the dose. If it is lower than necessary, then instead of destroying bacteria, they become resistant to their introduction. When using large quantities and a long course, the risk of complications increases significantly.
We recommend reading about the rules for using Ceftriaxone for pneumonia. From the article you will learn about the mechanism of action of the antibiotic for pneumonia, the course of treatment with Ceftriaxone in children and adults, and what it can be combined with. And here is more information about Ceftriaxone analogues.
Contraindications
General contraindications for these drugs are intolerance to:
- active ingredients (cefepime hydrochloride or ceftriaxone), ;
- other cephalosporins;
- penicillins;
- carbapenems (for example, Meronem).
They are used with caution in cases of previously suffered intestinal inflammation after the administration of any antibiotics (drug-induced colitis, dysbacteriosis), lactation, severe kidney failure, liver failure.
Cefepime should not be prescribed to children under 1 month of age, in the first trimester of pregnancy and in individuals with high sensitivity to the amino acid arginine. Ceftriaxone is prohibited for use in newborns under the following conditions:
- age up to 41 weeks, including the period of intrauterine development;
- increased blood bilirubin, jaundice;
- the need for droppers with calcium salts;
- a shift in the blood reaction to the acidic side.
Rules for preparing injections
To prepare a solution of Ceftriaxone for injection into the muscle, you need to take 4 ml of 1% Lidocaine or 2 ml of water for injection and 2% Lidocaine per 1 g of powder. The solvent is injected into the vial with a syringe and shaken until the solution is completely transparent.
For intravenous injections, 10 ml of saline solution is taken per 1 g of Ceftriaxone. If it is necessary to place a dropper, then 2 g of the medication is dissolved in 40 ml of a calcium-free solution:
- 0.9% sodium chloride,
- 5% glucose,
- 6% Voluven.
For Cefepime, the predominant route of administration is intravenous. For injection, add saline solution or 5% glucose in a volume of 10 ml per 1 g of the drug. If it is necessary to carry out an infusion, then take the resulting antibiotic solution for a dropper and adjust the amount of solvent to 50-100 ml. For intramuscular injections, you need to add 2.5 ml of saline solution, water for injection or 1% Lidocaine per 1 g of Cefepime.