Artificial respiration (AR) is an urgent emergency measure if a person’s own breathing is absent or impaired to such an extent that it poses a threat to life. The need for artificial respiration may arise when providing assistance to those who have received sunstroke, drowned, suffered from electric current, as well as in case of poisoning with certain substances.
The purpose of the procedure is to ensure the process of gas exchange in the human body, in other words, to ensure sufficient saturation of the victim’s blood with oxygen and the removal of carbon dioxide from it. In addition, artificial ventilation has a reflex effect on the respiratory center located in the brain, as a result of which independent breathing is restored.
Mechanism and methods of artificial respiration
Content:
- Mechanism and methods of artificial respiration
- Indications and contraindications
- Preparing for artificial respiration
- Artificial respiration from mouth to mouth
- Artificial respiration from mouth to nose
- How long does artificial respiration last?
- Features of the procedure in children
- Manual methods of artificial respiration
- Hardware artificial respiration methods
- Complications of artificial respiration
Only through the process of breathing does a person’s blood become saturated with oxygen and carbon dioxide is removed from it. After air enters the lungs, it fills the lung sacs called alveoli. The alveoli are pierced by an incredible number of small blood vessels. It is in the pulmonary vesicles that gas exchange takes place - oxygen from the air enters the blood, and carbon dioxide is removed from the blood.
If the body's supply of oxygen is interrupted, vital activity is at risk, since oxygen plays the “first fiddle” in all oxidative processes that occur in the body. That is why, when breathing stops, artificially ventilating the lungs should be started immediately.
The air entering the human body during artificial respiration fills the lungs and irritates the nerve endings in them. As a result, nerve impulses are sent to the respiratory center of the brain, which are a stimulus for the production of response electrical impulses. The latter stimulate contraction and relaxation of the diaphragm muscles, resulting in stimulation of the respiratory process.
Artificially supplying the human body with oxygen in many cases makes it possible to completely restore the independent respiratory process. In the event that cardiac arrest is also observed in the absence of breathing, it is necessary to perform a closed cardiac massage.
Please note that the absence of breathing triggers irreversible processes in the body within five to six minutes. Therefore, timely artificial ventilation can save a person’s life.
All methods of performing ID are divided into expiratory (mouth-to-mouth and mouth-to-nose), manual and hardware. Manual and expiratory methods are considered more labor-intensive and less effective compared to hardware methods. However, they have one very significant advantage. They can be performed without delay, almost anyone can cope with this task, and most importantly, there is no need for any additional devices and instruments, which are not always at hand.
Sudden cardiac arrest on the street: what to do before the ambulance arrives?
Resuscitation measures are carried out after establishing a state of clinical death, the main signs of which are: absent breathing and heartbeat, unconsciousness, dilated pupils, lack of response to external stimuli. To reliably determine the severity of the situation, it is necessary to determine the following indicators of the victim:
- check the pulse in the carotid arteries of the neck at the jaw angle - when the pressure drops to less than 60-50 mm Hg. Art. the pulse on the radial artery of the inner surface of the hand is not detected;
- examine the chest, check for spontaneous breathing movements;
- approach the victim’s face to check breathing, determine inhalation and exhalation (air movement assessment);
- pay attention to the color of the skin - cyanosis and severe pallor appear when breathing stops;
- check consciousness - lack of response to stimuli indicates coma.
Cardiopulmonary resuscitation according to the new standards is carried out only in two cases. You should start performing CPR only after determining your pulse and breathing.
If the pulse is clearly detected for 10-15 seconds and atonal breathing is disturbed with episodes of convulsive sighs, artificial respiration is required. To do this, you need to take 10-12 breaths “mouth to mouth” or “mouth to nose” over the course of a minute. While waiting for an ambulance, you need to measure your pulse every minute; if it is absent, CPR is indicated.
If spontaneous breathing and pulse fail, a set of resuscitation measures is indicated strictly according to the algorithm.
Consciousness testing is carried out according to the following principle:
- Address the victim loudly. Ask what happened and how he feels.
If there is no response, use painful stimuli. Pinch the top edge of the trapezius muscle or apply pressure at the base of the nose.- If there is no reaction (speech, twitching, attempts to defend yourself with your hand) - there is no consciousness, you can move on to the next stage.
Breath test:
- Tilt your head back (holding it by the back of your head and chin) and open your mouth. Inspect it for foreign bodies. If they are there, remove them.
- Bend towards your face and for 10 seconds. check your breathing. You should feel it with your cheek and hear and see the movements of your chest. Normally, 2-3 breaths are sufficient.
- If there is no breathing or only 1 breath is felt (which can be considered its absence), we can assume the cessation of a vital function.
In such a case, it is necessary to call an ambulance and begin performing resuscitation measures in case of cardiac and respiratory arrest.
Indications and contraindications
Indications for the use of ID are all cases where the volume of spontaneous ventilation of the lungs is too low to ensure normal gas exchange. This can happen in many urgent and planned situations:
- For disorders of the central regulation of breathing caused by impaired cerebral circulation, tumor processes of the brain or brain injury.
- For medicinal and other types of intoxication.
- In case of damage to the nerve pathways and neuromuscular synapse, which can be caused by trauma to the cervical spine, viral infections, the toxic effect of certain medications, and poisoning.
- For diseases and damage to the respiratory muscles and chest wall.
- In cases of lung lesions of both obstructive and restrictive nature.
The need to use artificial respiration is judged based on a combination of clinical symptoms and external data. Changes in pupil size, hypoventilation, tachy- and bradysystole are conditions that require artificial ventilation. In addition, artificial respiration is required in cases where spontaneous ventilation is “turned off” with the help of muscle relaxants administered for medical purposes (for example, during anesthesia for surgery or during intensive care for a seizure disorder).
As for cases where ID is not recommended, there are no absolute contraindications. There are only prohibitions on the use of certain methods of artificial respiration in a particular case. So, for example, if venous return of blood is difficult, artificial respiration modes are contraindicated, which provoke even greater disruption. In case of lung injury, ventilation methods based on high-pressure air injection, etc., are prohibited.
Invasive ventilation
An endotracheal tube is inserted into the trachea through the mouth or nose and connected to a ventilator.
With invasive respiratory support, the ventilator provides forced pumping of oxygen to the lungs and completely takes over the breathing function. The gas mixture is supplied through an endotracheal tube placed into the trachea through the mouth or nose. In particularly critical cases, tracheostomy is performed - a surgical operation to dissect the anterior wall of the trachea to insert a tracheostomy tube directly into its lumen.
Invasive ventilation is highly effective, but is used only if it is impossible to help the patient in a more gentle way, i.e. without invasive intervention.
Who needs invasive ventilation and when?
A person connected to a ventilator can neither speak nor eat. Intubation is not only inconvenient, but also painful. Because of this, the patient is usually placed in a medically induced coma. The procedure is carried out only in a hospital setting under the supervision of specialists.
Invasive ventilation is highly effective, but intubation involves placing the patient in a medically induced coma. In addition, the procedure is associated with risks.
Traditionally, invasive respiratory support is used in the following cases:
- lack of effect or intolerance of NIV in the patient;
- increased drooling or production of excessive sputum;
- emergency hospitalization and the need for immediate intubation;
- coma or impaired consciousness;
- possibility of respiratory arrest;
- presence of trauma and/or burns to the face.
How does an invasive ventilator work?
The operating principle of devices for invasive ventilation can be described as follows.
- For short-term mechanical ventilation, an endotracheal tube is inserted into the patient's trachea through the mouth or nose. For long-term mechanical ventilation, an incision is made in the patient's neck, the anterior wall of the trachea is dissected, and a tracheostomy tube is placed directly into its lumen.
- A breathing mixture is delivered through a tube into the lungs. The risk of air leakage is minimized, so the patient is guaranteed to receive the right amount of oxygen.
- The patient's condition can be monitored using monitors that display breathing parameters, the volume of supplied air mixture, saturation, cardiac activity, and other data.
Features of equipment for invasive ventilation
Equipment for invasive ventilation has a number of characteristic features.
- Completely takes over the breathing function, i.e. actually breathes instead of the patient.
- It requires regular checking of the serviceability of all valves, because... The patient’s life depends on the performance of the system.
- The procedure must be supervised by a doctor. Weaning the patient from the ventilator also requires the participation of a specialist.
- Used with additional accessories - humidifiers, cough cleaners, spare circuits, suction units, etc.
Preparing for artificial respiration
Before performing expiratory artificial respiration, the patient should be examined. Such resuscitation measures are contraindicated for facial injuries, tuberculosis, polio and trichlorethylene poisoning. In the first case, the reason is obvious, and in the last three, performing expiratory artificial respiration puts the person performing resuscitation at risk.
Before starting expiratory artificial respiration, the victim is quickly freed from clothing squeezing the throat and chest. The collar is unbuttoned, the tie is undone, and the trouser belt can be unfastened. The victim is placed supine on his back on a horizontal surface. The head is tilted back as much as possible, the palm of one hand is placed under the back of the head, and the other palm is pressed on the forehead until the chin is in line with the neck. This condition is necessary for successful resuscitation, since with this position of the head the mouth opens and the tongue moves away from the entrance to the larynx, as a result of which air begins to flow freely into the lungs. In order for the head to remain in this position, a cushion of folded clothing is placed under the shoulder blades.
After this, it is necessary to examine the victim’s oral cavity with your fingers, remove blood, mucus, dirt and any foreign objects.
It is the hygienic aspect of performing expiratory artificial respiration that is the most delicate, since the rescuer will have to touch the victim’s skin with his lips. You can use the following technique: make a small hole in the middle of a handkerchief or gauze. Its diameter should be two to three centimeters. The fabric is placed with a hole on the victim’s mouth or nose, depending on which method of artificial respiration will be used. Thus, air will be blown through the hole in the fabric.
Artificial respiration from mouth to mouth
To perform artificial respiration using the mouth-to-mouth method, the person who will provide assistance must be on the side of the victim’s head (preferably on the left side). In a situation where the patient is lying on the floor, the rescuer kneels. If the victim's jaws are clenched, they are forced apart.
After this, one hand is placed on the victim’s forehead, and the other is placed under the back of the head, tilting the patient’s head back as much as possible. Having taken a deep breath, the rescuer holds the exhalation and, bending over the victim, covers the area of his mouth with his lips, creating a kind of “dome” over the patient’s mouth. At the same time, the victim’s nostrils are pinched with the thumb and index finger of the hand located on his forehead. Ensuring tightness is one of the prerequisites for artificial respiration, since air leakage through the victim’s nose or mouth can nullify all efforts.
After sealing, the rescuer quickly, forcefully exhales, blowing air into the airways and lungs. The duration of exhalation should be about a second, and its volume should be at least a liter for effective stimulation of the respiratory center to occur. At the same time, the chest of the person receiving assistance should rise. If the amplitude of its rise is small, this is evidence that the volume of air supplied is insufficient.
Exhaling, the rescuer unbends, freeing the victim's mouth, but at the same time keeping his head thrown back. The patient should exhale for about two seconds. During this time, before taking the next breath, the rescuer must take at least one normal breath “for himself”.
Please note that if a large amount of air enters the patient's stomach rather than the lungs, this will significantly complicate his rescue. Therefore, you should periodically press on the epigastric region to empty the stomach of air.
Artificial respiration from mouth to nose
This method of artificial ventilation is carried out if it is not possible to properly unclench the patient’s jaws or there is an injury to the lips or oral area.
The rescuer places one hand on the victim’s forehead and the other on his chin. At the same time, he simultaneously throws back his head and presses his upper jaw to the lower. With the fingers of the hand that supports the chin, the rescuer must press the lower lip so that the victim’s mouth is completely closed. Taking a deep breath, the rescuer covers the victim’s nose with his lips and forcefully blows air through the nostrils, while watching the movement of the chest.
After artificial inspiration is completed, you need to free the patient's nose and mouth. In some cases, the soft palate may prevent air from escaping through the nostrils, so when the mouth is closed, there may be no exhalation at all. When exhaling, the head must be kept tilted back. The duration of artificial exhalation is about two seconds. During this time, the rescuer himself must take several exhalations and inhalations “for himself.”
How long does artificial respiration last?
There is only one answer to the question of how long ID should be carried out. You should ventilate your lungs in this mode, taking breaks for a maximum of three to four seconds, until full spontaneous breathing is restored, or until the doctor appears and gives other instructions.
At the same time, you should constantly ensure that the procedure is effective. The patient's chest should swell well, and the facial skin should gradually turn pink. It is also necessary to ensure that there are no foreign objects or vomit in the victim’s respiratory tract.
Please note that due to the ID, the rescuer himself may experience weakness and dizziness due to a lack of carbon dioxide in the body. Therefore, ideally, air blowing should be done by two people, who can alternate every two to three minutes. If this is not possible, the number of breaths should be reduced every three minutes so that the person performing resuscitation normalizes the level of carbon dioxide in the body.
During artificial respiration, you should check every minute to see if the victim’s heart has stopped. To do this, use two fingers to feel the pulse in the neck in the triangle between the windpipe and the sternocleidomastoid muscle. Two fingers are placed on the lateral surface of the laryngeal cartilage, after which they are allowed to “slide” into the hollow between the sternocleidomastoid muscle and the cartilage. This is where the pulsation of the carotid artery should be felt.
If there is no pulsation in the carotid artery, chest compressions in combination with ID should be started immediately. Doctors warn that if you miss the moment of cardiac arrest and continue to perform artificial ventilation, it will not be possible to save the victim.
Cardiopulmonary resuscitation: instructions for carrying out
How to perform cardiopulmonary resuscitation yourself?
Each of us hopes that he will not have to carry out resuscitation measures or provide emergency medical care to the victim, but no one is immune from such cases.
In emergency situations, first aid must be provided very quickly and correctly. Only then is there a chance for a person to return to life. Although almost all of us have some knowledge regarding first aid, in most cases it is a strange mixture of stereotypes that are completely inapplicable in practice. For example, everyone has an idea of what chest compressions and artificial respiration are. However, not everyone knows in what situation cardiopulmonary resuscitation is necessary and how to carry it out correctly.
What it is? Cardiopulmonary resuscitation is a set of measures aimed at returning a person to life in the event of circulatory or respiratory arrest.
In general, all activities can be divided into two large groups - basic and specialized cardiopulmonary resuscitation (CPR).
Specialized, as the name suggests, is carried out in specialized wards and requires appropriate equipment and medications, as well as education. Here we will consider only basic resuscitation issues.
When is CPR necessary? Indications for CPR: absence of consciousness, breathing, pulse in the carotid arteries, preagonal, agonal states, clinical death.
If the heartbeat is heard, the pulse and breathing are preserved and even quite rhythmic, resuscitation measures are not required.
Basic cardiopulmonary resuscitation includes three stages (ABC):
- ensuring airway patency (A - Airway);
- performing artificial respiration (B - Breathing);
- performing indirect cardiac massage (C - Circulation).
In practice, there is a universal algorithm of actions for sudden death of adults, which includes all these stages in sequence.
Assessing the presence of consciousness in the victim First, it is necessary to assess the presence of injury, especially to the head or neck - if injury is suspected, it is possible to move the victim only if absolutely necessary. After this, you can pat or lightly shake him by the shoulders, while loudly asking a question like: “Are you okay?”
Ensuring airway conduction, assessing spontaneous breathing
First, the victim must be laid flat on his back on a hard, flat surface. At the same time, it must be rotated “as a single whole,” without allowing parts of the body to move relative to each other or rotate.
The second is to empty the mouth of liquid contents (with the index and middle fingers wrapped in a piece of cloth) and solid foreign bodies (with the bent index finger). Then ensure the patency of the upper respiratory tract by throwing back the head and lifting the chin or pushing the lower jaw forward. If there is a suspicion of head or neck injury, only the mandible is moved forward.
Third, put your ear to the victim’s mouth and nose and evaluate the movements of the chest during inhalation and exhalation, the presence of the sound of exhaled air and the sensation of air movement (the assessment should take no more than 10 seconds).
Fourth, if after ensuring the airway is clear, breathing is restored and there are signs of blood circulation, the victim should be turned on his side and his head should be placed so that fluid can flow freely from the mouth.
If there is no breathing, the next stage should begin - artificial respiration. In the absence of special equipment (for example, an Ambu bag), the most effective is mouth-to-mouth breathing, which is carried out immediately after ensuring the airway is open.
The main disadvantage of this method is the presence of a psychological barrier - it is difficult to force yourself to breathe into the mouth or nose of another, sometimes a stranger and stranger, especially if he has previously vomited.
With your left hand, holding the victim’s head in an tilted position, at the same time cover the nasal passages with your fingers to ensure tightness. Next, you need to take a deep breath, wrap your lips around the victim’s mouth, and inhale. Cover your mouth with any clean cloth beforehand for hygienic purposes.
This procedure should be repeated at a frequency of 10-12 breathing cycles per minute (once every 5-6 seconds). Passive exhalation should be complete (time does not matter); the next air injection can be done when the chest has dropped.
The main criterion for the effectiveness of artificial respiration is the movement of the chest during inhalation and exhalation, the sound of exhaled air and the sensation of its movement. If this is not observed, the airway should be re-cleared and the airway should be checked for obstruction (eg by a foreign body) at the level of the larynx.
If signs of spontaneous breathing appear in the victim, artificial ventilation of the lungs is not stopped immediately, it is continued until the number of spontaneous breaths corresponds to 12-15 per minute. At the same time, if possible, synchronize the rhythm of inhalations with the recovery breathing of the victim.
Assessment of blood circulation It is carried out in parallel with artificial respiration - it is necessary to determine the pulsation in the carotid or femoral arteries. Easier and better for sleep - light pressure with two or three fingers in the hole between the lateral surface of the larynx and the muscle roll on the lateral surface of the neck.
In addition, non-professional rescuers are recommended to be additionally guided by indirect signs - breathing, coughing, movements of the victim in response to artificial respiration (the assessment should take no more than 10-15 seconds).
After making sure that the patient has no cardiac activity, it is necessary to begin performing indirect (closed) cardiac massage. The rescuer’s hands are located on the victim’s sternum 2-3 cm above the xiphoid process - the part of the sternum located below the place where the cartilage of the X ribs is attached to it. The hands are placed one on top of the other (“locked”) in the lower third of the sternum.
Before starting chest compressions, you should carry out 2-3 intense blows of air into the victim’s lungs and strike with your fist in the area of the projection of the heart (precordial blow). This is sometimes enough for the heart to “start working” again, while “hitting with all your might” on the sternum is unnecessary and dangerous, you could easily break a person’s ribs. After this, chest compressions begin in the anteroposterior direction by 2.5-5 cm with a frequency of 80-100 times per minute.
The forces are applied strictly vertically to the lower third of the sternum using crossed wrists and arms straightened at the elbows, without touching the chest with the fingers. Compression and cessation of compression should take equal time; when the compression stops, the hands do not leave the chest.
Simultaneous artificial respiration and closed cardiac massage If spontaneous breathing is absent during the first examination, two breaths are first taken, and their effectiveness is simultaneously assessed.
Then, if one person is performing resuscitation, 15 chest compressions should be alternated with two breaths, if two people - 5 chest compressions should be alternated with one breath, stopping chest compressions for 1-2 seconds while blowing air into the lungs.
Mouth-to-mouth breathing is dangerous for the rescuer and can cause infection. It is believed that indirect cardiac massage can be performed without artificial ventilation of the lungs - if there are no special devices for artificial respiration: an Ambu bag, a ventilator, etc. However, this technique is less effective, and if possible, you should still opt for artificial respiration.
Monitoring the victim's condition during resuscitation After every 4 cycles of artificial respiration and chest compressions, you need to check the pulse in the carotid artery (within 3-5 seconds). If a pulse appears, chest compressions should be stopped and spontaneous breathing assessed.
If it is absent, you need to continue artificial respiration while simultaneously determining the pulsation in the carotid artery after every 10 blows of air into the lungs.
When spontaneous breathing is restored and there is no consciousness, it is necessary to maintain the patency of the upper respiratory tract and carefully monitor the presence of breathing and pulsation in the carotid artery until the arrival of the resuscitation team.
Irreversible changes in the brain occur 3-4 minutes after circulatory arrest, which is why early help and the start of resuscitation measures are of great importance. Refusal to use resuscitation measures or their cessation is permissible only if biological death is established or these measures are recognized as absolutely futile.
In parallel with resuscitation efforts (without interrupting them), you need to call an ambulance and diagnose the victim’s condition.
Features of the procedure in children
When performing artificial ventilation for babies under one year of age, the mouth-to-mouth and nose technique is used. If the child is older than one year, the mouth-to-mouth method is used.
Small patients are also placed on their back. For babies under one year old, place a folded blanket under their back or slightly raise their upper body, placing a hand under their back. The head is thrown back.
The person providing assistance takes a shallow breath, seals her lips around the child’s mouth and nose (if the baby is under one year old) or just the mouth, and then blows air into the respiratory tract. The volume of air blown in should be less, the younger the patient. So, in the case of resuscitation of a newborn, it is only 30-40 ml.
If a sufficient volume of air enters the respiratory tract, chest movement occurs. After inhaling, you need to make sure that the chest drops. If you blow too much air into your baby's lungs, this can cause the alveoli of the lung tissue to rupture, causing air to escape into the pleural cavity.
The frequency of insufflations should correspond to the breathing frequency, which tends to decrease with age. Thus, in newborns and children up to four months, the frequency of inhalations and exhalations is forty per minute. From four months to six months this figure is 40-35. In the period from seven months to two years - 35-30. From two to four years it is reduced to twenty-five, in the period from six to twelve years - to twenty. Finally, in a teenager aged 12 to 15 years, the respiratory rate is 20-18 breaths per minute.
Emergency assistance from the medical team: what is the algorithm of action?
To provide emergency care in case of sudden cardiac arrest, a special cardiology team arrives on site, whose task is to carry out advanced resuscitation measures and immediately transport the patient to the hospital. It works according to a protocol that includes the following sequence of actions:
- Checking vital signs and making a diagnosis. For this purpose, a wider arsenal of equipment is used, including an electrocardiograph. It is necessary to exclude other causes of clinical death, such as bleeding or blockage.
Resumption of conductivity of the upper respiratory tract. To ensure maximum oxygen supply, they are intubated.- Resuscitation measures are carried out according to the same algorithm as indicated above, but for mechanical ventilation they use breathing masks, an Ambu bag or a ventilator.
- In the presence of atrial fibrillation or ventricular fibrillation on the ECG, the question of using defibrillation is raised.
- Drug support is provided by intravenous or intracardiac administration of drugs such as Adrenaline (1 ml 0.1% in 19 ml NaCl 0.9%) and Cordarone (in the presence of arrhythmias, 300 mg IV).
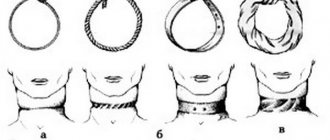
Manual methods of artificial respiration
There are also so-called manual methods of artificial respiration. They are based on changing the volume of the chest due to the application of external force. Let's look at the main ones.
Sylvester's method
This method is most widely used. The victim is placed on his back. A cushion should be placed under the lower part of the chest so that the shoulder blades and the back of the head are lower than the costal arches. In the event that artificial respiration is performed using this method by two people, they kneel on either side of the victim so as to be positioned at the level of his chest. Each of them holds the victim’s hand in the middle of the shoulder with one hand, and with the other just above the level of the hand. Next, they begin to rhythmically raise the victim’s arms, stretching them behind his head. As a result, the chest expands, which corresponds to inhalation. After two or three seconds, the victim’s hands are pressed to the chest, while squeezing it. This performs the functions of exhalation.
In this case, the main thing is that the movements of the hands are as rhythmic as possible. Experts recommend that those performing artificial respiration use their own rhythm of inhalation and exhalation as a “metronome”. In total, you should do about sixteen movements per minute.
ID using the Sylvester method can be performed by one person. He needs to kneel behind the victim’s head, grab his arms above the hands and perform the movements described above.
For broken arms and ribs, this method is contraindicated.
Schaeffer method
If the victim's arms are injured, the Schaeffer method can be used to perform artificial respiration. This technique is also often used for the rehabilitation of people injured while on the water. The victim is placed prone, with his head turned to the side. The one who performs artificial respiration kneels, and the victim’s body should be located between his legs. Hands should be placed on the lower part of the chest so that the thumbs lie along the spine and the rest rest on the ribs. When exhaling, you should lean forward, thus compressing the chest, and while inhaling, straighten, stopping the pressure. The elbows are not bent.
Please note that this method is contraindicated for fractured ribs.
Laborde method
The Laborde method is complementary to the Sylvester and Schaeffer methods. The victim's tongue is grabbed and rhythmically stretched, imitating breathing movements. As a rule, this method is used when breathing has just stopped. The resistance of the tongue that appears is evidence that the person’s breathing is being restored.
Kallistov method
This simple and effective method provides excellent ventilation. The victim is placed prone, face down. A towel is placed on the back in the area of the shoulder blades, and its ends are passed forward, threaded under the armpits. The person providing assistance should take the towel by the ends and lift the victim’s torso seven to ten centimeters from the ground. As a result, the chest expands and the ribs rise. This corresponds to inhalation. When the torso is lowered, it simulates exhalation. Instead of a towel, you can use any belt, scarf, etc.
Howard's method
The victim is positioned supine. A cushion is placed under his back. Hands are moved behind the head and extended. The head itself is turned to the side, the tongue is extended and secured. The one who performs artificial respiration sits astride the victim’s thigh area and places his palms on the lower part of the chest. With your fingers spread, you should grab as many ribs as possible. When the chest is compressed, it simulates inhalation; when the pressure is released, it simulates exhalation. You should do twelve to sixteen movements per minute.
Frank Eve's method
This method requires a stretcher. They are installed in the middle on a transverse stand, the height of which should be half the length of the stretcher. The victim is placed prone on the stretcher, the face is turned to the side, and the arms are placed along the body. The person is tied to the stretcher at the level of the buttocks or thighs. When lowering the head end of the stretcher, inhale; when it goes up, exhale. Maximum breathing volume is achieved when the victim's body is tilted at an angle of 50 degrees.
Nielsen method
The victim is placed face down. His arms are bent at the elbows and crossed, after which they are placed palms down under the forehead. The rescuer kneels at the victim’s head. He places his hands on the victim’s shoulder blades and, without bending them at the elbows, presses with his palms. This is how exhalation occurs. To inhale, the rescuer takes the victim’s shoulders at the elbows and straightens, lifting and pulling the victim towards himself.
Hardware artificial respiration methods
For the first time, hardware methods of artificial respiration began to be used back in the eighteenth century. Even then, the first air ducts and masks appeared. In particular, doctors proposed using fireplace bellows to blow air into the lungs, as well as devices created in their likeness.
The first automatic ID machines appeared at the end of the nineteenth century. At the beginning of the twenties, several types of respirators appeared at once, which created intermittent vacuum and positive pressure either around the entire body, or only around the patient’s chest and abdomen. Gradually, respirators of this type were replaced by air-injection respirators, which had less solid dimensions and did not impede access to the patient’s body, allowing medical procedures to be performed.
Best materials of the month
- Coronaviruses: SARS-CoV-2 (COVID-19)
- Antibiotics for the prevention and treatment of COVID-19: how effective are they?
- The most common "office" diseases
- Does vodka kill coronavirus?
- How to stay alive on our roads?
All ID devices existing today are divided into external and internal. External devices create negative pressure either around the patient's entire body or around his chest, thereby inhaling. Exhalation in this case is passive - the chest simply collapses due to its elasticity. It can also be active if the device creates a positive pressure zone.
With the internal method of artificial ventilation, the device is connected through a mask or intubator to the respiratory tract, and inhalation is carried out by creating positive pressure in the device. Devices of this type are divided into portable, intended for work in “field” conditions, and stationary, the purpose of which is long-term artificial respiration. The former are usually manual, while the latter operate automatically, driven by a motor.
Non-invasive ventilation
Over the past two decades, the use of non-invasive mechanical ventilation equipment has increased markedly. NIV has become a generally accepted and widespread tool for the treatment of acute and chronic respiratory failure both in hospitals and at home.
One of the leading manufacturers of medical respiratory devices is the Australian company ResMed
NIV - what is it?
Non-invasive ventilation refers to mechanical respiratory support without invasive access (ie, without an endotracheal or tracheostomy tube) using various known assisted ventilation modes.
The equipment supplies air to the patient interface through a breathing circuit. To provide NIV, various interfaces are used - nasal or oro-nasal mask, helmet, mouthpiece. Unlike the invasive method, the person continues to breathe on his own, but receives hardware support during inspiration.
When is non-invasive ventilation used?
The key to successful use of noninvasive ventilation is recognition of its capabilities and limitations, as well as careful patient selection (diagnosis and patient assessment). Indications for NIV are the following criteria:
- shortness of breath at rest;
- respiratory rate RR>25, participation of auxiliary respiratory muscles in the respiratory process;
- hypercapnia (PaC02>45 and its rapid increase);
- Ph level
- symptomatic lack of positive effect from oxygen therapy, hypoxemia and gas exchange disorders;
- increase in airway resistance by 1.5-2 times the norm.
To perform non-invasive ventilation, the patient must be conscious and able to follow the instructions of the doctors. There must be a clear prospect of stabilizing the patient within several hours or days after the start of respiratory support. Absolute contraindications for NIV are:
- coma;
- heart failure;
- respiratory arrest;
- any condition requiring immediate intubation.
Advantages of NIV
One of the advantages of non-invasive ventilation is the ability to carry out therapy at home.
Non-invasive ventilation allows you to help a patient with acute or chronic respiratory failure without resorting to endotracheal intubation or tracheostomy. The technique is simpler and more comfortable for the patient. Let us list the main advantages of NIV.
- A respiratory support session is easy to start and just as easy to complete.
- The patient retains the ability to speak, swallow, eat independently, and cough.
- The procedure does not cause complications that are possible with endotracheal intubation and tracheostomy, including mechanical damage to internal organs by the tube, bleeding, swelling of the glottis, infection of the respiratory tract, etc.
- The air passes through the respiratory tract, due to which it is humidified, purified and warmed naturally.
- NIV can be performed at an early stage of the disease, i.e. before the patient's condition becomes critical. This shortens the duration of treatment, reduces the number of complications, and also reduces the risk of readmission.
- In many cases, devices for non-invasive respiratory support can be used not only in a hospital, but also at home.
- There is no “respirator weaning” period after completion of treatment.
Non-invasive conscious ventilation also has some disadvantages and side effects. For example, it is impossible to apply high treatment pressure, because this leads to significant leakage from under the mask. There is no direct access to the respiratory tract, so it is impossible to sanitize it. It is also impossible not to mention the likelihood of aerophagia, aspiration of stomach contents and skin irritation in the areas where the contour is adjacent.
Non-invasive ventilation in CPAP and BIPAP modes
The terms CPAP and BIPAP are often used interchangeably with NIV. These are common methods of non-invasive respiratory support using special portable devices. Many modern ventilators used in intensive care units have the option of CPAP and BIPAP.
Portable respirators are low cost (relative to resuscitation stationary ventilators), and they effectively compensate for even high air leakage. But most often they do not provide advanced monitoring of the patient's condition in real time.
Most resuscitation respirators can operate in CPAP and BIPAP modes. But more often, portable devices are used to provide respiratory support to a conscious patient.
In CPAP (continuous positive airway pressure) mode, the device supplies air under constant positive pressure, and the patient breathes spontaneously (i.e., independently). The method is used in the management of patients with moderate to severe obstructive sleep apnea syndrome (OSA), as well as post-traumatic or postoperative acute respiratory failure.
Bi-level positive airway pressure (BIPAP) devices have a wider range of applications and different mode options. Unlike CPAP, they involve an increase in pressure as you inhale and a decrease in pressure as you exhale. Thanks to this, it becomes possible to use high treatment pressure, but the patient does not experience discomfort in the exhalation phase, overcoming the resistance of the air flow. Two-level ventilation allows you to relieve the respiratory muscles, reduce the respiratory rate and increase the tidal volume. And the presence of auxiliary modes in modern models helps to select the optimal treatment protocol in accordance with the diagnosis and needs of the patient.
CPAP and BIPAP machines to help patients with COVID-19
Over the past few months, the issue of mechanical ventilation has been raised frequently in connection with the COVID-19 pandemic. High demand for ventilators has caused their shortage. The Australian company ResMed, as a manufacturer of medical respirators, is taking the necessary measures to prioritize the production of devices to assist patients with severe respiratory failure. But due to the acute shortage of equipment at the moment, alternative ventilation options, incl. non-invasive respiratory support.
The COVID-19 pandemic has led to a shortage of ventilators. In this regard, primary care for patients with coronavirus infection and symptoms of acute respiratory failure can be carried out using CPAP and BIPAP machines.
CPAP and bipap therapy can be used to provide primary care to patients with COVID-19 who require respiratory support. According to clinical protocols and reports received from clinicians in Italy and China, non-invasive ventilation (including BPAP and CPAP) for patients with COVID-19 is recommended in the following scenarios.
- To provide respiratory support to patients with respiratory failure who have not yet progressed to more severe hypoxemia.
- To facilitate extubation and recovery after invasive ventilation.
- To reduce hospital stays by allowing patients who still require respiratory support and rehabilitation to transition to home care.
NIV cannot replace invasive ventilation in the most severe forms of COVID-19. But this therapy is important when triaging patients in medical institutions. CPAP and BIPAP machines provide supplemental oxygen for less severe cases and reduce dependence on invasive ventilation. In addition, they are relevant for countries where hospital bed capacity turned out to be insufficient during the ongoing pandemic.
The following ResMed brand devices are suitable for home therapy: Lumis series BIPAP devices, as well as the AirCurve 10 CS PaceWave servo ventilator. They can be connected to additional oxygen (up to 15 l/min), as well as a module with a pulse oximetry sensor to monitor blood oxygen saturation.
Long-term use of non-invasive ventilation: benefit or harm
There is an opinion that the longer a patient is on a ventilator, the more difficult it is for him to refuse a respirator. This gives rise to the fear of “forgetting how” to breathe without a device and the fear of suffocation if the device turns off for some reason. But such risks occur only with invasive ventilation, when the device literally breathes instead of the patient. In turn, long-term use of non-invasive ventilation does not cause addiction, because the patient breathes on his own, and medical equipment only helps him with this.
According to research results, long-term non-invasive respiratory support (including at home) can optimize gas exchange, reduce the load on the respiratory system and reduce the risk of subsequent hospitalizations in patients with COPD. One of the advantages of long-term NIV is the ability to provide rest to the respiratory muscles, which are in a state of chronic fatigue.
Long-term use of non-invasive ventilation improves sleep quality and well-being while awake. When NIV is discontinued even for a week, patients with chronic respiratory failure begin to have morning migraines again, shortness of breath appears, and their night saturation also worsens.
NIV for chronic respiratory failure is most often performed at night. First, it increases the total time of respiratory support. Secondly, it helps eliminate nocturnal hypoventilation and episodes of desaturation, which most often occur in the REM phase of sleep.