SPIRIVA RESPIMAT solution for inhalation 2.5 mcg/dose 4 ml 60 doses
Tiotropium bromide is a long-acting m-anticholinergic blocker. The drug has the same affinity for the M 1 -M 5 subtypes of muscarinic receptors. The result of inhibition of M 3 receptors in the respiratory tract is relaxation of smooth muscles. The bronchodilator effect depends on the dose and lasts for at least 24 hours. The significant duration of action is probably due to the very slow dissociation of the drug from M 3 receptors; The half-dissociation period is significantly longer than that of ipratropium bromide. When administered by inhalation, tiotropium bromide, as an N-quaternary ammonium derivative, has a local selective effect (on the bronchi), while in therapeutic doses it does not cause systemic m-anticholinergic side effects. Dissociation from M 2 receptors occurs faster than from M 3 receptors, which indicates the predominance of selectivity for the M 3 receptor subtype over M 2 receptors. High affinity for receptors and slow dissociation of the drug from connection with receptors determine a pronounced and long-lasting bronchodilator effect in patients with chronic obstructive pulmonary disease (COPD). Bronchodilation that develops after inhalation of tiotropium bromide is primarily due to local (on the respiratory tract) rather than systemic effects. Clinical studies have shown that the use of Spiriva Respimat once a day leads to a significant improvement (compared to placebo) in lung function (forced expiratory volume in 1 second FEV1 and forced vital capacity FVC) within 30 minutes after the first dose. . Improvement in lung function persists for 24 hours at steady state. Pharmacodynamic equilibrium was achieved within one week. Spiriva Respimat significantly improved morning and evening peak expiratory volume flow (PEEF) measured by patients. Spiriva Respimat resulted in a reduction (compared with placebo) in rescue bronchodilator use. The bronchodilator effect of the drug persists for 48 weeks of use of the drug; There are no signs of addiction. Analysis of combined data from two randomized, placebo-controlled, crossover clinical trials showed that the bronchodilator effect of Spiriva Respimat (5 mcg) after a 4-week treatment period was quantitatively greater than the effect of Spiriva (18 mcg). In long-term (12-month) studies, Spiriva Respimat was found to significantly reduce shortness of breath; improves quality of life; reduces the psychosocial impact of COPD and increases activity. Spiriva Respimat significantly improved overall health status (total score) compared with placebo at the end of two 12-month studies, a difference that was maintained throughout the treatment period; Spiriva Respimat significantly reduced the number of exacerbations of COPD and increased the period until the first exacerbation compared to placebo. Spiriva Respimat has been shown to reduce the risk of exacerbation of COPD and significantly reduce the number of hospitalizations. In a retrospective analysis of individual clinical studies, a statistically insignificant increase, compared with placebo, in the number of deaths in patients with cardiac arrhythmias was observed. However, these data are not statistically confirmed and may be associated with heart disease. Pharmacokinetics Tiotropium bromide is a quaternary ammonium derivative, sparingly soluble in water. Tiotropium bromide is available as an inhalation solution, which is used with the Respimat inhaler. Approximately 40% of the inhalation dose is deposited in the lungs, the rest enters the gastrointestinal tract. Some pharmacokinetic data described below were obtained using doses higher than those recommended for treatment. Absorption After inhalation of the solution by young healthy volunteers, it was found that about 33% of the inhalation dose enters the systemic circulation. Eating does not affect the absorption of tiotropium bromide, due to the fact that it is poorly absorbed from the gastrointestinal tract. Absolute bioavailability when taken orally is 2-3%. Cmax in plasma is observed 5 minutes after inhalation. Distribution: The binding of the drug to plasma proteins is 72%; V d - 32 l/kg. At the dynamic equilibrium stage, the peak plasma concentration of tiotropium bromide in patients with COPD is 10.5-11.7 pg/ml 10 minutes after administration of the drug at a dose of 5 mcg using the Respimat inhaler. At the stage of dynamic equilibrium, the lowest plasma concentration was 1.49-1.68 pg/ml. Studies have shown that tiotropium bromide does not cross the BBB. Metabolism The degree of biotransformation is insignificant. This is confirmed by the fact that after intravenous administration of the drug to young healthy volunteers, 74% of the substance tiotropium bromide in unchanged form is found in the urine. Tiotropium bromide is an ester that splits into ethanol-N-methylscopine and dithienylglycolic acid; these compounds do not bind to muscarinic receptors. In vitro studies have shown that some of the drug (
Spiriva® Respimat®
Tiotropium bromide is a quaternary ammonium derivative, sparingly soluble in water. Tiotropium bromide is available as an inhalation solution, which is used with the RESPIMAT inhaler.
Approximately 40% of the inhalation dose is deposited in the lungs, the rest enters the gastrointestinal tract. Some pharmacokinetic data described below were obtained using doses higher than those recommended for treatment.
Suction
After inhalation of the solution by young healthy volunteers, it was found that about 33% of the inhalation dose enters the systemic circulation. Taking pitti does not affect the absorption of tiotropium bromide, due to this. that it is poorly absorbed from the gastrointestinal tract.
Absolute bioavailability when taken orally is 2 - 3%. The maximum concentration in plasma is observed 5-7 minutes after inhalation. At the dynamic equilibrium stage, the peak plasma concentration of tiotropium in patients with COPD is 10.5 pg/ml and decreases rapidly. This indicates a multicompartmental type of drug distribution. At the stage of dynamic equilibrium, the basal concentration of tiotropium in the blood plasma is 1.6 pg/ml. At the stage of dynamic equilibrium, the peak concentration of tiotropium in blood plasma in patients with bronchial asthma was 5.15 pg/ml and was achieved after 5 minutes. Distribution
The binding of the drug to plasma proteins is 72%; volume of distribution 32 l/kg. Studies have shown that tiotropium bromide does not penetrate
blood-brain barrier. Biotransformation
The degree of biotransformation is insignificant. This is confirmed by the fact that after intravenous administration of the drug to young healthy volunteers, 74% of the substance tiotropium bromide in unchanged form is found in the urine. Tiotropium bromide is an ester that is cleaved into ethanol-M-methylscopine. and dithienylglycolic acid; these compounds do not bind to muscarinic receptors.
in vitro studies
it has been shown that some part of the drug (<20% of the dose after intravenous administration) is metabolized by oxidation by cytochrome P450, followed by conjugation with glutathione and the formation of various metabolites. This mechanism can be inhibited by inhibitors of the CYP450 isoenzymes 2D6 and 3A4, quinidine, ketoconazole and gestodene. Thus, CYP450 2D6 and 3A4 are involved in metabolism. Tiotropium bromide, even at supratherapeutic concentrations, does not inhibit cytochrome P450 1A1, 1A2, 2B6, 2C9, 2C19, 2D6, 2E1 or 3A in human liver microsomes.
Removal
The terminal half-life of tiotropium bromide after inhalation is 27 to 45 hours in patients with COPD. In patients with asthma, the effective half-life after inhalation is 34 hours.
The total clearance after intravenous administration of the drug to young healthy volunteers was 880 ml/min. Tiotropium bromide after intravenous administration is mainly excreted unchanged by the kidneys (74%). After inhalation of the solution in patients with COPD, renal excretion is 18.6% (0.93 mcg), the remaining unabsorbed portion is excreted through the intestine. At the pharmacokinetic equilibrium stage in patients with asthma, 11.9% (0.595 mcg) of the dose is excreted unchanged in the urine 24 hours after taking the drug. The renal clearance of tiotropium bromide exceeds the clearance of creatinine, indicating its tubular secretion. After long-term inhalation administration of the drug once a day by patients with COPD, pharmacokinetic equilibrium is achieved on day 7; however, no further accumulation is observed.
Tiotropium bromide has linear pharmacokinetics within therapeutic limits after intravenous administration, dry powder inhalation and solution inhalation. Pharmacokinetics in elderly patients
In old age, there is a decrease in renal clearance of tiotropium
(347 ml/min in patients with COPD under the age of 65 years and 275 ml/min in patients with COPD and asthma over 65 years of age), It has been established that in patients with bronchial asthma, the effect of tiotropium bromide does not depend on the age of the patients.
Patients with impaired renal function
After inhaled once-daily administration of tiotropium during steady-state pharmacokinetics in patients with COPD and mild renal impairment (creatinine clearance 50-80 ml/min), there was a slight increase in AUC0-6.ss by 1.8-30% and Cmax ,Ss compared with patients with normal renal function (creatinine clearance >80 ml/min). In patients with COPD and moderate to severe renal impairment (creatinine clearance <50 mL/min), intravenous tiotropium bromide resulted in a twofold increase in total exposure (AUC0-44 increased by 82% and Cmax increased by 52%) compared with patients with COPD and normal renal function. A similar increase in plasma concentration was noted after inhalation of the dry powder.
In patients with bronchial asthma and mild renal impairment (creatinine clearance 50-80 ml/min), inhaled tiotropium bromide did not lead to a significant increase in exposure compared to patients with normal renal function.
Patients with liver dysfunction
It is assumed that liver failure does not have a significant effect on the pharmacokinetics of tiotropium bromide, since tiotropium bromide is primarily excreted by the kidneys and by non-enzymatic cleavage of the ester bond to form derivatives that do not have pharmacological activity.
Efficacy and safety of Spiriva Respimat for COPD and bronchial asthma
The new inhaler Spiriva Respimat is characterized by a simple inhalation technique, ensures good patient-inhaler coordination and is highly appreciated by patients. Long-term maintenance therapy with Spiriva Respimat in patients with chronic obstructive pulmonary disease significantly improves lung function, reduces shortness of breath, improves quality of life and reduces the risk of exacerbations, including those leading to hospitalization. In patients with poorly controlled bronchial asthma, despite therapy with inhaled glucocorticosteroids and long-acting beta-2 agonists, the addition of Spiriva Respimat to therapy can significantly reduce the severity of bronchial obstruction and reduce the risk of developing severe exacerbations of asthma.
Rice. 1. Respimat: appearance and diagram of the device
Rice. 2. Diagram of the uniblock device in the Respimat inhaler
Rice. 3. Duration of existence of an aerosol cloud when using Respimat and MDI [27]
Rice. 4. Deposition of inhaled drugs when using Respimat and DPI [28, 30]
Rice. 5. Comparison of different doses of tiotropium using Respimat and HandiHaler [32]
Rice. 6. Changes in FEV1 after inhalation of tiotropium in the form of Spiriva Respimat (5 μg) and Spiriva HandiHaler (18 μg) [33]
Table 1. Comparison of tiotropium Respimat and placebo: primary endpoints [39]
Rice. 7. Physical activity of patients with COPD while taking Spiriva Respimat [41]
Table 2. Most common adverse events with Spiriva Respimat [40]
Table 3. Adverse events during therapy with Spiriva Respimat [40]
Rice. 8. Mean plasma concentrations of tiotropium when administered via HandiHaler (18 mcg) or Respimat (1.25, 2.5 or 5 mcg) over 4 weeks in patients with COPD [50]
Rice. 9. All-cause mortality in patients with COPD during tiotropium therapy [51]
Table 4. All-cause mortality during tiotropium therapy [51]
Rice. 10. Time to development of the first exacerbation when treating patients with COPD with tiotropium [51]
Rice. 11. Change in FEV1 with the addition of tiotropium to ICS/LABA therapy (A – study 1; B – study 2) [53]
Rice. 12. Reduction in the number of severe asthma exacerbations when adding ICS/LABA tiotropium to therapy [53]
Rice. 13. Effect of training on pulmonary deposition when using Respimat and MDI [56]
Rice. 14. Patient preference when using Respimat and other inhalers [59, 60]
The value of tiotropium bromide for the treatment of COPD
Chronic obstructive pulmonary disease (COPD) is a disease characterized by airflow limitation with the development of incompletely reversible bronchial obstruction. Airflow limitation is progressive and is associated with an increased pathological inflammatory response of the airways to noxious particles or gases [1, 2]. According to a number of recent studies, the global prevalence of COPD in patients over 40 years of age is 10.1% (11.8% in men and 8.5% in women) [3]. According to the World Health Organization, COPD ranks 4th in the world among the leading causes of death: about 2.75 million people die from COPD every year, accounting for 4.8% of the mortality rate [1]. The economic costs for a patient with COPD are 3 times higher than for a patient with bronchial asthma. The greatest economic damage comes from the treatment of exacerbations of COPD [1].
Drug therapy for COPD is used to prevent and control symptoms of the disease, improve the quality of life of patients, reduce the frequency and severity of exacerbations and reduce mortality [1, 2]. Long-acting bronchodilators are recognized as the first-line treatment of most patients with COPD [1], among which the most studied and most frequently used is the active anticholinergic drug (ACD) tiotropium bromide [4, 5].
The advantages of tiotropium bromide include its selectivity towards M1 and M3 receptors and long-lasting action. The drug provides bronchodilation and protection against cholinergic bronchoconstrictor stimuli for 24 hours, which allows its administration once a day [4–6]. These properties of the drug significantly simplify the dosage regimen and improve patient adherence to therapy.
The increase in functional pulmonary parameters in patients with COPD during therapy with tiotropium bromide in all studies exceeded that in patients receiving comparator drugs (ipratropium, salmeterol, etc.), and this improvement was maintained throughout the entire study period without the development of tachyphylaxis [7–10]. Tiotropium bromide was the first drug whose positive effect on pulmonary hyperinflation was confirmed in randomized controlled trials (RCTs) [11, 12]. The positive dynamics of pulmonary functional parameters during therapy with tiotropium bromide was accompanied by an improvement in the clinical picture, exercise tolerance, quality of life of patients, and a decrease in the frequency of taking short-acting bronchodilators. Patients taking tiotropium bromide had fewer exacerbations of COPD, the time to the first exacerbation significantly increased, and the number of hospitalizations decreased [6].
In the global four-year study UPLIFT (Understanding Potential Long-term impacts on Function with Tiotropium), for the first time evidence was obtained of a reduction in mortality in patients with COPD during long-term use of tiotropium bromide - a significant reduction in the relative risk of death was achieved by 13% (p 1), that is, it slows down progression of COPD [14–16]. Taking tiotropium bromide significantly reduced the number of episodes of respiratory failure (RR 0.69; 95% CI 0.52–0.92).
The vast majority of studies of tiotropium bromide have been performed with the HandiHaler metered-dose powder inhaler (DPI) delivery device (daily dose: 1 inhalation of 18 mcg). Quite recently, a new drug was registered in Russia - Spiriva Respimat, the cardinal difference of which from Spiriva HandiHaler is the drug delivery device - the Respimat inhaler. As is known, the key to successful inhalation therapy is not only the properties of the drug, but also the choice of the optimal delivery system. An ideal delivery device should ensure good drug deposition in the lungs, be reliable, fairly easy to use, and available for use at any age and in severe stages of the disease. From this point of view, the new Respimat inhaler truly represents a step forward in the field of inhalation therapy [17].
Main characteristics of the Respimat inhaler
The Respimat soft mist inhaler is based on the forced passage of a medicinal solution through a series of channels that converge to two outlets - nozzles (Fig. 1 and 2), creating two liquid jets, upon collision of which a medicinal aerosol is formed [18, 19].
To activate the device, the base is rotated 180 degrees until it clicks, which compresses the spring and advances the capillary tube with the one-way valve of the solution cartridge. In this way, the liquid is pumped into the dosing chamber (Fig. 1). When the button is pressed, the spring is released and pushes the capillary tube towards the so-called uniblock (Fig. 1 and 2), closing the one-way valve and turning the capillary tube towards the piston, thereby beginning to move the solution through the uniblock. Next, the drug solution is forced through microchannels that converge to two mirror-like outlets. When exiting them, liquid jets collide at a certain angle, resulting in the formation of a medicinal aerosol.
The Respimat inhaler has a compact design and is equipped with a digital dose counter (Fig. 1). The meter needle approaches the red zone when the drug remains in the inhaler for approximately a week [18]. After activating a specified number of doses (Spiriva Respimat has 60 doses), the mechanism is blocked and further use of the inhaler becomes impossible.
The optimal aerodynamic diameter of aerosol particles is in the range from 1 to 5 microns. Particles with a diameter of 5 microns settle in the upper DP (oropharynx). Approximately 75% of aerosol particles produced by Respimat have a mean aerodynamic diameter ≤ 5.8 μm and ≤ 5% have a mean aerodynamic diameter ≤ 1 μm [19, 20].
The efficiency of delivery of medicinal aerosols to the lower AP is significantly influenced by the deposition of the drug in the inhalation device and on the posterior wall of the oropharynx, which occurs due to the ballistic effects of the aerosol and turbulent dispersion [21–25]. The coordination between device activation and aerosol inhalation depends on the speed of the aerosol cloud and its lifetime. The delivery of an aerosol drug to the lower DP can be improved by creating a longer-lasting aerosol cloud [26]. D. Hochrainer et al. measured the velocity of the aerosol stream at a distance of 10 cm from the outlet of 3 different inhalers - a metered-dose aerosol inhaler (MDI) with freon filler, a MDI with hydrofluoroalkane, and Respimat. It turned out that the speed of the aerosol jet was 5.6, 2.4 and 0.8 m/s, respectively [27]. In the same study, using video recording, it was shown that the duration of existence of the aerosol cloud when using these inhalers was 0.15, 0.21 and 1.45 s, respectively (Fig. 3) [27]. Thus, the Respimat inhaler creates a slow, high-speed aerosol cloud that lasts 7–10 times longer than the cloud created by a MDI. The low speed of aerosol particles emanating from Respimat improves the capture of particles during the patient's inhalation maneuver, their increased delivery to the lower airway, as well as a decrease in oropharyngeal deposition.
Scintigraphic studies have demonstrated higher pulmonary and lower oropharyngeal drug deposition with Respimat compared with metered-dose inhalers (DPIs) and MDIs with and without a spacer [28–32]. In a study with healthy volunteers, SP Newman et al. showed that the pulmonary deposition of flunisolide or fenoterol when using Respimat is 39.2–44.6%, while the oropharyngeal deposition is only 26.2–39.9% (Fig. 4) [29, 30]. In the same studies, the pulmonary deposition of drugs when inhaled using a MDI without a spacer was 11.0–15.3%, and when using a MDI with a spacer, it was 9.9–28% (Fig. 4) [29, 30]. Another study compared the deposition of budesonide inhaled with Respimat and Turbuhaler: pulmonary deposition of the drug was 51.6 and 28.5%, respectively, and oropharyngeal deposition was 19.3 and 49.3%, respectively [31].
Doses of tiotropium bromide when using Spiriva Respimat
Since the Respimat inhalation device is the most effective compared to all known portable delivery devices (MDI and DPI), it would be logical to assume that when using Respimat, a reduction in traditional drug doses used with other inhalers would be required. Indeed, today the recommended dose of tiotropium bromide when using Respimat is 5 mcg (when using Spiriva HandiHaler - 18 mcg). The new dose was determined through several dose-response studies. A multicenter RCT involving 202 patients with COPD in parallel groups compared 5 doses of tiotropium bromide inhaled via Respimat (1.25, 2.5, 5, 10 and 20 mcg) to 1 conventional dose of tiotropium bromide inhaled via HandiHaler (18 mcg), and placebo [32]. The primary endpoint of the study was pre-bronchodilator FEV1 on day 21 of therapy. The effectiveness of treatment with doses of tiotropium bromide of 5 and 20 mcg via Respimat and 18 mcg via HandiHaler was significantly different from that in the placebo control group. At the same time, in terms of the effect on the parameters of the external respiration function, the doses of tiotropium inhaled through Respimat, 5 mcg, and tiotropium inhaled through HandiHaler, 18 mcg, were maximally consistent with each other. In addition, by another index, urinary excretion of tiotropium bromide 0–2 hours before inhalation on day 21, these tiotropium doses administered using different inhalers were virtually equivalent (Fig. 5).
A randomized, double-blind, crossover study in which 134 patients with COPD (mean age 70 years, mean FEV1 43%) received either Spiriva Respimat 5 mcg or Spiriva HandiHaler 18 mcg for 21 days showed complete equivalence. doses of tiotropium bromide both in terms of the percentage of improvement in pulmonary function parameters (Fig. 6) and in terms of the effect on plasma concentrations of tiotropium in the first 3 hours after inhalation [33]. Therefore, when prescribing Spiriva Respimat, it is recommended to use a dose of 5 mcg per day (that is, 2 consecutive inhalations of 2.5 mcg per day).
Clinical efficacy of Spiriva Respimat
To date, the results of five RCTs have been published that examined the effectiveness of Spiriva Respimat for at least 12 weeks [34–38]. Collectively, these studies included 6522 patients with COPD. Of these, 3686 received therapy with Spiriva Respimat (2839 patients at a dose of 5 mcg/day and 847 patients at a dose of 10 mcg/day) and 2836 received placebo. Two studies lasted 12 weeks [34, 35], three lasted 1 year [36–38].
The data obtained once again confirmed the high efficiency of tiotropium bromide [5].
In all studies, Spiriva Respimat at doses of 5 and 10 mcg was significantly superior to placebo and comparable to ipratropium in the first hours after inhalation in terms of the effect on pulmonary functional parameters. Both doses of tiotropium bromide in long-term studies resulted in significant and clinically significant improvements in health-related quality of life and reductions in dyspnea as measured by the Transition Dyspnee Index (TDI) [39] (Table 1).
In addition, therapy with Spiriva Respimat led to a significant reduction in the number of all exacerbations of COPD by 31%, and severe exacerbations leading to hospitalization of patients by 27% [40]. Thus, Spiriva Respimat significantly improves lung function, reduces shortness of breath, improves quality of life and reduces the risk of exacerbations, including those leading to hospitalization.
In an open-label observational study involving 1230 patients with COPD, treatment with Spiriva Respimat 5 mcg for 6 weeks was shown to significantly improve patients' physical activity. There was a significant increase in scores on the “physical functioning” scale of the SF-36 questionnaire (Short Form – 36) by 13.4 points (p
Safety of Spiriva Respimat
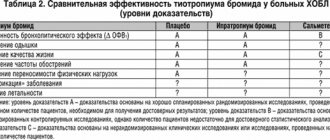
Like other representatives of the ACP group, tiotropium is traditionally considered as one of the safest drugs for the treatment of COPD [5]. The favorable profile of Spiriva HandiHaler has been confirmed by numerous studies. The new drug Spiriva Respimat could theoretically have even greater safety because it contains a lower dose of tiotropium and is characterized by less deposition in the oropharynx. This may lead to a decrease in its systemic bioavailability. When analyzing the most common adverse events recorded in studies of Spiriva Respimat, attention is drawn to the more frequent development of such an adverse event as dry mouth - an effect specific to all ACPs (Table 2). However, this adverse event occurs approximately 2 times less often when using Spiriva Respimat than Spiriva HandiHaler [32, 42], which can be explained by less drug deposition in the oropharynx when inhaled through Respimat.
In a study by U. Feifel et al. When using very high doses of Spiriva Respimat (up to 32 mcg/day), only mild anticholinergic side effects (dry mucous membranes) were noted [43]. In the same study, volunteers were given tiotropium solution instilled into their eyes to study ocular side effects. At the same time, there were no changes in pupil diameter, pupillary reflexes, intraocular pressure or accommodation, that is, if the drug from the Respimat inhaler accidentally gets into the eyes, the development of any adverse events is unlikely.
R. Hodder et al. conducted a special analysis of 12-month studies of Spiriva Respimat involving a total of 1990 patients with COPD to identify paradoxical bronchoconstriction with the use of this drug [44]. In the analyzed studies, there was no indication of the development of paradoxical bronchospasm; 21 (1.1%) patients noted the need to use fast-acting bronchodilators or the development of respiratory discomfort, and 6 (0.3%) patients noted discomfort that required taking a fast-acting bronchodilator. Moreover, these undesirable effects were also observed in the placebo group. Therefore, paradoxical bronchoconstriction is unlikely with Spiriva Respimat therapy.
Over the past 3 years, there has been intense debate regarding the cardiovascular safety of Spiriva Respimat [45–49]. After a cumulative analysis of 2 year-long studies of similar design, E. Bateman et al. noted that the number of deaths from any cause among patients taking Spiriva Respimat was slightly higher - 2.4 and 2.7% (with 5 and 10 mcg tiotropium, respectively) - compared with patients in the placebo group (1.6% ) [39]. However, these differences were not statistically significant. Is there a direct relationship between the increased mortality, or is it simply coincidence (especially since the mortality in these studies is no higher or even lower than in other studies of the effectiveness of drugs in patients with COPD)? Interestingly, in these studies, the cause of death was not only cardiovascular diseases, but also malignant neoplasms (Table 3). Considering the duration of the studies (1 year), we can safely say that there is no biological probability of a relationship between the use of Spiriva Respimat and the development of tumors.
The results of a meta-analysis by S. Singh et al., based on data from five RCTs that studied the effectiveness of Spiriva Respimat in 6522 patients with COPD, caused quite a wide resonance [48]. The authors concluded that the use of Spiriva Respimat leads to a significant increase in the risk of mortality (RR 1.52; 95% CI 1.06–2.16; p = 0.02). At the same time, both the tiotropium dose was 10 mcg (RR 2.15; 95% CI 1.03–4.51; p = 0.04) and the tiotropium dose was 5 mcg (RR 1.46; 95% CI 1.01–2 .10; p = 0.04) were associated with an increased risk of death. The findings included a figure of 124 patients (95% CI 52–5682) for the number needed to treat (NNT) per year to achieve 1 death. Explaining the possible association of Spiriva Respimat therapy with increased mortality, the researchers suggested that the Respimat inhaler, by providing better deposition of tiotropium in the lungs, leads to its increased concentration in the systemic circulation (i.e., increased systemic bioavailability), which in turn increases the risk of arrhythmic events. However, from a pharmacokinetic point of view, this explanation is unlikely. A comparison of plasma concentrations of tiotropium after inhalation through Respimat and after inhalation through HandiHaler in doses of 5 and 18 μg, respectively, demonstrated that their peak concentrations and areas under the concentration curves (AUC) are almost identical [20, 33].
The study, presented at the 2013 European Respiratory Society (ERS) Congress, compared the pharmacokinetic properties of tiotropium at doses of 1.25, 2.5 and 5 mcg, inhaled using the Respimat device, and tiotropium inhaled dose of 18 mcg, inhaled through HandiHaler [50]. This multicenter, crossover, placebo-controlled, double-blind study included 154 patients with COPD. Each of the five stages of therapy took 4 weeks, the primary endpoint of the study was the peak concentration of the drug (Cmax,ss) and the area of the concentration curve within 6 hours after inhalation of the drug (AUC0-6h,ss). As this study showed, tiotropium was rapidly absorbed from the mucous membranes. However, there were no differences between the devices and the median achievement of the maximum concentration tmax,ss was 5–7 minutes after inhalation (Fig. 8). The pharmacokinetic profile of Spiriva Respimat was proportional to the drug doses used (1.25, 2.5 and 5 mcg). The bioavailability of the 5 mcg dose of Spiriva Respimat was slightly less than that of the 18 mcg dose of Spiriva HandiHaler. The mean ratio between these doses inhaled via Respimat and HandiHaler (P5/XX18) was 81% (90% CI 73–89%) for Cmax,ss and 76% (90% CI 70–82%) for AUC0-6h. ss, indicating lower systemic exposure to tiotropium when using Respimat.
BJ Lipworth and PM Short, commenting on the results of a meta-analysis conducted by S. Singh et al., noted that the data obtained can hardly be trusted, since they are based on studies in which deaths were not endpoints, and the 95% CI is simply huge range – 52–5682 patients [49]. Taking into account the data demonstrating a decrease in cardiovascular events during therapy with Spiriva HandiHaler, on the one hand, and their increase during therapy with Spiriva Respimat, on the other, the authors of the commentary qualified the very possibility of developing adverse effects from the cardiovascular system during the use of Spiriva Respimat as lack of biological plausibility. Moreover, the increase in cardiovascular events as a consequence of taking Spiriva Respimat cannot be explained in terms of increased systemic bioavailability of the drug.
More reliable data on the safety of Spiriva Respimat are presented in the recently published largest study in the field of COPD, the randomized, double-blind TIOSPIR (The Tiotropium Safety and Performance in Respimat Trial) [51]. The TIOSPIR study included 17,135 patients with COPD (mean age 65 years, mean FEV1 48%) who received Spiriva Respimat 2.5 or 5 mcg daily or Spiriva HandiHaler 18 mcg daily for an average of 2.3 years. The primary endpoints of the study were the risk of death and the risk of developing a first exacerbation of COPD; the cardiovascular safety of the drugs was also studied, including safety assessment in patients with stable heart disease (among which 15.2% of patients had ischemic heart disease, 6% - post-infarction cardiosclerosis, 10.6% – arrhythmias).
The study showed that long-term therapy with Spiriva Respimat did not differ from therapy with Spiriva HandiHaler in terms of the risk of death (for tiotropium at a dose of 5 μg RR 0.96; 95% CI 0.84-1.09; for tiotropium at a dose 2.5 μg RR 1.00; 95% CI 0.87–1.14) (Fig. 9, Table 4) and by the risk of developing the 1st exacerbation (for tiotropium at a dose of 5 mcg RR 0.98; 95% CI 0.93 –1.03) (Fig. 10). The number of deaths and major cardiovascular events was similar in all three tiotropium treatment groups.
Thus, the results of the global TIOSPIR study practically complete the long-term discussion about the possible cardiovascular risks of COPD therapy with Spiriva Respimat, clearly demonstrating that the new drug has a good safety profile.
Spiriva Respimat in stepwise therapy of uncontrolled bronchial asthma in adults
In many patients with bronchial asthma (BA), low and medium doses of inhaled glucocorticosteroids (ICS) do not allow them to achieve adequate control of the disease. Therefore, additional prescription of long-acting beta-2 agonists (LABAs), leukotriene receptor antagonists or an increase in the dose of ICS is required. The effectiveness of short-acting antihypertensive drugs (ipratropium) for the basic treatment of asthma has not been proven, and the effectiveness of tiotropium has been studied in only a few studies. SP Peters et al. in the double-blind crossover randomized trial TALC (Tiotropium bromide as an Alternative to increased inhaled glucocorticoid in patients inadequately controlled on a Lower dose of inhaled Corticosteroid) compared additional tiotropium therapy, doubling the dose of ICS and additional LABA therapy in patients with asthma inadequately controlled by monotherapy ICS [52]. This work demonstrated that in patients with inadequate asthma control on ICS monotherapy, adding tiotropium is more effective than doubling the ICS dose. Improvement in lung function during treatment with tiotropium was accompanied by a decrease in symptoms and an increase in the number of days of controlled asthma.
New evidence has recently emerged regarding the role of tiotropium therapy in patients with poorly controlled asthma. Two randomized placebo-controlled studies of similar design examined the effectiveness of additional tiotropium therapy (at a dose of 5 μg per day through the Respimat inhalation device) in asthma patients already receiving ICS and LABA [53]. Pulmonary functional parameters and the number of exacerbations were chosen as the main effectiveness criteria. The study lasted 48 weeks. Before inclusion in the study, all patients had symptoms of the disease, FEV1 was less than 80% of normal values, and patients had at least one exacerbation of asthma in the previous year. A total of 912 patients with asthma participated in the studies (mean age 53 years, mean FEV1 62%).
After 24 weeks from the start of therapy in both studies, the change in peak FEV1 from baseline was more pronounced in patients receiving additional tiotropium therapy, the difference in FEV1 between groups was 86 ± 34 ml (p = 0.01) and 154 ± 32 ml (p 1, measured before inhalation of the bronchodilator (trough FEV1), in the tiotropium treatment groups was 88 ± 31 ml (p = 0.01) and 111 ± 30 ml (p 1 was relatively small (
In addition, adjunctive tiotropium therapy resulted in a 21% reduction in the total number of severe asthma exacerbations (RR 0.79; p = 0.03) and an increase in time to first exacerbation (282 vs. 226 days) (Fig. 12). The reduction in the risk of severe exacerbations was significant in a post hoc analysis, with the number needed to treat (NNT) to prevent one exacerbation over 48 weeks being 15.
In the studies conducted, adverse events and serious adverse events occurred equally frequently in both comparison groups. Dry mouth, a common side effect across the ACP class, was reported in less than 2% of patients and was more common with tiotropium (8 vs. 3 patients).
The effects achieved by adding tiotropium to standard therapy in patients with asthma should be considered through the lens of achieving additional benefits against the background of the most accepted therapy for asthma. Thus, the addition of leukotriene and xanthine receptor antagonists to ICS/LABA therapy is usually not accompanied by any significant positive effects, systemic GC therapy is associated with severe side effects, and omalizumab therapy is only suitable for a very limited cohort of patients (IgE-dependent asthma).
Patient's opinion about the Respimat inhaler
From a physician's point of view, the choice of an inhalation device for therapy is determined by many factors, such as the drug substance, proven clinical effectiveness, ease of use of the inhaler, and economic aspects of therapy. In addition, among these factors, the patient's attitude towards the device plays an important role. The advantage of the Respimat inhalation device is its simple inhalation technique [54]. Acceptable inhalation technique using Respimat is achieved in 96–98% of patients after just the first five inhalations through the device [55]. Another advantage of Respimat is good coordination between the patient and the inhaler, which ensures high delivery of the drug to the respiratory tract even in an untrained patient. In a study by P. Brand et al. pulmonary deposition of the drug during inhalation through Respimat in patients with COPD was 37% before training in the inhalation technique and 53% after training (Fig. 13) [56]. In contrast, in the same study, the best pulmonary deposition rates for inhaled CFC-free MDI after exercise were 21% [56].
While many studies have examined patient evaluation of various delivery devices, results favoring one or the other inhaler may be found, but more often these studies have used randomized questionnaires that do not address the fundamentals of psychometric testing [57]. Therefore, particular attention has been drawn to studies that have used more advanced instruments, such as the Patient Satisfaction and Preference Questionnaire (PASAPQ), a practical, validated, reliable and sensitive tool for testing patient attitudes towards an inhalation device [58]. In a study by W. Schurmann et al., which included 224 patients with COPD and asthma, patients' preferences for using Respimat and MDI inhalers were compared using PASAPQ [55]. The study demonstrated that the vast majority of patients (81%) preferred the Respimat inhaler and would like to use it in the future [55]. The mean score for 13 of the 15 questions on the PASAPQ was significantly higher for the Respimat score compared to the DAI score (p
In two other studies of similar design, including 152 and 150 patients with COPD and asthma, using the PASAPQ questionnaire, patients' preferences were compared when using Respimat and DPI (Multidisk and Turbuhaler) [59, 60]. Overall preference was given to Respimat by 74 and 64% of patients, Turbuhaler by 17%, and Multidisk by 34%. In both studies, the total PASAPQ score for Respimat was significantly higher than for DPI (p
Finally, in a small real-world study assessing the effects of switching COPD patients from Spiriva HandiHaler to Spiriva Respimat, 72% of patients were in favor of the new inhaler [42].
Conclusion
Based on the data presented in the review, the following conclusions can be drawn.
The new Respimat inhaler is characterized by a simple inhalation technique, provides good patient-inhaler coordination and is highly appreciated by patients.
Long-term maintenance therapy with Spiriva Respimat in patients with COPD significantly improves lung function, reduces shortness of breath, improves quality of life and reduces the risk of exacerbations, including those leading to hospitalization.
In patients with COPD, data on adverse events associated with Spiriva Respimat therapy are consistent with the known safety profile of Spiriva HandiHaler.
Spiriva Respimat has a good safety profile, no different from Spiriva HandiHaler. This is confirmed by the results of the global study TIOSPIR.
In patients with poorly controlled asthma, despite therapy with ICS and LABA, the addition of Spiriva Respimat to therapy can significantly reduce the severity of bronchial obstruction and reduce the risk of developing severe exacerbations of asthma.
Spiriva powder for ing caps 18 µg N 30+inhaler
Active substance
tiotropium bromide
ATX code
R03BB04 (Tiotropium bromide)
Release form, packaging and composition of the drug
Capsules with powder for inhalation
hard gelatin, size No. 3, light greenish-blue color, opaque; with the symbol printed in black ink; the contents of the capsules are white powder.
| 1 caps. | |
| tiotropium bromide monohydrate | 22.5 mcg, |
| which corresponds to the content of tiotropium | 18 mcg |
[PRING] lactose monohydrate, 200 M - 5.2025 mg, micronized lactose monohydrate - 0.2750 mg.
Capsule composition (mg/capsule):
macrogol - 2.4000 mg, indigo carmine (E132) - 0.0120 mg, titanium dioxide (E171) - 1.0240 mg, yellow iron oxide (E172) - 0.0120 mg, gelatin - 44.5160 mg.
10 pieces. - blisters (1) complete with or without the HandiHaler® inhaler - cardboard packs. 10 pieces. - blisters (3) complete with or without the HandiHaler® inhaler - cardboard packs. 10 pieces. - blisters (6) complete with or without the HandiHaler® inhaler - cardboard packs.
Clinical and pharmacological group
Bronchodilator - m-cholinergic receptor blocker
Pharmacotherapeutic group
M-anticholinergic
pharmachologic effect
Tiotropium bromide is a quaternary ammonium compound, sparingly soluble in water.
Tiotropium bromide has linear pharmacokinetics within therapeutic limits after intravenous administration and dry powder inhalation.
Suction
When administered by inhalation, the absolute bioavailability of tiotropium bromide is 19.5%, which indicates the high bioavailability of the drug fraction reaching the lungs. Cmax in blood plasma is achieved 5-7 minutes after inhalation. Tiotropium bromide is poorly absorbed from the gastrointestinal tract. For the same reason, food intake does not affect the absorption of tiotropium. When taking tiotropium bromide orally in solution form, the absolute bioavailability was 2-3%.
Distribution
Plasma protein binding - 72%. Vd - 32 l/kg.
At steady state, Cmax in blood plasma in patients with COPD is 12.9 pg/ml and decreases rapidly. This indicates a multicompartmental type of drug distribution. At steady state, Cmin of tiotropium in blood plasma is 1.71 pg/ml.
Does not penetrate the BBB.
Metabolism
The degree of biotransformation is insignificant. This is confirmed by the fact that after intravenous administration of the drug to young healthy volunteers, 74% of the unchanged substance is found in the urine.
Tiotropium bromide is broken down nonenzymatically to alcohol-N-methylscopine and dithienylglycolic acid, which do not bind to muscarinic receptors.
Studies have shown that the drug (<20% of the dose after intravenous administration) is metabolized with the participation of cytochrome P450 isoenzymes, through oxidation and subsequent conjugation with glutathione to form various metabolites. Metabolic disturbances may occur when using inhibitors of CYP2D6 and CYP3A4 (quinidine, ketoconazole and gestodene). Thus, the isoenzymes CYP2D6 and CYP3A4 are included in the metabolism of the drug.
Removal
T1/2 of tiotropium after inhalation varies from 27 to 45 hours. The total clearance when administered intravenously to young healthy volunteers is 880 ml/min. Tiotropium after intravenous administration is mainly excreted unchanged by the kidneys (74%). After inhalation of the dry powder at steady state, renal excretion is 7% per day of the dose, the remaining unabsorbed portion is excreted through the intestines. The renal clearance of tiotropium exceeds the clearance of creatinine, indicating tubular secretion of the drug. After long-term administration of the drug once a day by patients with COPD, pharmacokinetic equilibrium is achieved on day 7, with no further accumulation observed.
Pharmacokinetics in special groups of patients
In elderly patients, a decrease in the renal clearance of tiotropium is observed (365 ml/min in patients with COPD under 65 years of age, to 271 ml/min in patients with COPD over 65 years of age). These changes did not lead to a corresponding increase in AUC0-6 or Cmax values.
In patients with COPD and mild renal impairment (creatinine clearance 50-80 ml/min), inhaled tiotropium once a day at steady state resulted in an increase in AUC0-6 by 1.8-30%. The Cmax value remained the same as in patients with normal renal function (creatinine clearance >80 ml/min). In patients with COPD and moderate or severe renal impairment (creatinine clearance <50 ml/min), intravenous tiotropium resulted in a twofold increase in plasma drug concentrations (AUC0-4h increased by 82% and Cmax increased by 52%). compared with patients with COPD and normal renal function. A similar increase in plasma tiotropium concentration was observed after inhalation of dry powder.
It is expected that hepatic impairment will not have a significant effect on the pharmacokinetics of tiotropium bromide because the drug is mainly excreted in the urine and the formation of pharmacologically active metabolites is not associated with the participation of enzymes.
Indications for use
- as maintenance therapy in patients with COPD, including chronic bronchitis and emphysema (maintenance therapy for persistent shortness of breath and to prevent exacerbations).
Dosage
Prescribed 1 capsule/day at the same time in the form of inhalations using the HandiHaler® inhaler.
The drug should not be swallowed. Spiriva should not be used more than once a day. Spiriva capsules should only be used with the HandiHaler® inhaler.
Elderly patients
The drug should be taken in recommended doses.
For impaired renal function
patients can use Spiriva® in recommended doses.
However, careful monitoring is required in patients with moderate or severe renal impairment
receiving Spiriva (as with other drugs excreted primarily by the kidneys).
Patients with liver failure
can take the drug in recommended doses.
How to use the HandiHaler® inhaler
The HandiHaler® inhaler is designed specifically for the use of Spiriva and is not intended for use with other medications. The patient can use their HandiHaler® for one year.
The inhaler includes: dust cap, mouthpiece, base, piercing button, central chamber.
Using the HandiHaler® inhaler:
1. Open the dust cap by pressing the piercing button fully and then releasing it.
2. Open the dust cap completely by lifting it up; then open the mouthpiece by lifting it up.
3. Immediately before use, remove the Spiriva capsule from the blister and place it in the central chamber (it does not matter which side the capsule is placed in the chamber).
4. Close the mouthpiece tightly until it clicks, leaving the dust cap open.
5. Holding the HandiHaler® with the mouthpiece facing up, press the piercing button all the way once and then release; This creates an opening through which the drug is released from the capsule during inhalation.
6. Exhale completely; never exhale into the mouthpiece.
7. Place HandiHaler® in your mouth and press your lips tightly around the mouthpiece; keeping your head straight, you should inhale slowly and deeply, but at the same time with enough force to hear or feel the vibration of the capsule; inhale until your lungs are completely filled; then hold your breath as long as possible and remove the HandiHaler® from your mouth; continue to breathe calmly; repeat procedures 6 and 7 to completely empty the capsule.
8. Next, you should open the mouthpiece again, remove and discard the used capsule. Close the mouthpiece and dust cap.
Cleaning the HandiHaler® inhaler
HandiHaler® should be cleaned once a month. To do this, open the mouthpiece and dust cap, then open the base of the device by lifting the piercing button. Rinse the inhaler thoroughly in warm water until the powder is completely removed. HandiHaler® should be wiped with a paper towel and with the mouthpiece, base and dust cap open, left to air dry for 24 hours. Once cleaned in this manner, the device is ready for subsequent use. If necessary, the outer surface of the mouthpiece can be cleaned using a damp, but not wet, cloth.
Opening the blister
Separate the blister strip along the perforated line. Open the blister strip immediately before use so that one capsule is completely visible. The capsule contains a small amount of powder, so it is not completely filled.
If the capsule is accidentally opened and exposed to air, it should not be used. Neither in the device nor in the blister, capsules should be exposed to high temperatures or exposure to sunlight.
Contraindications
- I trimester of pregnancy;
- children and adolescents up to 18 years of age;
- hypersensitivity to atropine or its derivatives (including ipratropium and oxitropium);
- hypersensitivity to the components of the drug.
Carefully
The drug should be used for angle-closure glaucoma, prostatic hyperplasia, and bladder neck obstruction.
Overdose
Symptoms:
When using high doses, manifestations of anticholinergic effects are possible - dry mouth, accommodation disturbances, increased heart rate.
After inhalation of a single dose of up to 282 mcg in healthy volunteers, no systemic anticholinergic effects were detected. After repeated administration of a single daily dose of 141 mcg, bilateral conjunctivitis in combination with dry mouth was observed in healthy volunteers, which disappeared with continued treatment. In a study examining the effects of multiple-dose tiotropium in COPD patients receiving a maximum of 36 mcg of the drug for more than 4 weeks, dry mouth was the only adverse effect.
Acute intoxication associated with accidental ingestion of capsules is unlikely due to the low bioavailability of the drug.
Side effects
From the side of metabolism:
dehydration*.
From the digestive system:
often (≥1% and <10%) – dry mouth, usually mild; uncommon (≥0.1% and <1%) – stomatitis, constipation, gastroesophageal reflux; rarely (≥0.01% and <0.1%) – oropharyngeal candidiasis, gingivitis, glossitis; intestinal obstruction, including paralytic ileus, dysphagia.
From the respiratory system:
infrequently (≥0.1% and <1%) - dysphonia, cough, pharyngitis; rarely (≥0.01% and <0.1%) – paradoxical bronchospasm, laryngitis, sinusitis, nosebleeds.
From the cardiovascular system:
uncommon (≥0.1% and <1%) - atrial fibrillation; rarely (≥0.01% and <0.1%) – tachycardia (including supraventricular tachycardia), palpitations.
From the urinary system:
uncommon (≥0.1% and <1%) - difficulty urinating and urinary retention (in men with predisposing factors), dysuria; rarely (≥0.01% and <0.1%) - urinary tract infections.
Allergic reactions:
uncommon (≥0.1% and <1%) - rash; rarely (≥0.01% and <0.1%) - urticaria, itching, hypersensitivity reactions, including immediate reactions, angioedema*.
From the skin:
skin infections and skin ulcers, dry skin*.
From the musculoskeletal system:
swelling of the joints*.
From the nervous system:
uncommon (≥0.1% and <1%) - dizziness; rarely - (≥0.01% and <0.1%) - insomnia.
From the side of the organ of vision:
uncommon (≥0.1% and <1%) - blurred vision; rarely - (≥0.01% and <0.1%) - increased intraocular pressure, glaucoma.
* these adverse reactions were not identified in the combined database of clinical studies; There have been only isolated reports of these adverse reactions with widespread use of the drug, but the connection with the m-anticholinergic effect of the drug Spiriva® has not been proven; the frequency of these rare events is difficult to estimate.
Overdose
It is possible to prescribe Spiriva® in combination with other drugs commonly used to treat COPD: sympathomimetics, methylxanthine derivatives, oral and inhaled corticosteroids. Combined use with long-acting beta2-agonists, inhaled corticosteroids and their combinations does not affect the effect of tiotropium.
Limited information on combined use with anticholinergic drugs comes from two clinical studies: a single dose of ipratropium bromide during chronic administration of Spiriva in patients with COPD (64 people) and healthy volunteers (20 people) did not reduce adverse reactions, changes in vital parameters and ECG. However, the chronic combined use of anticholinergic drugs and Spiriva® has not been studied and is therefore not recommended.
Storage conditions
The drug should be stored out of the reach of children at a temperature not exceeding 25°C; do not freeze. Shelf life: 2 years.
Once opened, the blister should be used within 9 days.
Conditions for dispensing from pharmacies
The drug is available with a prescription.
RU/SPRES-171477
Special Instructions
The drug Spiriva® is not intended for the relief of acute attacks of bronchospasm.
After inhalation of Spiriva powder, immediate hypersensitivity reactions may develop.
The process of inhalation of Spiriva (as well as other inhaled drugs) can cause bronchospasm.
Patients with renal insufficiency (creatinine clearance ≤50 ml/min) should be carefully monitored when prescribing Spiriva.
Patients should be familiarized with the rules for using the inhaler. Do not allow the powder to get into your eyes. Eye pain or discomfort, blurred vision, visual halos in combination with eye redness, conjunctival congestion and corneal edema may indicate an acute attack of angle-closure glaucoma. If any combination of these symptoms develops, the patient should consult a doctor immediately. The use of only drugs that cause miosis is not an effective treatment in this case.
One capsule contains 5.5 mg of lactose monohydrate.
Impact on the ability to drive vehicles and operate machinery
No studies have been conducted to study the effect of the drug on the ability to drive vehicles and operate machinery. Cases of dizziness and blurred vision while using the drug may have a negative impact on the above-mentioned ability.