Periarteritis nodosa
Periarteritis nodosa is an inflammatory lesion of the arterial wall of small and medium-sized vessels leading to progressive organ failure with the formation of microaneurysms.
Epidemiology
Due to the rarity of the disease, its epidemiology is poorly studied. 0.2-1 cases per 100,000 population are recorded annually. The average age of onset of the disease is 48 years. Men get sick 3-5 times more often than women.
Etiology
There is no clear cause of the disease. Currently, two main factors have been identified:
- drug intolerance;
- persistence of hepatitis B virus.
There are already about a hundred medications that have been associated with the occurrence of periarteritis nodosa.
In 30-40% of patients, hepatitis B surface antigen (HBsAg) or immune complexes including it, as well as other hepatitis B antigens (HBeAg) and antibodies to the HBcAg antigen, formed during viral replication, were detected in the blood. It is known that in France, the incidence of HBV-associated polyarteritis nodosa has decreased from 36% in the early 1980s to less than 5% in the 2000s, due to mass vaccination against hepatitis B.
Also, 5-12% of patients have hepatitis C virus, but its role in causing the disease has not yet been proven. Other viruses are also being considered: HIV, cytomegalovirus, Epstein-Barr virus, rubella, parvovirus B 19, human T-lymphotropic virus type 1, but their role has not yet been proven.
Separate observations have also been published on the occurrence of symptoms of polyarteritis nodosa after administration of a vaccine against hepatitis B and influenza.
Another suspected etiological factor is hereditary predisposition, but it has not yet been possible to establish a connection with a specific HLA antigen.
Pathogenesis
Pathogenesis consists of a hyperallergic reaction of the body in response to etiological factors, an autoimmune antigen-antibody reaction (including to the vascular wall), and the formation of immune complexes.
Since endothelial cells have receptors for the Fc fragment of IgG and the first fraction of complement Clq, this facilitates the interaction of immune complexes with the vascular wall. Immune complexes are deposited in the vascular wall, which leads to the development of immune inflammation in it.
The formed immune complexes activate complement, which causes vascular damage, as well as the formation of chemotactic substances that attract neutrophils to the lesion. They phagocytose immune complexes, but in this case they release lysosomal proteolytic enzymes that damage the structures of the vascular wall. Neutrophils are also able to adhere to the endothelium and, in the presence of complement, release activated oxygen radicals, which aggravate vascular damage.
The endothelium also increases the release of factors that promote blood clotting and thrombus formation in the inflamed vessel.
Clinical picture
The disease usually begins with general syndromes: constant fever, progressive weight loss, muscle and joint pain.
Fever occurs in 95-100% of patients, usually of the wrong type, unresponsive to antibiotics, but disappears with corticosteroids. As a rule, it disappears later, when organ pathology appears.
Weight loss with periarteritis nodosa is pathognomic. In some cases, body weight decreases by 30-40 kg in a few months, and the degree of cachexia is higher than in cancer.
Myalgia and, less commonly, arthralgia occur at the onset of the disease. They manifest themselves as characteristic pain in the calf muscles and large joints.
With the development of periarteritis nodosa, five types of organ pathologies are most common. They determine the specific clinical picture of the disease.
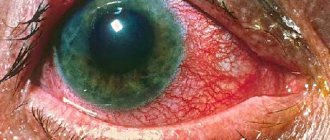
- Renal vascular lesions occur in 75-90% of patients. The appearance of symptoms indicates a deep stage of the disease. Arterial hypertension usually develops, stable, persistent, leading to severe retinopathy and even loss of vision.
Proteinuria (1-3 g per day), microhematuria, and occasionally macrohematuria are observed in the urine.
In some patients, the aneurysmally dilated vessel ruptures with the formation of a perinephric hematoma.
Kidney damage in chronic periarteritis nodosa usually leads to the development of renal failure within 1-3 years.
- When the blood vessels of the organs and tissues of the abdominal cavity are affected, symptoms often appear in the early stages of the disease. Abdominal pain is typical, diffuse, persistent, and increasing in intensity.
Dyspeptic symptoms are also characteristic: usually diarrhea with a stool frequency of up to 6-10 times a day mixed with blood. Anorexia, nausea, and vomiting occur.
Peritonitis often develops as a result of perforation of an ulcer or intestinal gangrene. Gastrointestinal bleeding is possible.
- In 50-70%, damage to the coronary vessels of the heart occurs, although usually not accompanied by anginal pain.
Myocardial infarctions develop, mostly small focal ones. Cardiosclerosis progresses rapidly, which leads to rhythm disturbances, conduction disturbances, and heart failure.
- Lung damage occurs in about a third of patients with periarteritis nodosa.
Manifested by bronchospasms, hypereosinophilia, eosinophilic pulmonary infiltrates.
The development of vascular pneumonia is typical, characterized by a cough with a scanty amount of sputum, occasionally hemoptysis, and increasing signs of respiratory failure.
X-ray examination shows a sharp increase in the vascular pattern, reminiscent of congestive lung, infiltration of lung tissue, mainly in the hilar zones.
- Damage to the peripheral nervous system occurs in approximately half of patients.
Manifested by the development of asymmetric mono- or polyneuritis. Sharp pain, paresthesia, and sometimes paresis are observed. The lower extremities are mainly affected. Sometimes a picture of polymyeloradiculoneuritis with paresis of the hands and feet develops.
In some patients (15-30%), nodular formations (which give the name of the disease) can be identified along the vascular trunks. Sometimes ulcerative-necrotic changes in the skin occur.
Sometimes damage to peripheral vessels with periarteritis nodosa can lead to soft tissue necrosis and the development of gangrene.
Diagnostics
The diagnosis is established on the basis of anamnesis (drug allergy, persistence of the hepatitis B virus), a typical polysyndromic clinical picture of the disease, and laboratory test results.
However, laboratory tests for periarteritis nodosa are nonspecific. Their diagnostic value is low; the indicators reflect mainly the degree of activity of the process.
The following diagnostic criteria for periarteritis nodosa are distinguished:
- Weight loss of more than 4 kg - loss of body weight of 4 kg or more since the onset of the disease, not related to dietary habits
- Livedo reticularis is a branched change in skin pattern on the limbs and torso.
- Testicular tenderness - a feeling of soreness in the testicles that is not associated with infection or injury
- Myalgia, weakness or soreness in the muscles of the legs - diffuse myalgia (excluding the shoulder girdle or lumbar region) or weakness and soreness in the muscles of the lower extremities
- Mononeuritis or polyneuropathy - development of corresponding neurological manifestations
- Diastolic blood pressure is more than 90 mm Hg. st - increased blood pressure
- Increased levels of urea or creatinine in the blood - urea content more than 14.4 mmol/l (40 mg%) or creatinine more than 133 µmol/l (1.5 mg%), not associated with dehydration or obstruction of the urinary tract
- Hepatitis B virus - the presence of HBsAg or antibodies to it in the blood serum
- Arteriographic changes - aneurysms or occlusions of visceral arteries during arteriography, not associated with atherosclerosis, fibromuscular dysplasia and other non-inflammatory diseases
- Biopsy of small and medium-sized arteries - granulocytic and mononuclear cell infiltration of the vessel wall during morphological examination
The presence of 3 or more of any criteria allows you to make a diagnosis of periarteritis nodosa.
Treatment
The basis of treatment is glucocorticoids, which are most effective in the early stages of the disease. With long-term use of prednisolone, stabilization of hypertension, progression of retinopathy and renal failure are observed. In acute cases, a paradoxical effect of corticosteroids with the development of multiple infarctions is possible. Also, corticosteroids can dramatically worsen the course of malignant hypertension syndromes. To reduce complications, it is also recommended to use cytotoxic drugs - cyclophosphamide and azathioprine.
Forecast
Without treatment, the prognosis is extremely unfavorable. The disease occurs at lightning speed, or with periodic exacerbations against the background of steady progression. The cause of death is renal failure, gastrointestinal lesions (especially intestinal infarction with perforation), and cardiovascular pathologies. Often, damage to the kidneys, heart and central nervous system is aggravated by persistent arterial hypertension, which is associated with late complications.
The five-year survival rate without treatment does not exceed 13%; with treatment with corticosteroids it reaches 40%. The labor prognosis is questionable due to the persistence of complications of the disease - peripheral and central paralysis, severe hypertension, heart damage and others.
Etiology
There is no clear cause of the disease. Currently, two main factors have been identified:
- drug intolerance;
- persistence of hepatitis B virus.
There are already about a hundred medications that have been associated with the occurrence of periarteritis nodosa.
In 30-40% of patients, hepatitis B surface antigen (HBsAg) or immune complexes including it, as well as other hepatitis B antigens (HBeAg) and antibodies to the HBcAg antigen, formed during viral replication, were detected in the blood. It is known that in France, the incidence of HBV-associated polyarteritis nodosa has decreased from 36% in the early 1980s to less than 5% in the 2000s, due to mass vaccination against hepatitis B.
Also, 5-12% of patients have hepatitis C virus, but its role in causing the disease has not yet been proven. Other viruses are also being considered: HIV, cytomegalovirus, Epstein-Barr virus, rubella, parvovirus B 19, human T-lymphotropic virus type 1, but their role has not yet been proven.
Separate observations have also been published on the occurrence of symptoms of polyarteritis nodosa after administration of a vaccine against hepatitis B and influenza.
Another suspected etiological factor is hereditary predisposition, but it has not yet been possible to establish a connection with a specific HLA antigen.
Treatment
The basis of treatment is glucocorticoids, which are most effective in the early stages of the disease. With long-term use of prednisolone, stabilization of hypertension, progression of retinopathy and renal failure are observed. In acute cases, a paradoxical effect of corticosteroids with the development of multiple infarctions is possible. Also, corticosteroids can dramatically worsen the course of malignant hypertension syndromes. To reduce complications, it is also recommended to use cytotoxic drugs - cyclophosphamide and azathioprine.
Without treatment, the prognosis is extremely unfavorable. The disease occurs at lightning speed, or with periodic exacerbations against the background of steady progression. The cause of death is renal failure, gastrointestinal lesions (especially intestinal infarction with perforation), and cardiovascular pathologies. Often, damage to the kidneys, heart and central nervous system is aggravated by persistent arterial hypertension, which is associated with late complications.
The five-year survival rate without treatment does not exceed 13%; with treatment with corticosteroids it reaches 40%. The labor prognosis is questionable due to the persistence of complications of the disease - peripheral and central paralysis, severe hypertension, heart damage and others.
Types and classification of vasculitis
Vasculitis is one of the most serious diseases. The inflammatory process can affect both small vessels of the circulatory system (capillaries, arterioles and venules) and large ones (aorta and its large branches). The affected blood vessels can be located shallowly under the skin, in the internal organs themselves and in any cavities.
Depending on the cause of the disease, there are 2 types of systemic vasculitis:
- primary vasculitis (identified as an independent disease in which the vessels themselves become inflamed);
- secondary vasculitis (appears as a result of other diseases or is the body’s reaction to an infection).
According to the generally accepted classification, primary vasculitis can be divided into three groups, depending on the size of the inflamed vessels:
- inflammation of small vessels (hemorrhagic vasculitis (Henoch-Schönlein purpura), Wegener's granulomatosis (vasculitis), microscopic polyangiitis, cryoglobulinemic vasculitis, Charge-Strauss syndrome);
- inflammation of the middle vessels (periarteritis nodosa, Kawasaki disease);
- inflammation of large vessels (giant cell arteritis (or temporal arteritis, Horton's disease), Takayasu's disease);
There is also isolated “skin vasculitis”, which can be a manifestation of the following diseases:
- (hypersensitive allergic vasculitis, Henoch-Schönlein hemorrhagic vasculitis;
- erythema nodosum, vasculitis nodosum, periarteritis nodosum).
Vasculitis can also affect various human organs:
vasculitis of the brain, vasculitis of the lungs, vasculitis of the lower extremities, vasculitis of the eyes. Eyes with vasculitis can be very damaged (inflammation of the retinal arteries can lead to hemorrhages and partial loss of vision).
Usually people who first encounter this disease are interested in whether vasculitis is contagious. Primary vasculitis is not contagious and is not dangerous to others, but secondary (infectious) vasculitis, which appears against the background of infectious diseases, such as meningitis, can pose an epidemic danger.
Vasculitis during pregnancy can not only provoke delayed fetal development, but also lead to miscarriage.
3.Symptoms
There are several clinical variants of periarteritis nodosa, which differ quite strongly from each other (cutaneous, asthmatic, etc.). Thus, the skin form with the formation of specific granuloma nodules, which gave the name of the disease, occurs only in 20-25% of cases and is distinguished by a significant variety of manifestations (marble pallor, pigmentation, rash of one or another nature, color and distribution). However, the further development of the clinical picture is determined by which internal organs suffer the most due to circulatory disorders, which in turn are caused by necrotizing fibrosis, thrombosis, and aneurysms. Typical is the formation of joint-muscular, cardiovascular, renal, pulmonary syndromes, often in combination with severe arterial hypertension, damage to the central nervous system and gastrointestinal tract, visual organs, and endocrine glands. In many cases, there is a febrile state that is practically not controlled by antibiotics or anti-inflammatory drugs.
The course of the disease also varies widely in different cases - from benign and slowly progressing to fulminant, with death a few months after manifestation.
The natural consequences of necrotizing fibrosis of arterioles include ischemia and infarction of internal organs, hemorrhages due to rupture of aneurysms, perforated ulcers, severe damage to the meninges, which sooner or later results in disability.
Symptomatically, periarteritis nodosa can imitate many diseases, so evidence-based diagnosis requires their exclusion. Differential diagnosis is carried out on the basis of clinical and laboratory criteria (microscopic analysis of skin samples is considered the most informative). Instrumental methods usually include Doppler sonography, angiography, and chest x-ray.
About our clinic Chistye Prudy metro station Medintercom page!
Pathogenesis
Pathogenesis consists of a hyperallergic reaction of the body in response to etiological factors, an autoimmune antigen-antibody reaction (including to the vascular wall), and the formation of immune complexes.
Since endothelial cells have receptors for the Fc fragment of IgG and the first fraction of complement Clq, this facilitates the interaction of immune complexes with the vascular wall. Immune complexes are deposited in the vascular wall, which leads to the development of immune inflammation in it.
The formed immune complexes activate complement, which causes vascular damage, as well as the formation of chemotactic substances that attract neutrophils to the lesion. They phagocytose immune complexes, but in this case they release lysosomal proteolytic enzymes that damage the structures of the vascular wall. Neutrophils are also able to adhere to the endothelium and, in the presence of complement, release activated oxygen radicals, which aggravate vascular damage.
The endothelium also increases the release of factors that promote blood clotting and thrombus formation in the inflamed vessel.
Causes of vasculitis
Doctors cannot yet fully determine the causes of primary vasculitis. There is an opinion that this disease is hereditary in nature and is associated with autoimmune disorders (autoimmune vasculitis), plus negative external factors and infection with Staphylococcus aureus play a role.
The cause of the development of secondary (infectious-allergic vasculitis) in adults is a previous infection.
Other causes of vasculitis include the following:
- allergic reaction (to medications, pollen, book dust, fluff);
- autoimmune diseases (systemic lupus erythematosus, thyroid diseases);
- vaccination;
- abuse of sunbathing;
- consequences of injuries;
- negative reaction of the body to various chemicals, poisons;
- hypothermia of the body;
1 Consultation with an ophthalmologist
2 Consultation with a neurologist
3 ENT consultation
Diagnostics
The diagnosis is established on the basis of anamnesis (drug allergy, persistence of the hepatitis B virus), a typical polysyndromic clinical picture of the disease, and laboratory test results.
However, laboratory tests for periarteritis nodosa are nonspecific. Their diagnostic value is low; the indicators reflect mainly the degree of activity of the process.
The following diagnostic criteria for periarteritis nodosa are distinguished:
Weight loss of more than 4 kg - a loss of body weight of 4 kg or more since the onset of the disease, not associated with dietary habits Livedo reticularis - a branched change in the skin pattern on the limbs and torso Soreness in the testicles - a feeling of soreness in the testicles, not associated with infection, injury Myalgia , weakness or soreness in the muscles of the legs - diffuse myalgia (excluding the shoulder girdle or lumbar region) or weakness and soreness in the muscles of the lower extremities Mononeuritis or polyneuropathy - development of corresponding neurological manifestations Diastolic blood pressure more than 90 mm Hg. Art. - increased blood pressure Increased level of urea or creatinine in the blood - urea content is more than 14.4 mmol/l (40 mg%) or creatinine is more than 133 µmol/l (1.5 mg%), not associated with dehydration or obstruction of the urinary tract Hepatitis B virus - presence of HBsAg or antibodies to it in the blood serum Arteriographic changes - aneurysms or occlusion of visceral arteries during arteriography, not associated with atherosclerosis, fibromuscular dysplasia and other non-inflammatory diseases Biopsy of small and medium-sized arteries - granulocytic and mononuclear cell infiltration of the vessel wall during morphological examination Presence 3 and more than any criteria allows you to make a diagnosis of periarteritis nodosa.
Clinical picture
Initial symptoms are:
- fever (simultaneous increase in body temperature and chills);
- progressive weight loss;
- pain in muscles and joints.
With further development of the pathology, signs of damage to many organs and tissues appear:
- deterioration and loss of vision;
- stomach ache;
- dyspeptic symptoms – diarrhea, nausea, vomiting;
- bronchospasm;
- necrosis of soft tissues.
What does the treatment of polyarteritis nodosa depend on? Clinical recommendations are based on the reported manifestations.