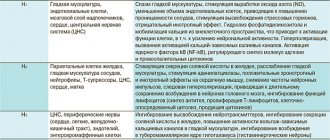
Antihistamines are aimed at eliminating allergies in all its manifestations. During their action, the drugs block special receptors that are involved in the development of an allergic reaction. Especially if this is an immediate reaction, where the main role belongs to an organic compound - histamine. Under provoking factors, histamine becomes active in the human body and can lead to such types of allergies as:
- allergic rhinitis;
- allergic conjunctivitis;
- hives;
- angioedema;
- reaction to an insect bite;
- allergies to medications (tablets, sprays, etc.);
- food allergies;
- skin allergies, allergic dermatosis.
Taking an antihistamine (drops, tablets, ointment) in these cases is the first line of treatment. All medications in the form of tablets or drops act on H1 receptors located in the brain, blood vessels, smooth muscles, cardiac tissue, cartilage tissue, etc. [1].
The role of histamine in allergic reactions
Histamine is a biologically active substance produced by the body to regulate vital functions (blood circulation, respiration, digestion). It is concentrated in mast cells, white blood cells that are part of the immune system.
Under normal conditions, there is little histamine in the human body and it is inactive. But when certain substances enter the body, their active production begins. When the allergen binds to immunoglobulin, mast cells degranulate (release substances that cause an inflammatory response). Histamine is released, leaves the cells, and the body comes under its influence. It causes:
- hives;
- swelling of the mucous membranes;
- bronchospasms;
- decreased blood pressure;
- digestive disorders;
- confusion;
- slowing down the conduction of nerve impulses.
The first three reactions are allergic. They are the immune system's response to contact with an irritant. Most allergic reactions develop immediately.
Discussion
Since during exacerbation of itchy dermatoses the leading symptom is largely itching, the prescription of antipruritic drugs is justified.
At the present stage, the most commonly used group of drugs is topical glucocorticosteroids, which have anti-inflammatory, antiallergic, and immunosuppressive effects. However, despite the creation of a new generation of topical glucocorticosteroids with minimal side effects, their application over large areas and for a long time leads to an increase in the steroid load on the skin and the development of its dystrophy. In addition, the antipruritic effect of topical glucocorticosteroids is often insufficient for rapid and long-term relief of itching.
Choosing an effective and safe drug for the treatment of pruritic dermatoses, which has a pronounced antipruritic effect, turned out to be a difficult task. In our choice, we settled on the Neotanin series of drugs,
including lotion, spray and cream.
The main active components of the Neotanin
are synthetic tannin and polidocanol; zinc oxide is added to the lotion.
M. Puschmann and C. Matthies proved the antipruritic effect of tannin using the histamine blister test and stimulation of the lip mucosa [9, 10]. The histamine blister test was performed on 85 healthy volunteers. Due to the important role of skin mast cells as effector cells in immediate allergic reactions and diseases accompanied by itching, T. Zuberbier et al. [11] studied the effect of synthetic tannin on IgE —
dependent activation of human mast cells. The effect of tannin was manifested in a dose-dependent inhibition of anti-IgE-induced histamine release. The effect appeared to be more pronounced than that observed with dexamethasone. In addition to antipruritic, synthetic tannin has astringent, anti-inflammatory, antimicrobial effects, and reduces transepidermal water loss [12].
The second active component of the Neotanin
is polidocanol, which has an antipruritic effect. The antipruritic effect of polidocanol develops 5-10 minutes after application to the skin, the duration of action is on average 3-4 hours. Polidocanol also enhances the astringent, drying effect of tannin, promotes the healing of erosions, has an anesthetic effect on the skin and mucous membranes, reduces sensitivity and conductivity sensory nerves. Polidocanol as an antipruritic and local anesthetic is included in the European Guidelines for Chronic Itching (2012), Recommendations of the Association of Scientific Medical Societies in Germany (AWMF) for the diagnosis and treatment of atopic dermatitis (2016), Recommendations of the European Dermatological Forum (EDF) on the treatment of atopic eczema / atopic dermatitis (2018) [13-15].
What can trigger an increase in histamine?
Allergens are substances that provoke increased release of histamine. Medicine has studied many allergens that can be divided into such groups.
Exogenous infectiousExogenous non-infectiousEndogenousVirusesFoodProtein-containing compounds that make up the cells of the bodyBacteriaPolenFungiIndustrialHouseholdMedicinal
Endogenous allergens are produced by the body itself. They cause autoimmune diseases (attacks of the immune system on healthy tissues).
Exogenous ones enter the body from the environment - through food, plant pollen, house dust. Industrial allergens include a variety of chemicals (dyes, cleaning products, fragrances).
Symptoms of an allergic reaction
A wide range of symptoms is known, but this does not mean that the same clinical picture occurs upon contact with all allergens. Depending on the type of hypersensitivity, the body reacts differently:
- atopic: rhinitis, conjunctivitis, dermatitis, asthma, Quincke's edema;
- reagin: inflammation of the mucous membranes, autonomic disorders;
- cytotoxic immune: damage to cells and tissues (immune thrombocytopenia, hemolytic anemia, etc.);
- immunocomplex: inflammation of joints, kidneys, skin manifestations.
There are also delayed-type reactions that do not make themselves felt immediately upon contact with the irritant. After two days, the allergen combines with lymphocytes, which leads to the development of an infectious-allergic disease, for example, chronic neurodermatitis.
TOP allergy drugs
Below we look at the 15 most common active ingredients against allergies. Please note that the name of the active substance often does not coincide with the name of the medicine.
Chloropyramine
Generation: first
Trade names: “Suprastin”, “Suprilamin”, “Suprivell”, “Gistaprim”, “Chloropyramine”.
Chloropyramine is mainly available in tablets. But there are also forms for intramuscular administration. The drug has a pronounced antihistamine effect. Relief occurs within 15-30 minutes after administration². After an hour, the maximum concentration of the drug in the blood is reached.
Chloropyramine-based medications usually work within 4-6 hours. Such products not only block the production of histamine, but also relieve swelling and itching. Chloropyramine also has an inhibitory effect on the central nervous system (calming and sedative effects).
Contraindications: hypersensitivity to the components of the drug, severe forms of prostate adenoma, pregnancy and breastfeeding.
Clemastine
Generation: first
Trade names: “Tavegil”, “Clemastin”, “Clemastin-Eskom”.
Preparations with clemastine are available in tablets, syrups and solutions for intramuscular administration. This is an over-the-counter medicine that works within 8-12 hours.
Clemastine is used to suppress acute allergic reactions. Also used in the complex treatment of anaphylactic reactions.
Contraindications: hypersensitivity to the components of the drug, age under 6 years (tablets) or under 1 year (syrup or injections), pregnancy, breastfeeding.
Loratadine
Generation: second
Trade names: “Claritin”, “Klarnedin”, “LoraGexal”, “Clarifer”, “Erolin”, “Clarotadine” and others.
Loratadine helps cope with the classic symptoms of allergies - sneezing, itching and runny nose³. The therapeutic effect of the drug occurs quickly, after 30-40 minutes and lasts up to 24 hours.
Side effects of loratadine include headache (in 12% of cases), drowsiness (8%), fatigue (4%). In rare cases (less than 2%), loratadine impairs concentration.
Contraindications: hypersensitivity to the components of the drug, children under 2 years of age.
During pregnancy, loratadine is taken if the expected benefit outweighs the potential risk to the fetus.
Figure 2. Allergy symptoms. Image: inspiration/freepik.com
Cetirizine
Generation: second
Trade names: “Zirtec”, “Zintset”, “Alerza”, “Zodak”, “Parlazin”, “Cetirizine”, “Solonex” and others.
Cetirizine has a long-lasting antiallergic effect and is practically free of sedative effect. The drug relieves swelling and itching. During the flowering season, cetirizine preparations can also be used for preventive purposes.
The most common form for cetirizine is tablets. Also available in the form of drops. Used to relieve nasal, eye and skin allergy symptoms.
Contraindications: hypersensitivity to cetirizine, late stage of renal failure. Cetirizine in the form of drops is not prescribed to children under 6 months. Tablet forms of the drug are allowed from the age of 6 years. Cetirizine should not be used during pregnancy due to the lack of clinical studies regarding its safety in pregnant women.
Desloratadine
Generation: third
Trade names: “Erius”, “Espontin”, “Lordestin”, “Nalorius”, “Delorsin”, “Desloratadine”, “Dezal”, “Blogir-3” and others.
Medicines based on desloratadine are available in the form of tablets or syrup. The active substance has a long-term antiallergic and anti-inflammatory effect, which lasts up to 24 hours.
Desloratadine is used to treat seasonal and perennial allergic rhinitis and urticaria.
Contraindications: hypersensitivity to the components of the drug, pregnancy and breastfeeding. The syrup should not be taken by children under 1 year of age, and tablet forms of the drug should not be taken by children under 12 years of age.
What to do if you don’t have the drug at hand?
- Even disciplined allergy sufferers (who always carry the necessary medications with them) can find themselves in a situation where there is no life-saving remedy at hand. In such situations, you need to act depending on the type of allergy:
- For allergies to pollen. Rinse your eyes, face and hair. Change clothes as quickly as possible. A lot of pollen settles on hair and clothes.
- For food allergies. Drink more water. If the allergic attack does not subside, induce vomiting.
- If you are allergic to an insect bite. To relieve swelling and inflammation, apply something cold to the bite. This can be a bottle of cold water or a towel soaked in water. If you have ice on hand, wrap it in a cloth and apply it to the bite. Do not apply ice to bare skin!
Diphenhydramine
Generation: first
Trade names: "Diphenhydramine".
Diphenhydramine is available in the form of tablets, gels and solutions for intramuscular administration. The drug is used for a wide range of allergic diseases, including hay fever, vasomotor rhinitis, urticaria, anaphylactic shock and others. Diphenhydramine is also used in the treatment of bronchial asthma, gastric ulcers, sea and airborne illnesses.
Preparations in the form of a gel are used to treat skin allergic diseases and sunburn.
Contraindications: hypersensitivity to the components of the drug, breastfeeding, childhood (newborn period).
Important!
Drugs containing diphenhydramine are used with caution in glaucoma, pregnancy and prostate adenoma. In such cases, the doctor assesses the potential risks of the drug, on the basis of which he decides whether to prescribe the medicine or not.
Ebastine
Generation: second
Trade names: “Ebastine”, “Espa-Ebastine”, “Kestin”, “Zirtal-10”.
Products with ebastine are used for allergic rhinitis, chronic urticaria and diseases with high histamine release.
Contraindications: hypersensitivity to the drug, pregnancy, age under 12 years.
Mebhydrolin
Generation: first
Trade names: "Diazolin".
Diazolin is available in tablets or dragees. It is effective for allergic rhinitis, hay fever, allergic conjunctivitis and skin allergic manifestations. It is also used in the complex treatment of itchy dermatoses.
Contraindications: hypersensitivity, exacerbation of gastric and duodenal ulcers, inflammatory diseases of the digestive system, prostate adenoma.
Astemizole
Generation: second
Trade names: “Gistalong”, “Asmoval 10”, “Mibiron”, “Stemiz”.
Preparations containing astemizole are available in the form of tablets and suspensions. Used for nasal, eye and skin allergic reactions. Also used for adjuvant therapy of bronchial asthma.
Contraindications: hypersensitivity, pregnancy and breastfeeding, children under 2 years of age.
Allergy medicine should be in every first aid kit. Photo: ufabizphoto / freepik.com
Promethazine
Generation: first
Trade names: "Pipolfen".
Promethazine is used for a wide range of allergic reactions. These are numerous skin manifestations, drug allergies, asthmatic bronchitis, anaphylactic and anaphylactoid reactions. The drug is also used for rheumatic lesions, neuralgia, neurosis-like conditions and psychoses.
Contraindications: hypersensitivity, coma, combination with monoamine oxidase inhibitors (MAO). Promethazine should not be taken in a state of alcohol intoxication, renal or liver failure. The drug is prohibited during pregnancy, breastfeeding and in early childhood under 6 years of age.
Hormonal medications for allergies
For allergies, not only antihistamines are used, which our material is devoted to.
In severe forms of an allergic reaction, corticosteroids are also used to relieve the inflammatory process. These are hormonal anti-inflammatory drugs that have a pronounced effect. Corticosteroids are prescription medications that can only be prescribed by a doctor. They are used to relieve bronchospasms, skin lesions and nasal congestion. They are produced in the form of tablets, sprays, ointments, as well as solutions for injections.
Levocetirizine
Generation: third
Trade names: “Xizal”, “Suprastinex”, “Glenset”, “Cetrin”, “Zodak”, “Elcet”.
Levocetirizine is available in the form of tablets and drops. Used for year-round and seasonal allergic rhinitis and conjunctivitis. The drug is effective for hay fever, urticaria, and allergic skin diseases.
Contraindications: hypersensitivity to levocetirizine, cetirizine, hydroxyzine and other piperazine derivatives. The drug should not be taken in case of end-stage renal failure, as well as in children under 2 years of age (drops) and 6 years of age (tablets).
Akrivastine
Generation: second
Trade names: Semprex.
Akrivastine is available in capsule form. The medicine is used against allergic rhinitis, as well as allergic skin reactions. The sedative effect is weak. However, in rare cases, such a side effect does occur (like insomnia). The antihistamine effect of acrivastine lasts approximately 12 hours.
Contraindications: hypersensitivity, pregnancy and lactation, children under 12 years of age, severe renal failure.
Azelastine
Generation: first
Trade names: “Azelastine-Xantis”, “Allergodil”.
The drug is available in the form of a nasal spray and drops (nasal and eye). Used to treat seasonal or year-round allergic rhinitis and conjunctivitis.
Contraindications: hypersensitivity to the drug, pregnancy, breastfeeding. Eye drops should not be used by children under 4 years of age, and sprays and nasal drops by children under 6 years of age.
Dimetinden
Generation: first
Trade names: “Fenistil”, “Phenicitol”, “Dimetinden”, “Allergolan”, “Akristil”.
Antiallergic drugs based on dimethindene are used for external use and oral administration. Available in the form of drops, capsules, gels and emulsions.
Capsules and drops for internal use are prescribed for hay fever, urticaria, eczema, angioedema, food and drug allergies, as well as reactions to insect bites.
Gels and emulsions for external use are used for itchy dermatoses, urticaria, and burns.
Contraindications: hypersensitivity, 1st trimester of pregnancy, newborn period.
Fexofenadine
Generation: third
Trade names: “Allegra”, “Fexofast”, “Telfast”, “Fexadin”, “Fexofen”.
Fexofenadine is produced in the form of tablets, capsules and drops. It is used to treat urticaria, itching, and allergic symptoms of the upper respiratory tract4.
Contraindications: hypersensitivity to the components of the drug, children under 6 years of age.
How to eliminate allergy symptoms
The more free histamine is released, the more severe the allergic reaction. In some cases it causes inconvenience (constant sneezing, itchy eyes), in others it poses a threat to life (with bronchospasm a person cannot breathe). You can stop the reaction:
- stopping contact with the allergen;
- neutralizing histamine with an antihistamine;
- symptomatic therapy (for example, inhalation to immediately expand the lumens of the bronchi).
In the event of the development of anaphylactic shock, accompanied by a decrease in blood flow and laryngeal edema, it is important to promptly eliminate the threat to life. The set of measures includes the administration of adrenaline and ensuring air flow into the lungs (intubation).
Differences between the first generation of drugs
Some time ago, only first-generation drops and tablets were used to treat allergies, and they had quite a lot of disadvantages. The main disadvantage of type 1 antihistamines is poor and quickly reversible contact with histamine receptors. This meant that the drugs had to be used in large quantities, which inevitably led to addiction and side effects. By acting directly on brain receptors, they almost always resulted in:
- to vision problems;
- to the development of dry mouth;
- to a slowdown of all reactions associated with the central nervous system - drowsiness, lethargy, attention disorder;
- to the development of arrhythmia and other heart rhythm disturbances;
- to increased excitability, aggression, hyperactivity;
- to digestive disorders, including constipation.
First generation medications gave relatively quick results, alleviating the patient’s symptoms, but this effect did not last long. The risk of addiction was unreasonably high, but medicine could not offer any alternatives.
Types of antihistamines
First-generation drugs could block histamine receptor signals only after penetrating the barrier between the circulatory and central nervous systems. As a result, the effects on the central nervous system could not be avoided. Because of this, antihistamines caused drowsiness and loss of coordination.
Pharmacologists took this shortcoming into account when creating second-generation drugs. They do not penetrate the mentioned barrier, act selectively, and do not have a sedative effect.
Third generation antihistamines are metabolites of their predecessors. They give the same effect at a lower dosage and do not affect the functioning of the cardiovascular system. However, some allergists and immunologists do not agree with separating them into a separate group and classify them as the second generation.
In 2015, the Consensus working group on new generation antihistamines led by Professor S.T. Holgate concluded that none of the existing drugs can be classified as third generation.
Examples of AGPs of different generations
AGP 1st generationAGP 2nd generationAGP 3rd generation*DiphenhydramineLoratadineCetirizineTavegilClaritinZyrtecSuprastinKestinCetrinDramamineVisin and Tizin AllergiTelfastDiazolinAllergodilFexofenadineAtarkcFenistilAllerfex
*according to supporters of their existence
Sources
1. Scudellari M. (2017).
News Feature: Cleaning up the hygiene hypothesis. Proceedings of the National Academy of Sciences of the United States of America, 114(7), 1433–1436. https://doi.org/10.1073/pnas.1700688114 2. State register of medicines. Instructions for use of the drug for medical use CHLOROPYRAMINE https://grls.rosminzdrav.ru/ImgInstr.aspx?folder=ScanVavilova&Filepath=\Vneseno_v_Grls\454954\IP&idReg=160167&isOld=1&fileType=jpg&pfolder=2
3. Tenn MW, Steacy LM, Ng CC, Ellis AK. Onset of action for loratadine tablets for the symptomatic control of seasonal allergic rhinitis in adults challenged with ragweed pollen in the Environmental Exposure Unit: a post hoc analysis of total symptom score. Allergy Asthma Clin Immunol. 2018;14:5. Published 2022 Jan 16. doi:10.1186/s13223-017-0227-4
4. Axelrod, David, and Leonard Bielory. “Fexofenadine hydrochloride in the treatment of allergic disease: a review.” Journal of asthma and allergy vol. 1 19-29. 19 Sep. 2008, doi:10.2147/jaa.s3092
Features of the action of antihistamines
First generation antihistamines are not limited to suppressing the activity of the central nervous system. They block receptors for various neurotransmitters, not just histamine, and therefore have a number of side effects:
- increased heart rate;
- nausea and vomiting;
- increased eye pressure;
- stomach pain;
- urinary disturbance;
- dry mucous membranes.
With prolonged use, the patient may lose weight, become overexcited, and lose consciousness. In case of overdose, convulsions are possible.
Second-generation antihypertensives act more selectively, and therefore their use does not cause undesirable reactions from organs other than the heart. Patients should consider the risk of sinus and reflex tachycardia, as well as arrhythmias.
Material and methods
The clinical study was conducted from October 2022 to April 2019. This study was an open comparative study. The study included 40 patients of both sexes aged from 7 to 43 years with itchy dermatoses in the acute stage with and without weeping, including those complicated by secondary infection, with comparable lesions on the mirror parts of the body. 27 patients were diagnosed with atopic dermatitis, 2/3 of them having moderate to severe degrees; 13 patients sought consultation due to exacerbation of hand eczema. Diagnosis of dermatoses was based on a comprehensive assessment of clinical and anamnestic data.
Before starting and during treatment, a clinical assessment of the patient’s condition was carried out:
1. Assessment of subjective clinical signs (patient complaints): itching of the skin, burning, soreness and insomnia. Itching of the skin and the antipruritic effect of therapy were assessed for each half of the body using several parameters:
a) intensity of skin itching according to VAS (10-point system);
b) time (in minutes) after which the itching stops; duration of antipruritic action after morning application of the product;
c) severity of itching, frequency of attacks of itching, duration of itching (assessed over the last week).
2. Assessment of objective signs of inflammation: erythema, swelling, crusts/weeping, excoriation, lichenification, dry skin, cracks/erosions.
3. Assessing the effectiveness of therapy by a doctor:
a) pronounced improvement - resolution of old elements, absence of itching and soreness of the skin;
b) improvement - incomplete resolution of old elements, absence of itching and soreness of the skin;
c) state without change - no changes in the skin;
d) deterioration - deterioration of the clinical picture, the appearance of itching, soreness of the skin.
4. Dermatological quality of life index (DIQL).
The examination was carried out 5 times (once every 2-3 days) for 12-16 days. All patients applied a topical glucocorticosteroid (Akriderm cream) to the affected areas of the skin of one half of the body 2 times a day (morning and evening), lightly rubbing; two drugs were applied to the lesions of the second half of the body - Neotanin
(spray/lotion/cream) and Akriderm cream.
Neotanin
cream was prescribed to 18 patients,
Neotanin
- 12,
Neotanin
- 10. First,
Neotanin
in a thin layer to the affected area of the skin 3-4 times a day. After application, wait until the treated surface dries. After 15 minutes, 2 times a day (morning and evening), apply a thin layer of Akriderm cream to the affected area of the skin, lightly rubbing.
During the study, the prescription of topical (except Akriderm) and systemic glucocorticosteroids, antihistamines and antibacterial drugs, and antiseptics was not allowed. Some patients additionally received concomitant therapy: choleretic, systemic desensitizing agents, external emollients.
Permission from the Ethics Committee was obtained to conduct the study.
For statistical processing of data, the Mann-Whitney, Wilcoxon tests (to assess dynamics), χ2 or two-sided Fisher's exact test were used.
Antihistamines and the stomach
Histamine itself activates the production of gastric juice. Therefore, there is an opinion that blocking it inhibits secretion. This is not entirely true. H1 blockers are used to relieve symptoms of an allergic reaction. H2 blockers can reduce the production of gastric juice:
- Cimetidine;
- Ranitidine;
- Famotidine;
- Roxatidine.
This is another group of antihistamines used to treat gastritis, gastric ulcers, and reflux esophagitis. Allergy sufferers do not use them. Therefore, there is no risk of disrupting digestion in an attempt to combat hives or conjunctivitis.
Suprastin: what helps
Suprastin is a drug that has long been a part of the lives of allergy sufferers and copes well with its functions, including:
- stopping allergic rhinitis;
- getting rid of hives;
- relief of skin itching;
- reducing the severity of the reaction to an insect bite.
An undeniable advantage of Suprastin is its safety in relation to pregnant women. Therefore, it is often prescribed to expectant mothers for seasonal rhinitis. One contraindication should be noted separately: Suprastin should not be taken by patients with glaucoma.
For laryngitis. bronchitis and tracheitis, the prescription of Suprastin must be accompanied by a mandatory condition - the patient must drink plenty of fluids daily. This is due to the fact that a side effect of the drug is drying out of the mucous membranes. Healthy people can easily put up with this, but patients with laryngitis or bronchitis must independently maintain the rheological properties of the sputum discharge so as not to get a complication in the form of pneumonia.