Pharmacodynamics and pharmacokinetics
The drug has a pronounced antihypertensive and vasodilating effect. Its main component is metabolized within the body, resulting in the formation of a pharmacologically active substance - fosinoprilate . The mechanism of therapeutic action is manifested by inhibition of the activity of angiotensin-converting enzyme , which helps prevent the transition of angiotensin-I to angiotensin-II , which has a noticeable vasoconstrictor effect. bradykinin , also slows down . At the same time, the total peripheral vascular resistance decreases, blood pressure , and pre- and afterload on the myocardium .
These tablets are well absorbed from the gastrointestinal tract. The development of the therapeutic effect occurs within an hour, the maximum concentration is reached after 2-6 hours and lasts about 24 hours even with a single use. Long-term use does not contribute to the development of tolerance to fosinopril . This substance is characterized by an increased degree of binding to plasma proteins, about 95%. Excretion of fosinoprilat occurs through the kidneys and liver. On average, the half-life reaches 11.5 hours.
Pharmacological properties of the drug Fosicard
fosinopril is a prodrug, an ester of fosinoprilat, a long-acting ACE inhibitor. After oral administration, fosinopril is quickly and completely converted by hydrolysis into fosinoprilat, which is an active ACE inhibitor. In hypertension (arterial hypertension), the effect of fosinopril is mainly due to its effect on the renin-angiotensin-aldosterone system (RAAS). Inhibition of ACE and a decrease in the concentration of angiotensin II leads to vasodilation, a decrease in sodium and water retention due to inhibition of aldosterone secretion. There may be a slight increase in serum potassium. Inhibition of ACE slows down the breakdown of bradykinin, which is a powerful vasodilator, which also contributes to the therapeutic effect. When taking fosinopril once a day, blood pressure begins to decrease after 1 hour, the maximum effect occurs after 2–6 hours, the hypotensive effect persists for 24 hours. In heart failure, the effect of fosinopril is due to inhibition of the RAAS. ACE inhibition reduces both pre- and afterload. The hemodynamic effect persists for 24 hours when using fosinopril once a day. Treatment with fosinopril improves the performance of patients with heart failure within 24 hours after administration. Treatment with fosinopril reduces the need to increase the dose of diuretics to relieve symptoms of heart failure.
Contraindications for use
It is not recommended to take this drug if:
- hypersensitivity to fosinopril and other components;
- hereditary or idiopathic angioedema ;
- lactation, pregnancy;
- under 18 years of age.
Caution is necessary when:
- renal failure;
- hyponatremia;
- bilateral stenosis of the renal arteries and the artery of the only kidney;
- condition after kidney transplantation, desensitization, some systemic connective tissue diseases;
- hemodialysis;
- cerebrovascular diseases, for example, cerebrovascular insufficiency;
- diabetes mellitus;
- aortic stenosis;
- inhibition of bone marrow hematopoiesis;
- old age and so on.
Side effects
When treated with Fosicard, side effects may occur that affect the activity of all systems and organs. For example, the cardiovascular system may respond with decreased blood pressure, orthostatic hypotension, tachycardia, palpitations, arrhythmia, angina pectoris, myocardial infarction, and chest pain.
Deviations in the functioning of the digestive system in the form of nausea, vomiting, constipation, intestinal obstruction, pancreatitis, hepatitis, stomatitis, glossitis, dyspepsia, abdominal pain, anorexia and so on are also possible.
In addition, it is possible that disorders associated with the activities of the respiratory, urinary and nervous systems .
There is still a possibility of damage to the sensory organs, the development of allergic reactions and changes in laboratory parameters .
Phosicard - instructions for use (Method and dosage)
Fosicard tablets are intended for oral administration. Usually the dosage and duration of treatment are selected individually, but there are a number of standard rules.
According to the instructions for use of Fosicard, during the treatment of arterial hypertension it is recommended to stop taking any antihypertensive drugs in advance.
The initial daily dosage of this drug is 1 time 10 mg. In the future, dose selection is required taking into account blood pressure indicators. In this case, the maintenance daily dose can be 10–40 mg once. If monotherapy with Fosicard does not bring a positive effect, then adding a diuretic .
When starting to take this drug along with a diuretic , an initial dose of up to 10 mg is prescribed, with careful medical monitoring of the patient’s condition.
During the treatment of chronic heart failure, an initial daily dose of 10 mg is set. Gradually increase the dose by 10 mg weekly. In this case, the maximum dosage should not be higher than 40 mg/day. It is also possible to additionally take a diuretic .
Special instructions for the use of the drug Fosicard
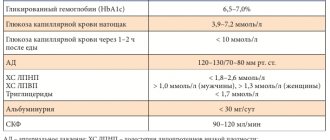
Treatment with fosinopril should not be initiated in patients with acute myocardial infarction who are at risk of further severe hemodynamic deterioration after use of vasodilators. These are patients with systolic blood pressure ≤100 mm Hg. Art. or patients with cardiogenic shock. During the first 3 days after myocardial infarction, the dose should be reduced if systolic blood pressure is ≤120 mmHg. Art. The maintenance dose should be reduced to 5–2.5 mg if systolic blood pressure ≤100 mm Hg. Art. For persistent hypotension (systolic blood pressure ≤90 mm Hg), fosinopril should be discontinued. During treatment with fosinopril in combination with diuretics in patients without signs of renal vascular disease, there may be a slight increase in serum urea and serum creatinine. This effect, however, is more often noted in patients with pre-existing renal failure. A dose reduction of fosinopril may be necessary. Regular monitoring of potassium and creatinine levels is part of standard medical monitoring in these patients. In patients with heart failure, hypotension at the start of treatment with ACE inhibitors may lead to additional impairment of renal function. In such cases, acute renal failure may develop, usually reversible. In acute myocardial infarction, treatment with fosinopril should not be started in patients with diagnosed renal dysfunction, with a serum creatinine concentration of 177 µmol/l and/or proteinuria exceeding 500 mg/24 hours. If renal dysfunction develops during treatment with fosinopril (serum creatinine concentration of 265 µmol/ l or if serum creatinine levels are 2 times higher than before treatment), the doctor should consider discontinuing treatment with fosinopril. There is evidence of anaphylactic reactions in patients receiving ACE inhibitors during hemodialysis using high-permeability membranes. In such cases, the possibility of using a different type of dialysis membrane or the use of antihypertensive drugs of a different group should be considered. There is evidence of the appearance of cough after the use of ACE inhibitors. Usually the cough is non-productive, persistent and stops after discontinuation of the drug. During the first month of treatment with an ACE inhibitor, strict monitoring of blood glucose levels is necessary in patients taking oral antidiabetic agents or insulin. During pregnancy and breastfeeding. It is not known whether fosinopril passes into breast milk. The use of fosinopril during pregnancy and breastfeeding is not recommended. Ability to drive vehicles and operate machinery. Fosinopril has no or negligible effect on the ability to drive vehicles or operate machinery. Drivers should be aware that dizziness or fatigue may sometimes occur.
Interaction
Simultaneous use of the drug with antihypertensive drugs, diuretics, narcotic analgesics, and general anesthesia can enhance the hypotensive effect of fosinopril.
Combination with potassium supplements and some potassium-sparing diuretics increases the likelihood of developing hyperkalemia . Simultaneous use with lithium salts increases the concentration of lithium in the blood.
Fosicard increases the hypoglycemic effect of sulfonylurea derivatives, insulin, the risk of leukopenia increases in cases of simultaneous use with allopurinol , immunosuppressants, cytostatic drugs, procainamide . Combination with NSAIDs and estrogens reduces the severity of the hypotensive effect.
special instructions
Treatment with Fosicard for patients suffering from severe arterial hypertension or decompensated chronic heart failure is recommended to begin in the hospital. In this case, the therapeutic process requires monitoring of blood pressure, kidney function, hemoglobin, urea and creatinine , concentrations of electrolytes and potassium, and the activity of liver enzymes in the blood.
It is also necessary to periodically monitor the number of leukocytes , especially if there is a risk of neutropenia , for example, in cases of impaired renal function or systemic connective tissue diseases.
A possible increase in the development of arterial hypotension requires caution when the drug is prescribed to patients who are on a salt-free or low-salt diet.
Taking this drug may cause dizziness, usually at the beginning of treatment when combined with diuretics , so caution should be used in activities requiring special attention or when driving.
Fosicard
Before starting treatment, it is necessary to analyze previous antihypertensive therapy, the degree of increase in blood pressure, dietary restrictions on salt and/or liquid, and other clinical circumstances.
Patients with severe arterial hypertension or concomitant decompensated CHF should begin treatment with Fosicard in a hospital setting.
Before and during treatment with the drug, it is necessary to monitor blood pressure, kidney function, potassium content, hemoglobin, creatinine, urea, electrolyte concentrations and the activity of “liver” transaminases in the blood.
Angioedema
The development of angioedema has been reported in patients using the drug Fosicard. Swelling of the tongue, pharynx, or larynx can cause airway obstruction, which can be fatal. If such reactions develop, patients must stop taking the drug and subcutaneously administer a solution of epinephrine (adrenaline) (1:1000), as well as take other emergency treatment measures.
There is a risk of anaphylactic reactions during desensitization with hymenoptera venom while taking an ACE inhibitor. The simultaneous use of APS inhibitors with the combination of valsartan + sacubitril is contraindicated due to the increased risk of angioedema. Taking Fosicard should not be started before 36 hours after taking the last dose of this combination, just as taking the combination of valsartan + sacubitril should not be started before 36 hours after taking the last dose of Fosicard.
Concomitant use of ACE inhibitors with racecadotril, mTOR inhibitors (such as sirolimus, everolimus, temsirolimus) and vildagliptin may lead to an increased risk of developing angioedema (see section "Interaction with other drugs").
Swelling of the intestinal mucosa
Swelling of the intestinal mucosa has rarely been observed while taking ACE inhibitors. These patients complained of abdominal pain (there may have been no nausea and vomiting), in some cases swelling of the intestinal mucosa occurred without swelling of the face, and the level of C1-esterases was normal. Symptoms disappeared after stopping the use of ACE inhibitors. Edema of the intestinal mucosa should be included in the differential diagnosis of patients taking ACE inhibitors who complain of abdominal pain.
Anaphylactic reactions during dialysis using high-permeability membranes Anaphylactic reactions may develop in patients who used ACE inhibitors during hemodialysis through high-permeability membranes, as well as during apheresis of low-density lipoproteins with adsorption to dextran sulfate. In these cases, the use of a different type of dialysis membrane or other antihypertensive therapy should be considered.
Neutropenia/agranulocytosis
It is possible to develop agranulocytosis and suppression of bone marrow function during treatment with ACE inhibitors. These cases occur more often in patients with impaired renal function, especially in the presence of systemic connective tissue diseases (systemic lupus erythematosus or scleroderma). Before starting therapy with ACE inhibitors and during treatment, the total number of leukocytes and the leukocyte formula are determined (once a month in the first 3-6 months of treatment and in the first year of use of the drug in patients with an increased risk of neutropenia).
Arterial hypotension
In patients with uncomplicated arterial hypertension, arterial hypotension may develop due to the use of the drug Fosicard.
Symptomatic hypotension with the use of ACE inhibitors most often develops in patients after intensive treatment with diuretics, a diet limiting salt intake, or during renal dialysis. Transient arterial hypotension is not a contraindication for the use of the drug after measures to restore blood volume.
In patients with CHF, treatment with ACE inhibitors may cause excessive antihypertensive effects, which can lead to oliguria or azotemia, which can be fatal. Therefore, when treating CHF with Fosicard, it is necessary to carefully monitor patients, especially during the first 2 weeks of treatment, as well as with any increase in the dose of Fosicard or a diuretic.
A reduction in the diuretic dose may be required in patients with hyponatremia and in patients previously intensively treated with diuretics. Arterial hypotension is not a contraindication for further use of the drug Fosicard. Some reduction in systemic blood pressure is a common and desirable effect when starting the drug for heart failure. The extent of this reduction is greatest early in treatment and stabilizes within one or two weeks of starting treatment. Blood pressure usually returns to pre-treatment values without a decrease in therapeutic efficacy.
Liver dysfunction
If noticeable jaundice appears and a marked increase in the activity of liver enzymes, Fosicard should be discontinued and appropriate treatment should be prescribed.
In rare cases, when using ACE inhibitors, a syndrome is observed, the first manifestation of which is cholestatic jaundice. This is followed by fulminant liver necrosis, sometimes fatal. The mechanism of development of this syndrome has not been studied.
In patients with impaired liver function, increased plasma concentrations of fosinopril may be observed. In liver cirrhosis (including alcoholic cirrhosis), the apparent total clearance of fosinopril is reduced, and the AUC is approximately 2 times higher than in patients without liver dysfunction.
Renal dysfunction
In patients with arterial hypertension with bilateral renal artery stenosis or stenosis of the artery of a single kidney, as well as with simultaneous use of diuretics without signs of renal impairment, the concentration of blood urea nitrogen and serum creatinine may increase during treatment with ACE inhibitors. These effects are usually reversible and disappear after treatment is stopped. It may be necessary to reduce the dose of the diuretic and/or Fosicard.
In patients with severe CHF, with altered activity of the renin-angiotensin-aldosterone system, treatment with ACE inhibitors can lead to oliguria, progressive azotemia and, in rare cases, acute renal failure and possible death.
Hyperkalemia
Increases in serum potassium levels have been observed in some patients receiving ACE inhibitor therapy, including fosinopril. Patients at increased risk of developing hyperkalemia include: patients with impaired renal function or diabetes mellitus, patients taking potassium-sparing diuretics, potassium supplements or potassium-containing salt substitutes, and patients taking other drugs that may increase serum potassium levels (eg heparin, trimethoprim or co-trimoxazole, also known as a combination of trimethoprim and sulfamethoxazole) and especially aldosterone antagonists or angiotensin receptor blockers. If the simultaneous use of these drugs is considered necessary, it is recommended to periodically monitor the level of potassium in the blood serum (see section "Interaction with other drugs").
Cough
When using ACE inhibitors, including fosinopril, some patients may experience a nonproductive, persistent cough that resolves after discontinuation of therapy. When cough occurs in patients taking ACE inhibitors, this therapy should be considered as a possible cause in the differential diagnosis.
Surgery/general anesthesia
ACE inhibitors may enhance the antihypertensive effect of drugs used for general anesthesia. Before surgery (including dentistry), the surgeon/anesthesiologist must be warned about the use of ACE inhibitors.
Special patient groups
Fosinopril (like other ACE inhibitors) has a less pronounced antihypertensive effect and has a higher risk of developing angioedema in black patients compared to representatives of other races.
There is no experience with the use of fosinopril in patients who have recently undergone kidney transplantation.
The drug should be used with caution in patients with obstruction of the blood outflow tract from the left ventricle (aortic or mitral stenosis/hypertrophic obstructive cardiomyopathy).
Caution should be exercised when performing work requiring increased attention, as dizziness may occur, especially after the initial dose of an ACE inhibitor in patients taking diuretics. Caution should be exercised when performing physical exercise or in hot weather due to the risk of dehydration and hypotension due to a decrease in blood volume.
The safety and effectiveness of Fosicard in children has not been established.
Fozikard's analogues
Level 4 ATC code matches:
Dilaprel
Prenesa
Enap
Diroton
Lipril
Renipril
Parnavel
Fozinap
Tritace
Enam
Zokardis
Fosinopril
Lisinopril
Captopril
Monopril
Renitek
Hartil
Amprilan
Ramipril
Perindopril
The main analogues are represented by the drugs Monopril, Fozinotec and Fosicard N. Also have a similar effect: Enalapril, Prestarium , Captopril and Lisinopril.
Possibilities of using the ACE inhibitor fosinopril (Fosicard) in cardiology
Angiotensin-converting enzyme inhibitors (ACE inhibitors) are one of the most commonly used groups of drugs in modern clinical practice. Over the twenty-five years that have passed since the creation of the first ACE inhibitor drugs, the number of indications for their use has constantly increased. Initially, they were intended for the correction of arterial hypertension, then for the treatment of chronic heart failure and a number of manifestations of coronary heart disease. Today, these drugs are considered in a broader therapeutic aspect - as effective means of combating cardiovascular morbidity and mortality. According to a number of large-scale placebo-controlled studies (SOLVD, SAVE, CAPPP, ELIT), it has become obvious that long-term use of ACE inhibitors significantly reduces the risk of both non-fatal and fatal cardiovascular accidents. However, much less attention is paid to the fact that in a number of studies, with long-term use of ACE inhibitors, there was a decrease in mortality not only from cardiovascular pathology, but also in overall mortality, that is, mortality from non-cardiac causes. As is known, in most socio-economically developed countries where these studies were carried out, such causes are tumor diseases and diabetes mellitus. The close relationship between metabolic disorders and cardiovascular diseases is beyond doubt. In patients with arterial hypertension, disorders of carbohydrate metabolism (impaired glucose tolerance, type 2 diabetes mellitus), lipid profile (hypertriglyceridemia, decreased HDL cholesterol, increased LDL cholesterol), fat metabolism (abdominal obesity), hyperuricemia, changes in the fibrinolysis system are often detected. Currently, this symptom complex is combined into a cluster of risk factors and is included in the concept of “metabolic syndrome”. It has been established that ACEIs combine a number of advantages: hypotensive activity, low incidence of side effects, proven cardio-, vaso- and nephroprotective effects, improved quality of life for patients, and reduced incidence of cardiovascular complications. During therapy with ACE inhibitors, there are no adverse changes in carbohydrate, lipid metabolism, or uric acid levels. The beneficial effect on insulin resistance and some indicators of hemostasis (decrease in the level of tissue plasminogen activator inhibitor, increase in tissue plasminogen activator) are debated. The group of angiotensin-converting enzyme inhibitors is quite numerous. These drugs differ from each other in: – chemical structure (presence or absence of a sulfhydryl group), – features of drug excretion from the body (by the kidneys or kidneys and liver), – duration of action, – tissue specificity, – features of metabolism. Based on their chemical composition, ACE inhibitors are classified as containing a sulfhydryl group (captopril), a carboxyl group (enalapril, ramipril, lisinopril, etc.) and a phosphonyl group (fosinopril). However, this classification has no practical significance, since it has been established that the physicochemical and clinical pharmacological properties of a particular drug are important, and not which radical interacts with the active center of ACE. Currently, one of the most common classifications of ACE inhibitors is based on dividing them into lipophilic and hydrophilic drugs, taking into account the characteristics of their metabolism. The systemic bioavailability of lipophilic ACE inhibitors is generally higher than that of hydrophilic drugs. It has been established that the amount of lipophilicity of ACE inhibitors directly correlates with the strength of tissue ACE inhibitor inhibition, which should provide the drugs with advantages in long-term blood pressure control and target organ protection. However, there is no evidence in favor of this assumption; for example, no significant differences were found in the clinical effectiveness of the lipophilic ACE inhibitor enalapril and the hydrophilic drug lisinopril in patients with arterial hypertension. Differences in the bioavailability of individual drugs are also of minor clinical significance. More significant is their interaction with food. Of all the ACE inhibitors, only captopril and moexipril have this property, since the proportion of their absorption after a meal is halved, which creates the need to use them an hour before or an hour after a meal. The main route of elimination of all known active ACE inhibitors and active metabolites of most inactive drugs is renal excretion. The excretion of drugs by the kidneys from the body depends on the intensity of glomerular filtration processes, which are assessed by the value of creatinine clearance. Renal blood flow under the influence of ACE inhibitors either does not change or is slightly increased, while the glomerular filtration rate may decrease, which is of important clinical significance in patients with renal failure. Treatment of such patients should begin with lower doses of ACE inhibitors, gradually increasing the dose to an effective one, since the nephroprotective effect of these drugs increases with its increase. Among ACE inhibitors, there are several drugs whose active metabolites are excreted not only by the kidneys, but also with bile and feces. It is clear that with long-term use, these ACE inhibitors are safer than drugs with predominantly renal elimination. For example, the active metabolite of fosinopril, fosinoprilat, is eliminated both through the kidneys and the liver. Normally, renal and hepatic excretion of fosinopril occurs to an equal extent. With nephropathy, the proportion of hepatic elimination increases, which prevents the accumulation of the drug. In patients with nephropathy, the accumulation index of fosinopril is three times less than that of enalapril, and six times less than that of lisinopril. The presence of a large number of ACE inhibitors poses a difficult task for clinicians in choosing a specific drug for a specific patient. The question arises to what extent the above-mentioned differences between various ACEIs affect their clinical effectiveness, and whether these differences should determine the choice of a particular drug by a practitioner. Since the main effect of ACE inhibitors is their ability to improve the prognosis of diseases, it is fundamentally important whether this ability is inherent to all drugs in this group to the same extent. Currently, only two ACE inhibitors (captopril and lisinopril) that directly possess biological activity are registered in Russia. Other known ACE inhibitors are inactive substances or prodrugs. They are converted into active metabolites only after absorption in the gastrointestinal tract as a result of hydrolysis and esterification during the first passage through the liver, for example, enalapril - into enalaprilat, perindopril - into perindoprilat, fosinopril - into fosinoprilat. Let's consider the currently available evidence base regarding one of the ACE inhibitors - fosinopril. Fosinopril (Fosicard, pharmaceutical company Actavis, Iceland) is one of the representatives of the latest (third) generation of ACE inhibitors. Fosicard is the first generic analogue of fosinopril, meets modern pharmacotherapy requirements and is available to a wide range of patients. Fosinopril (Fosicard) contains phosphonyl acid in its chemical formula, is a prodrug and acts after absorption and transformation into an active metabolite - fosinoprilat, which circulates in a state bound to blood plasma proteins (95-98%) with a half-life of about twelve hours. Fosinopil is transformed into an active metabolite not only in the liver, but also in the mucous membrane of the gastrointestinal tract. Due to the significant participation of extrahepatic pathways in metabolic transformation, the pharmacokinetics of fosinopril depend to a much lesser extent on the condition of the liver, which is manifested in the clinic by the stability of effects even when taking the first dose of the drug, regardless of the patient’s age and concomitant diseases of the gastrointestinal tract. The main advantage of fosinopril is its balanced dual route of elimination from the body - renal excretion in the urine and hepatic degradation of active metabolites, followed by their removal in bile through the gastrointestinal tract. The participation of both pathways in the elimination of fosinoprilat is approximately the same, and they mutually compensate for each other. Fosinoprilat has a high lipophilicity, which facilitates the penetration of the drug through cell membranes into many organs (heart, kidneys, blood vessels, lungs, adrenal glands) and can effectively suppress the activity of not only the circulating, but also the tissue renin-angiotensin-aldosterone system. The unique quality of fosinopril, which distinguishes it from other ACE inhibitors, is its good tolerability. According to placebo-controlled studies, in patients with chronic heart failure of functional class II–IV according to the NYHA classification, the frequency of side effects when using fosinopril and placebo was practically no different. In addition, when using fosinopril, an extremely low incidence of dry cough was noted. It has been proven that dry cough caused by other ACE inhibitors decreases or completely disappears when switching to fisinopril. In addition, its use is associated with fewer clinical and biochemical side effects, especially in elderly patients or patients with diabetes mellitus. Fosinopril (Fosicard) is easy to use and combines well with diuretics (potentiates the effect). A single dose of the drug provides 24-hour control over blood pressure levels. Fosinopril is a drug whose dose does not need to be changed in elderly patients [LH Opie, 1999]. In elderly patients (65–75 years) with clinically unchanged liver and kidney function, no difference in the pharmacokinetics of fosinoprilat was observed compared with young patients (20–35 years), therefore the initial dose of fosinopril in all patients is 10 mg/day. once. The FACET study compared the clinical efficacy, biochemical effects, and endpoints of fosinopril and the calcium antagonist amlodipine in patients with hypertension and non-insulin-dependent diabetes mellitus. During three years of follow-up, significantly fewer deaths, myocardial infarctions, and strokes were observed in the fosinopril group than during amlodipine therapy (14% versus 27%, respectively). The FOPS (Fosinopril in Old Patients Study) study involved more than seven hundred patients over 60 years of age with arterial hypertension, and the follow-up period was twelve weeks. The target blood pressure level was achieved in 80% of patients. The effectiveness of the drug did not depend on the degree of renal dysfunction. The incidence of side effects was 6.4%. The antihypertensive effect of fosinopril has been studied in many clinical studies (FISH, FLIGHT), where the drug also proved high antihypertensive activity and good tolerability. As part of the Russian program to assess the practical achievability of target blood pressure levels, a study of fosinopril in the treatment of arterial hypertension (FLAG) was conducted. At the end of the study, normalization of blood pressure was noted in 62.1% of patients, and treatment was effective (normalization of blood pressure and a decrease in blood pressure by more than 10% from baseline) in 88.8% of patients. Adverse reactions were noted in 8.3% of patients, with almost the same frequency in patients taking both 10 mg and 20 mg of fosinopril. Of particular interest is the FAMIS study, in which fosinopril was used in patients who had suffered an acute myocardial infarction and had no evidence of left ventricular dysfunction (EF>45%). Even in the group of patients at the lowest risk, fosinopril was effective and significantly reduced the risk of death and the development of severe chronic heart failure by 36.2%. The single-center, double-blind, placebo-controlled PREVEND IT trial was conducted to evaluate the ability of fosinopril and pravastatin to reduce cardiovascular deaths and cardiovascular hospitalizations in individuals with microalbuminuria. According to the results of this study, the use of fosinopril was accompanied by a significant decrease in both systolic and diastolic blood pressure, no changes in the main parameters of the lipid profile, and a rapid decrease in urinary albumin excretion. R. Fogari et al. (2002) showed a significant decrease in the level of albuminuria when fosinopril was prescribed in patients with diabetes mellitus, as well as a decrease in urinary excretion of one of the markers of endothelial dysfunction - the vascular adhesion molecule VCAM-1. A safety study of fosinopril that included more than 2,000 patients with hypertension and heart failure over a one-year follow-up found that overall adverse reactions were mild and transient, and their incidence was not related to the recommended daily dose. The most common symptoms (0.4–0.9%) were headache, nausea, vomiting, diarrhea, cough, weakness, and increased transaminases. In elderly patients, there were no differences in the incidence of adverse reactions when taking fosinopril compared with young patients. Only in the last few years have the results of studies appeared, the purpose of which was the pharmacoeconomic optimization of therapy for patients with arterial hypertension. The complexity of pharmacoeconomic analysis when assessing the effectiveness of various antihypertensive drugs is associated with the lack of a unit for measuring their effectiveness; therefore, the most reliable are cost-effectiveness calculations based on the results of large comparative randomized studies. During the FAGOT program (Pharmacoeconomic assessment of the use of ACE inhibitors in the outpatient treatment of patients with Complicated Arterial Hypertension), it was proven that fosinopril has better price characteristics (in terms of the cost of achieving the target blood pressure level) compared to other antihypertensive therapy regimens. When assessing pharmacoeconomics, it was shown that the use of fosinopril is the most cost-effective and affordable way to adequately improve the quality of life of patients with cardiovascular diseases. The study “Pharmacoeconomic assessment of the use of ACE inhibitors in the outpatient treatment of patients with heart failure (FASON),” which included about two thousand patients with chronic heart failure class II–III, proved the high effectiveness and safety of treatment of chronic heart failure with fosinopril. There was a significant improvement in clinical status (by 53%), while treatment costs were reduced by more than 50%. Thus, knowledge of the differences between individual ACE inhibitors, as well as their clinical, economic and social effectiveness, allows not only to select an effective drug that improves the prognosis of the disease and the patient’s quality of life, but also contributes to the rational use of resources allocated to healthcare. Currently, ACE inhibitors, including fosinopril (Fosicard), are increasingly used in clinical practice, while fosinopril (Fosicard) has a number of advantageous characteristics that distinguish it from other representatives of this class of drugs. ACE inhibitors are not only effective antihypertensive drugs, but also reduce cardiovascular morbidity and mortality in patients with arterial hypertension. Important additional characteristics of ACE inhibitors are good tolerability, organoprotective properties, and the effects are fully inherent in fosinopril (Fosicard). Thus, with the help of fosinopril (Fosicard), one of the most effective and safe representatives of the class of ACE inhibitors, it is possible not only to successfully treat patients with arterial hypertension and chronic heart failure (elderly, with diabetes mellitus, impaired renal function), but also to prevent the development cardiovascular complications, including chronic heart failure, in patients with multiple risk factors. Literature 1. Branko V.V., Proshin A.Yu. The use of angiotensin-converting enzyme in clinical practice (a view from the perspective of clinical pharmacology) Gedeon Richter in the CIS. – 2000. – No. 1. – P. 15–19. 2. Karpov Yu.A., Mareev V.Yu., Chazova I.E. Heart failure. “Russian programs for assessing the effectiveness of fosinopril treatment in patients with arterial hypertension and heart failure. Project TRI F (FLAG, FASON, FAGOT)", September, volume 4, no. 5, 2003. 3. Karpov Yu.A. Treatment of arterial hypertension: choice of the first drug. Russian medical journal. – 2001, No. 10, p. 396–400. 4. Kobalava Zh.D. New views on arterial hypertension. Proceedings of the Russian scientific forum with international participation “Cardiology 2000”, January 26–29. – pp. 144–154. 5. Stryuk R.I., Petrova T.V., Orlova T.A., Nagornev S.N. The clinical effectiveness of phosinopril in patients with hypertension in combination with metabolic disorders. Cardiology. - 1999. - No. 7. - S. 13–16. 6. FURBERG CD, Pitt V. ALL ALL ALL ALLL ANGIOTENSINGENERTING ENZYME Inhibitors Interchangeable? J.AMER.COLL.CARDIOL. 2001; 37: 1456–1460. 7. Hansson L., Lindholm LH, Niskanen L., Hedner J., Niklacon A., Luomanmaki K., Dahlof V., Defaire U., Morlin C, Karlberg V., Wester Po, Bjork J. - T. Effect of angiotensin - consyme inhibition compared with confidental Therapy on Cardiovascular Morbidity in Hypertension: The Captopril Prevention Provent (CAPPP) LANCET. – 1999. –Vol. 353.- No. No. 9153. - P. 611–616. 8. Houston M., Asher Jr, Naftilan Aj Hypertension Institute Clinical Review: Allhat Not It ”S Cracked Up To be: Review of the Facts and the Science J. amer. Nutraceutic. Association 2003; 6: L - 4. 9. World Health Organization - International Society of Hypertension Guidelines for the Management of Hypertension J. Hypertension. - 1999. Vol. 17. –P. 151–183.
Reviews about Fosicard
This drug is usually prescribed for hypertension , but it should be understood that such treatment does not bring complete recovery. At the same time, reviews of Physicard show that complex therapy with this drug is carried out for patients who have been bothered by this disease for several years.
According to experts, treating hypertension requires the right approach and perseverance. Therefore, patients must comply with the doctor’s prescriptions without violating the therapeutic regimen and without stopping treatment on their own. In addition to taking medications, it is necessary to adhere to a healthy lifestyle and perform procedures that will strengthen blood vessels.
Overdose of the drug Fosicard, symptoms and treatment
When using doses significantly higher than recommended, severe arterial hypotension, circulatory shock, stupor, bradycardia, electrolyte disturbances and renal failure may develop. Treatment is carried out by gastric lavage (within 30 minutes after taking the drug) and accelerating elimination. Treatment with angiotensin II should be considered. Bradycardia and pronounced vagal reactions can be relieved by administering atropine. If necessary, the use of a temporary pacemaker should be considered.
Phosicard price, where to buy
The price of Fosicard varies between 107-237 rubles and depends on the content of the active substance in the tablets.
- Online pharmacies in RussiaRussia
- Online pharmacies in UkraineUkraine
- Online pharmacies in KazakhstanKazakhstan
ZdravCity
- Phosicard tablets 5 mg 28 pcs. Zdravle JSC HFZ
194 rub. order - Phosicard tablets 10 mg 28 pcs. Zdravle JSC HFZ
RUB 328 order
- Phosicard tablets 20 mg 28 pcs. Zdravle JSC HFZ
RUB 357 order
Pharmacy Dialogue
- Fosicard N (tab. 20/12.5 mg No. 28) Actavis
RUR 442 order
- Phosicard (tab. 10 mg No. 28)Zdravlje
RUR 318 order
- Phosicard (tab. 20 mg No. 28) Actavis
RUB 342 order
- Phosicard (tab. 5 mg No. 28)Zdravlje
210 rub. order
show more
Pharmacy24
- Phosicard 20 mg No. 30 tablets Actavis AT.Islandiya/Pharmac.i Chemical Industry, Zdravle AT, Serbia/Balkanfarma-Dupnitsa AT, Bulgaria
204 UAH.order - Phosicard 10 mg No. 30 tablets Actavis AT.Icelandia/Pharmaceutical and Chemical Industry, Zdravle AT, Serbia
158 UAH order
PaniPharmacy
- Fosicard H tablets Fosicard N tablets. 20/12.5 mg No. 30 Iceland, Actavis
174 UAH order
- Phosicard tablets Phosicard tablets. 20 mg No. 30 Serbia, Zdravlje
205 UAH order
- Phosicard tablets Phosicard tablets. 10mg No. 30 Serbia, Zdravlje
152 UAH order
show more