Preparations of adrenal hormones (corticosteroids) are drugs that are similar in structure and function to the hormones of the adrenal cortex - glucocorticoids and mineralocorticoids.
Like all hormones, corticosteroids have a significant effect on the functioning of the body. Thus, glucocorticoids - hydrocortisone (cortisol) and cortisone - affect all types of metabolism: protein, fat and carbohydrate.
Capable of penetrating into the nuclei of the body's cells and there stimulating or suppressing the synthesis of various enzymes, antibodies, mediators and transport proteins, glucocorticoids affect immune, allergic and inflammatory processes in the body.
Mineralocorticoids (aldosterone) affect water-salt metabolism.
Indications for use
Glucocorticoid preparations are indicated for severe allergic reactions - anaphylactic shock, angioedema (Quincke's edema), bronchial asthma, status asthmaticus, serum sickness, atopic and contact dermatitis.
Glucocorticoids are also prescribed for autoimmune diseases that affect connective tissue (collagenosis): systemic lupus erythematosus, rheumatoid arthritis; skin diseases: psoriasis, seborrheic and exfoliative dermatitis, neurodermatitis.
Glucocorticoids are also used for shocks (sharp drop in blood pressure) of various origins: traumatic, anaphylactic, cardiogenic, toxic, burn.
Glucocorticoids are indicated for severe acute and chronic diseases of the respiratory system (pneumosclerosis), gastrointestinal tract (ulcerative colitis, Crohn's disease, acute pancreatitis, toxic and autoimmune hepatitis, cirrhosis of the liver), kidneys (glomerulonephritis), blood system (leukemia, agranulocytosis, aplastic anemia), eyes (conjunctivitis, keratitis, iritis, iridocyclitis).
Glucocorticoids are used for traumatic brain injury, pulmonary edema, and cerebral edema.
Glucocorticoids are also indicated for the prevention of graft rejection during organ and tissue transplantation.
Glucocorticoid preparations are also prescribed for various poisonings.
In addition, glucocorticoids are used in the complex treatment of malignant tumors.
Mineralocorticoid preparations are used for Addison's disease - acute and chronic insufficiency of the adrenal cortex, when the production of its own mineralocorticoids is reduced.
Corticosteroids for Covid
Impact of COVID-19 on the immune system
Covid-19 is a biphasic disease with the innate immune response evolving into a broadly effective adaptive immune response, except in the minority of people who develop severe disease. Corticosteroids, such as dexamethasone, have broad effects on innate and adaptive immunity. Adaptive immunity may be an integral part of the immunopathology of covid-19, as the occurrence of acute respiratory distress syndrome is temporally correlated with the emergence of specific antibodies against SARS-CoV-2.
Patients with severe COVID-19 may develop a systemic inflammatory response that can lead to lung damage and multiple organ dysfunction. The anti-inflammatory effects of corticosteroids may prevent or mitigate these harmful effects.
Difference between COVID-19 and other coronavirus infections
The pathogenesis of SARS-CoV-2 is fundamentally different from that of its predecessors SARS-CoV-1 and MERS, whose poor outcomes are correlated with viremia and high viral load in the lungs at the time of death. Unlike the MERS coronavirus, SARS-CoV-2 is rarely detected in the blood during the symptomatic phase of covid-19, even in people with severe illness. In addition, hypoxemia may develop when the viral load in the upper respiratory tract falls rapidly or becomes undetectable. Patients hospitalized with covid-19 typically report the onset of symptoms 3-5 days after infection (fatigue, chills), progressing to fever and dry cough after 48 hours. Progression to a severe condition with hypoxemia occurs five to seven days after the onset of symptomatic illness, approximately 8 to 14 days after initial infection. In the RECOVERY trial, dexamethasone was beneficial in participants treated for seven or more days after the onset of the symptomatic phase with the onset of hypoxemia . Thus, the RECOVERY data support the use of dexamethasone only in patients with hypoxemia and not in patients with milder disease. Data do not support the use of dexamethasone or other corticosteroids in the outpatient setting.
Dexamethosone for Covid
Corticosteroids, such as hydrocortisone and dexamethasone, have anti-inflammatory, antifibrotic, and vasoconstrictor effects that critical care practitioners have been trying to use for decades to improve the condition of patients with acute respiratory distress syndrome and septic shock. While early observational data from China suggested a potential increased mortality of corticosteroids in COVID-19, previous studies of corticosteroids in other viral pneumonias, particularly severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS), found an association with delayed viral clearance and increased concerns that corticosteroids may worsen the host response to SARS-CoV-2
The Randomized Evaluation of COVID-19 Therapy (RECOVERY), a multicenter, randomized, open-label trial in hospitalized patients with COVID-19, found that mortality from COVID-19 was lower among patients who were randomized to receive dexamethasone than among those who received standard care. help. The US Centers for Disease Prevention and Control (CDC) guidelines recommend against corticosteroid therapy for coronavirus infections because steroids "prolong viral replication" in patients with MER, although the difference in time to viral clearance was not statistically significant in the primary data.
Good or bad?
Both beneficial and harmful clinical outcomes have been reported with the use of corticosteroids (mostly prednisone or methylprednisolone) in patients with other pulmonary infections. In patients with pneumonia and hypoxia caused by Pneumocystis jirovecii, prednisone therapy reduces the risk of death; however, in outbreaks of other novel coronavirus infections (eg, Middle East respiratory syndrome—MERS and severe acute respiratory syndrome—SARS), corticosteroid therapy has been associated with delayed viral clearance. For severe pneumonia caused by influenza viruses, corticosteroid therapy is associated with worse clinical outcomes, including secondary bacterial infection and death.
A meta-analysis of trials in stress respiratory syndrome found that, compared with placebo, corticosteroid therapy reduced the risk of all-cause mortality. No benefit from dexamethasone was observed in patients who did not require supplemental oxygen at enrollment.
Corticosteroids other than dexamethosone
If dexamethasone is not available, alternative glucocorticoids such as prednisone, methylprednisolone, or hydrocortisone can be used. For these drugs, the total daily equivalent doses of dexamethasone 6 mg (oral or intravenous) are: prednisone - 40 mg, methylprednisolone - 32 mg, hydrocortisone - 160 mg. Hydrocortisone is commonly used to treat septic shock in patients with COVID-19; Unlike other corticosteroids previously studied in patients with acute respiratory distress syndrome, dexamethasone does not have mineralocorticoid activity and thus has minimal effects on sodium balance and fluid volume.
Side effects of dexamethosone
Clinicians should closely monitor COVID-19 patients receiving dexamethasone for adverse effects (eg, hyperglycemia, secondary infections, psychiatric disorders, avascular necrosis). Long-term use of systemic corticosteroids may increase the risk of reactivation of latent infections (eg, hepatitis B virus, herpesvirus infections, strongyloidiasis, tuberculosis). The risk of reactivation of latent infections with a 10-day course of dexamethasone (6 mg once daily) has not been clearly established. When initiating dexamethasone, appropriate screening and treatment should be undertaken to reduce the risk of Strongyloides hyperinfection in patients at high risk of strongyloidiasis.
Interaction of dexamethosone with other drugs
Dexamethasone is a moderate inducer of cytochrome P450 (CYP) 3A4. Therefore, it may decrease the concentrations and potential effectiveness of concomitant medications that are CYP3A4 substrates. Clinicians should review a patient's medication regimen to evaluate possible interactions. The combined use of remdesivir and dexamethasone has not been formally studied, but a clinically significant pharmacokinetic interaction is not predicted.
The half-life, duration of action, and frequency of dosing vary among corticosteroids.
Long-acting corticosteroid: dexamethasone; Half-life: 36 to 72 hours, apply once daily. Intermediate-acting corticosteroids: prednisone and methylprednisolone; Half-life: 12 to 36 hours, apply once daily or in two divided doses daily. Short-acting corticosteroid: hydrocortisone; Half-life: 8 to 12 hours, administered in two to four divided doses daily.
Dexamethosone during pregnancy
Short courses of betamethasone and dexamethasone, which are known to cross the placenta, are commonly used to reduce neonatal complications of prematurity in women at risk of preterm labor.
Dexamethosone in children
Dexamethasone may be useful for pediatric patients with COVID-19 respiratory disease who require mechanical ventilation. The use of dexamethasone in patients who require other forms of supplemental oxygen support should be considered on an individual basis and is generally not recommended for pediatric patients who require only low levels of oxygen support (eg, nasal cannula only).
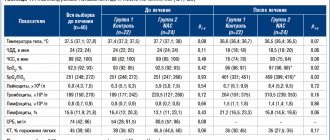
Initial severity of Covid and effectiveness of dexamethosone
The survival benefit was greatest among patients who required invasive mechanical ventilation at randomization: 29.3% of participants in the dexamethasone group died within 28 days compared with 41.4% in the standard care group. Among patients who required supplemental oxygen but not mechanical ventilation at enrollment, 23.3% of those in the dexamethasone group and 26.2% of those in the standard care group died within 28 days. There was no survival benefit observed among participants who did not require oxygen therapy on admission; 17.8% of patients in the dexamethasone group and 14.0% in the standard care group died within 28 days.
Extended course of corticosteroids
At present, an extended course of corticosteroids beyond 10 days is considered only in selected cases of severe COVID-19.3 One argument for long-term treatment is the prevention of fibrosis after illness in patients with COVID-19 for whom risk factors for pulmonary fibrosis may be established. However, with COVID-19, such a long course of corticosteroids may inadvertently lead to poor treatment outcomes. The possible influence of steroids in the procoagulant environment of COVID-19 patients should be considered, where even anticoagulant therapy does not sufficiently protect against the thrombotic complications found in deceased patients. A hypercoagulable state with profound endothelial damage following severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection plays an important role in the development of thrombosis. In autopsy studies of patients with COVID-19, diffuse alveolar abnormalities with large vessel thrombi and microthrombi have been seen. Dexamethasone (6 mg daily) tends to increase clotting factor and fibrinogen concentrations. In addition, long-term corticosteroid therapy may contribute to the so-called long COVID syndrome, which is characterized by fatigue and psychological symptoms in which steroid-related adverse drug reactions such as myopathy, neuromuscular weakness, and psychiatric symptoms may occur. Initiating methylprednisolone therapy more than 2 weeks after the onset of acute respiratory distress syndrome may increase the risk of death. The prothrombotic effects of steroids combined with their adverse drug reactions may have contributed to the increased mortality.
Corticosteroids therefore appear to be a double-edged sword in the fight against COVID-19 and should be used judiciously, taking into account the risk-benefit ratio, as a short-term (eg, up to 10 days) therapeutic agent in a select group. patients with COVID-19 who have demonstrated improved survival. There is no evidence to support the long-term use of steroids in patients with COVID-19 to prevent potential adverse effects such as pulmonary fibrosis. On the contrary, such a long course of steroids could be harmful.
Glucocorticoids as a cause of diabetes mellitus
High doses of glucocorticoids worsen hyperglycemia in people with diabetes, can reveal undiagnosed diabetes, and in people at risk for diabetes can precipitate hyperglycemia and new-onset diabetes (commonly called “steroid-induced diabetes”). In addition, glucocorticoids are the most common cause of the potentially life-threatening hyperglycemic hyperosmolar state in people with diabetes.
Classification of adrenal hormone preparations
Adrenal cortex hormone preparations are classified into:
- glucocorticoid preparations: hydrocortisone, prednisolone, dexamethasone, betamethasone, beclomethasone, methylprednisolone, prednisone, triamcinolone, clobetasol, mometasone, flumethasone, fluocinolone, fluticasone, flunisolide;
- mineralocorticoid preparations: fludrocortisone, deoxycorticosterone acetate.
In addition, glucocorticoids are additionally classified into drugs for systemic (intramuscular, intravenous), local (skin) and inhalation use.
Basics of treatment with adrenal hormones
Adrenal hormones are prescribed by a doctor, selecting the specific drug, its dose and route of administration individually, depending on the specific disease, its severity and the presence of concomitant diseases.
Glucocorticoids should be administered early in the morning - before 8:00 am, at the peak of the production of the adrenal cortex's own hormones. In this case, the maximum effect of the drugs develops. In addition, this mode of administration is a good prevention of a typical side effect that develops with long-term use of corticosteroids - secondary adrenal insufficiency.
If the entire daily dose cannot be administered in the morning, then it is divided into parts - 2/3 of the dose is prescribed before 8 a.m., and the remaining 1/3 of the dose is prescribed between 10:00 and 12:00.
In severe diseases, glucocorticoids are administered in pulse therapy, which involves a single intravenous injection of very large doses of the drug (most often methylprednisolone) for a short time (half an hour to an hour). This mode of administration can be used for no longer than three days in a row.
APPLICATION IN DERMATOLOGY
Glucocorticoids are used externally in the form of ointments, creams, gels, and lotions for a number of skin diseases. They have a local anti-inflammatory, anti-allergic effect, eliminate swelling, hyperemia, and itching. When using glucocorticoids externally, it is very important, depending on the location and nature of the lesion, to choose the optimal dosage form, each of which has some features (Table 13).
Table 13.
Features of the action of dosage forms for external use.
| Fat; the active substance is released slowly. | ||
| Cream | Preferred for intertriginous processes. Cosmetically more convenient. | May cause dryness and irritation, especially on damaged skin. |
| Lotion | Preferable for exudative processes. Convenient for use on hairy parts of the body. |
Classification
Glucocorticoid preparations for external use are traditionally divided into several groups, depending on the strength of the local anti-inflammatory effect. Moreover, there are some, not of fundamental importance, differences between the classifications considered in different literary sources. According to the above classification (Table 14), drugs are divided into 4 groups.
Table 14.
Classification of glucocorticoids for external use.
| Clobetasol propionate 0.05% | Dermovate | |
| Chalcinonide 0.1% | Chalciderm | |
| Strong | Betamethasone valerate 0.1% | Betnovate, Celestoderm-B |
| Budesonide 0.0375% | Alupent | |
| Halomethasone monohydrate 0.005% | Sikotren | |
| Hydrocortisone 17-butyrate 0.1% | Laticort, Lokoid | |
| Mometasone furoate 0.1% | Elokom | |
| Dexamethasone 0.025% | Esperon | |
| Triamcinolone acetonide 0.1% | Polcortolone ointment, Fluorocort | |
| Triamcinolone acetonide 0.025 and 0.1% | Triacort | |
| Flumethasone pivalate 0.02% | Locacorten, Lorinden | |
| Fluocinolone acetonide 0.025% | Sinalar, Sinaflan, Flucinar | |
| Fluticasone propionate 0.05% | Cutivate | |
| Medium strength | Prednisolone 0.25% | Deperzolon |
| Prednisolone 0.5% | Prednisolone ointment | |
| Prednicarbate 0.25% | Dermatop | |
| Fluocortolone 0.025% | Ultralan | |
| Weak | Hydrocortisone acetate 0.1%, 0.25%, 1%, 5% | Hydrocortisone |
The most powerful effect is exerted by fluorinated glucocorticoids (“very strong” and “strong” drugs), which are poorly absorbed from the surface of the skin and have a predominantly local effect. Their disadvantage is the more frequent development of local adverse reactions compared to other drugs (see below).
Drugs belonging to groups III and IV (prednisolone, hydrocortisone acetate and others) are characterized by a greater ability to be absorbed from the area of application, therefore their local effect is weaker, and the likelihood of developing systemic adverse reactions is higher.
The strength of the drug also depends on the type of dosage form (ointment > cream > lotion) and concentration.
One of the modern principles of systematization of glucocorticoid drugs for external use is their division into four generations, differing in their characteristics of action. To the first generation
includes hydrocortisone acetate, which has the mildest effect.
The second
is prednisolone, which has a moderate effect.
Third generation
is represented by a wide range of fluorinated glucocorticoids, which have a “strong” or “very strong” local effect.
The fourth group
includes “strong” glucocorticoids that do not contain a fluorine atom in their structure - hydrocortisone-17-butyrate, mometasone furoate, as well as a drug of moderate activity - prednicarbate.
The fourth generation drugs created in recent years are considered the most preferable, since they successfully combine the positive properties of their predecessors: they have high activity comparable to the potency of fluorinated glucocorticoids, and minimal undesirable local effects characteristic of hydrocortisone acetate.
Mometasone furoate ( elokom
- cream, ointment, lotion) refers to fourth generation glucocorticoids. It is superior to hydrocortisone, dexamethasone and betamethasone in its ability to block the formation of cytokines (interleukin-1 and interleukin-6), which play an important role in skin inflammation, in particular in psoriasis. Controlled clinical studies have shown higher efficacy of mometasone in psoriasis and atopic dermatitis compared to hydrocortisone and betamethasone. The drug is well tolerated and does not cause skin atrophy. Mometasone has a prolonged effect, so it is applied once a day. Thanks to its improved tolerability, it is suitable for use in children and the elderly.
Hydrocortisone 17-butyrate ( laticort, locoid
), unlike hydrocortisone acetate, is poorly absorbed from the area of application, so the likelihood of systemic action is extremely low. At the same time, like fluorinated glucocorticoids, it has a powerful local effect, but, unlike the latter, it rarely causes local adverse reactions and may have wider use.
Prednicarbate ( dermatope
) is a glucocorticoid with a moderate degree of activity and is characterized by a mild, gentle local effect. It practically does not cause systemic adverse reactions. Local effects are very rare. Can be used on large surfaces and applied to areas of the skin with the most increased sensitivity (face, groin area). Controlled clinical studies have shown high efficacy and good tolerability of prednicarbate in children from 2 months to 16 years and the elderly, therefore the drug is recommended primarily for use in these age groups.
Indications
Psoriasis, eczema, neurodermatitis, contact dermatitis, solar dermatitis, seborrheic dermatitis, atonic dermatitis, lichen planus, discoid lupus erythematosus, erythroderma.
Rules of application
- Before using glucocorticoid drugs, it is necessary to establish an accurate diagnosis.
- It is recommended to start treatment with the use of a drug with weak activity (Table 14), if there is no effect within 2-3 weeks, switch to a stronger one, and after achieving the effect, use a weak glucocorticoid again.
- Drugs with very strong activity (clobetasol propionate, chalcinonide) should be used only for lichenoid eczema and discoid lupus erythematosus.
- The drug is applied to clean skin (after a bath or shower) 2 times a day, in a thin layer, do not rub or massage. It is recommended to carry out the procedure with gloves. Mometasone furoate and fluticasone propionate, which have a prolonged effect, are applied once a day, which is convenient for diseases that require long-term use of glucocorticoids (eczema, psoriasis).
- After applying the drug to enhance the therapeutic effect (usually for psoriasis), you can use occlusive dressings for a short time, no more than 2 days.
- The process of releasing the active substance from an ointment is usually slower than from a cream, so for chronic processes it is preferable to use an ointment.
- When the lesion is localized on the scalp, it is recommended to use a gel or lotion.
- If an infection is suspected, combined topical glucocorticoids containing antimicrobial components should be used (see below).
Adverse reactions
- From the skin:
- atrophy (more often on the face - “corticosteroid face”, therefore, if possible, strong ointments should not be used on the face, with the exception of hydrocortisone 17-butyrate); striae; depigmentation; skin irritation; telangiectasia;
- acne;
- Tinea incognito
is an atypical clinical picture of dermatomycosis when using glucocorticoids (both locally and systemically); - perioral dermatitis (more often in young women; tetracycline can be used for treatment for 4-6 weeks);
- hirsutism or frontal alopecia in women.
- Accession or dissemination of infection.
- Systemic action
(with long-term use, application to large areas of the body, more often in children and when using occlusive dressings). - Withdrawal syndrome
(usually requires resumption of the use of local glucocorticoids). - Acne, including acne rosacea
. - Perioral dermatitis.
- Scabies.
- Tuberculosis.
- Syphilis.
- Viral and helminthic skin lesions.
- Bacterial and fungal skin infections that have not previously been treated with other drugs.
- Skin reactions after vaccination.
- During pregnancy, it is not recommended to use for a long time and on large areas of the body.
Contraindications
Features of use in children
In children, with local use of glucocorticoids, there is a higher susceptibility to their systemic action
than in adults (including suppression of the function of the hypothalamic-pituitary-adrenal system, the development of Cushing's syndrome, growth and development delay), since the ratio of surface area to body weight in children is greater.
Therefore, glucocorticoid preparations should be used in limited areas, especially in newborns, if possible, for a short course. In children under 1 year of age, only ointments with hydrocortisone (no more than 1%) or the fourth generation glucocorticoid prednicarbate should be used; for children under 5 years of age, ointments of medium strength and hydrocortisone 17-butyrate should be used.
Combination drugs
Combination ointments and creams are produced, which, along with glucocorticoids, include other components (Table 15). They may include antibiotics (neomycin and others), drugs that combine antifungal and antibacterial activity (miconazole, triclosan and others), antifungal and antitrichomoniacal action (natamycin), antiseptics, salicylic acid, local anesthetics, vitamin-like compounds, antihistamines.
Some features of the composition of the drug may be indicated by the presence of an additional letter in its trade name. For example, flucinar N
includes the antibiotic neomycin,
sinalar K
- the antifungal agent clioquinol,
lorinden A
- salicylic acid.
In other cases, combination drugs have special trade names (localen, triderm)
.
Preparations containing antimicrobial components are recommended for use in case of a bacterial or fungal infection, suspicion of it and a high probability of its development (weeping processes, intertriginous lesions, anogenital and senile itching). It should be borne in mind that neomycin, when applied externally, can be absorbed and have oto- and nephrotoxic effects, therefore dosage forms containing it should not be used for a long time and on large surfaces.
Salicylic acid has a kerato- and squamolytic effect, promotes the penetration of glucocorticoids through excessively keratinized epidermis, restores the protective cover of the skin, and has a weak antiseptic effect. Therefore, drugs that contain it are advisable to use for diseases accompanied by increased keratinization of the epidermis, desquamation, hyperkeratosis, callus, for example, with lichenoid eczema, chronic cases of psoriasis, ichthyosis and others.
Table 15.
Combined preparations of glucocorticoids for external use.
| Vipsogal | Gentamicin1 | |
| Salicylic acid | ||
| Panthenol2 | ||
| Diprogent | Gentamicin | |
| Diprosalik | Salicylic acid | |
| Triderm | Gentamicin | |
| Clotrimazole1,3 | ||
| Celestoderm-B with garamycin | Gentamicin | |
| Halomethasone | Sikorten plus | Triclosan1,3 |
| Hydrocortisone acetate | Oxycort | Oxytheracycline1 |
| Hydrocortisone 17-butyrate | Pimafukort | Neomycin1 |
| Natamycin2,4 | ||
| Sibicort | Chlorhexidine5 | |
| Difluocortolone | Travocort | Isoconazole1,3 |
| Prednisolone | Mycozolon | Miconazole1,3 |
| Aurobin | Triclosan | |
| Lidocaine6 | ||
| Panthenol | ||
| Dermozolon | Iodochlorohydroxyquinoline1,3 | |
| Triamcinolone | Polcortolon TS | Tetracycline11 |
| Flumethasone | Localizan | Salicylic acid |
| Lorinden A | Salicylic acid | |
| Lorinden S | Iodochlorooxyquinoline | |
| Fluocortolone | Ultraproct | Clemizole7 |
| Cinchocaine6 | ||
| Fluocinolone | Sinalar K | Clioquinol1,3 |
| Sinalar N | Neomycin | |
| Flucinar N | Neomycin | |
Notes:
| ||
APPLICATION IN OPHTHALMOLOGY AND ENTRYNOLARYNGOLOGY
The use of glucocorticoids in ophthalmology is based on their local anti-inflammatory, antiallergic, and antipruritic effects. They prevent the expansion of capillaries, reduce their permeability, inhibit the migration of leukocytes, the release of kinins, reduce the deposition of fibrin, collagen, and the formation of scar tissue. When used, pain, burning, lacrimation and photophobia are reduced.
Indications
are various inflammatory diseases of eye tissue of non-infectious etiology, including after injuries and operations (iritis, iridocyclitis, scleritis, keratitis, uveitis, severe forms of conjunctivitis and others).
The most preferred are special preparations of glucocorticoids for topical use - solutions, suspensions, ointments (Table 16). They have a more pronounced local anti-inflammatory effect than glucocorticoids used orally or parenterally in such situations. The most effective “ophthalmic” drugs are fluorometholone and prednisolone acetate.
In particularly severe cases, glucocorticoids can be administered subconjunctivally. For this, dexamethasone and betamethasone phosphate are used, and injections of the second are less painful. There is evidence of the possibility of subconjunctival administration of betamethasone phosphate/dipropionate (diprospan)
.
Glucocorticoids are contraindicated
for acute infectious eye diseases. If necessary, combination drugs containing antibiotics are used.
Table 16.
Glucocorticoids for local use in ophthalmology. Applied Therapeutics, 1995 [8]
| Alcohol | Maxidex | 0,1% | Suspension | 40% | |
| Phosphate | Decadron | 0,1% | Solution | 19% | |
| 0,05% | Ointment | 12% | |||
| Fluorometholone | – – | Efflumidex | 0,1% 0,25% | Suspension Suspension | 31% 35% |
| Acetate | Flarex | 0,1% | Suspension | 48% | |
| Prednisolone | Acetate | Econopred | 0,12% | Suspension | 34% |
| Econopred plus | 1,0% | Suspension | 52% | ||
| Phosphate | Inflamaze | 0,12% | Solution | 23% | |
| Inflamaze forte | 1,0% | Solution | 28% |
Adverse reactions
Despite the fact that glucocorticoids, when applied topically, in contrast to systemic administration, do not enhance, but rather inhibit the formation of chamber humor, they can also cause an increase in intraocular pressure (dexamethasone to the greatest extent, fluorometholone to the least) and lead to the development of glaucoma . Exophthalmos may be present. Sometimes a serious complication is posterior subcapsular cataract. In diseases accompanied by thinning of the cornea, perforation is possible.
Combination drugs
In ophthalmological and otorhinolaryngological practice, a number of combination drugs are used, which, in addition to glucocorticoids, include antibiotics (Table 17). They combine anti-inflammatory and bactericidal effects, and more preferable are drugs that include the glucocorticoid betamethasone, which has less effect on intraocular pressure (Garazon)
.
In ophthalmology
These drugs are used for inflammatory and allergic eye diseases, if a bacterial infection is present or suspected (staphylococcal blepharoconjunctivitis, fluctenular and microbial-allergic keratoconjunctivitis, keratitis, episcleritis, dacryocystitis, iridocyclitis, eye injuries and others).
In otorhinolaryngology
indications for the use of combined drugs are acute and chronic external otitis; eczema of the external auditory canal; seborrheic dermatitis; contact dermatitis complicated by secondary infection; allergic and vasomotor rhinitis, complicated by secondary infection.
Precautionary measures.
It is not recommended to use the same bottle of the drug to treat otitis, rhinitis and eye diseases to avoid the spread of infection.
It is not advisable to use these drugs for the treatment of otitis media, which requires systemic (oral, parenteral) use of antibiotics. The drug maxitrol
, containing two ototoxic antibiotics (neomycin and polymyxin B), can only be used in short courses.
Table 17.
Combined preparations of glucocorticoids for use in ophthalmology and otorhinolaryngology.
| Betamethasone Gentamicin | Eye/ear drops | Eyes: 1-2 drops 3-4 times a day; in the acute stage, 2 drops every 1-2 hours with subsequent reduction. | |
| Ears: 3-4 drops 2-4 times a day, or a tampon is placed for 24 hours, which is moistened with the drug every 4 hours. | |||
| Eye ointment | Placed 3-4 times a day in the conjunctival sac; in the acute stage - every 2 hours. | ||
| Sofradex | Dexamethasone Neomycin Gramicidin | Eye/ear drops | Eyes: 1-2 drops 4-6 times a day; more often in the acute stage. Ears: 2-3 drops 3-4 times a day. |
| Eye/ear ointment | Placed 1-2 times a day in the conjunctival sac or ears. | ||
| Gikomycin-Teva | Hydrocortisone Neomycin | Eye/ear/nasal drops | 2-3 drops every 1-4 hours in the eye, ear or each half of the nose; after inflammation subsides, 1-2 drops 3-4 times a day. |
| Eye/ear/nasal ointment | Apply 1-3 times a day. | ||
| Maxitrol | Dexamethasone Neomycin Polymyxin B | Eye drops | 1-2 drops 4-6 times a day; in the acute stage, 2 drops every 1-2 hours |
| Eye ointment | Apply 3-4 times a day. |
| © 2000-2009 NIIAH SGMA | ||
Features of treatment with adrenal hormones
Due to their immunosuppressive effect, adrenal hormone preparations can mask the symptoms of acute infectious diseases and reduce the body's resistance to infection.
Abrupt cessation of the use of corticosteroids is dangerous due to the development of acute adrenal insufficiency and shock - a sharp drop in blood pressure. In addition, there is a significant deterioration in the patient's condition, increased body temperature, pain in muscles and joints. Therefore, discontinuation of adrenal hormones after long-term use must be carried out gradually.
In the practice of a modern dermatologist, topical corticosteroids occupy a special place. With their help, it is possible to quickly cope with the symptoms of inflammation in many dermatoses. Most doctors cannot imagine their daily practice without these medications, the history of which dates back only a few decades. True, recalling the beginning of the corticosteroid era in medicine, one cannot help but mention that last year marked 155 years since T. Addison (1855) described the clinical picture of damage to the adrenal glands, drawing close attention of physiologists to the cortical layer of this organ. Just a year later (in 1856) Ch.-E. Brown-Sequard found that after removal of both adrenal glands, experimental animals quickly died “with phenomena of progressive weakness, difficulty breathing and general paralysis.” The administration of an extract of the adrenal glands caused a significant increase in blood pressure in animals, vascular contraction and an increase in the duration of skeletal muscle contraction. By 1891, the first attempts to treat Addison's disease using an extract from the adrenal glands of animals dated back to 1891. The isolation and synthesis of the adrenal hormones themselves took place already in the twentieth century. Adrenaline was the first to be isolated in its pure form in 1901, but the corticosteroid hormones themselves were isolated and synthesized several decades later. In 1929, the American rheumatologist Ph. Hench observed remission of rheumatoid arthritis during jaundice, and in 1930 noted the same effect in women with arthritis during pregnancy. These observations allowed Ph. Hench suggests that during pregnancy and jaundice, an anti-inflammatory substance called “substance X” is produced. It was later proven that “substance X” accumulates in the body during jaundice, since the affected liver is not able to remove it from the body. In 1948, biochemist E. Kendall and doctor L. Sarett isolated 17-hydroxy-11-dehydrocorticosterone from bile, called substance E. After administering this substance to a patient with rheumatoid arthritis, a positive effect was obtained. From that moment on, there was an undoubted breakthrough in the treatment of many diseases, including those previously considered incurable. In 1950 Ph. Hench and E. Kendall received the Nobel Prize in Physiology or Medicine "for their discoveries concerning adrenal hormones, their structure and biological effects."
A “revolution” in dermatology occurred in 1952, when hydrocortisone was first used to treat dermatitis, which was a turning point in the treatment of inflammatory skin diseases (Fig. 1).
Figure 1. Chemical formula of hydrocortisone.
In the 60s of the 20th century, domestic scientists V.A. Rakhmanov, N.S. Smelov, A.A. Studnitsin noted the positive effect of hydrocortisone ointment in the treatment of eczema, neurodermatitis, and dermatitis. Almost 50 years have passed since then, and topical steroids have maintained their leading position in the treatment of the most common dermatoses all these years. This is due to the fact that topical steroids have the following pharmacodynamic effects:
- anti-inflammatory;
- immunosuppressive;
- vasoconstrictor;
- antiproliferative;
- antipruritic.
The mechanism of action of topical steroids is associated with hyposensitization of skin cell receptors for histamine and serotonin, blockade of histaminase A2, increased hyaluronidase activity, which causes a decrease in the permeability of the vascular wall, exudation, itching, as well as normalization of vascular tone, stabilization of cell membranes. The anti-inflammatory effect of topical steroids is due to the inhibitory effect on phospholipase A2, which is necessary for the synthesis of arachidonic acid. This inhibition mechanism leads to the suppression of the formation of inflammatory mediators (prostaglandins, leukotrienes, interleukins, complement components, etc.). There is a decrease in the release of lysosomal enzymes. Topical steroids cause inhibition of the migration of lymphocytes and macrophages, a delay in the proliferation of fibroblasts and collagen synthesis, and a decrease in the number of Langerhans cells and mast cells. All this ensures the clinical effect of topical corticosteroids.
In the first years of using topical hydrocortisone preparations, it was noted that they were well tolerated by patients, but their effectiveness in psoriasis and other dermatoses was low. The next step was to add a double bond to the steroid molecule. This is how prednisolone appeared, which became 4 times more active than hydrococortisone (Fig. 2).
Figure 2. Chemical formula of prednisolone.
In order to increase anti-inflammatory activity, back in the 50s it was proposed to include one or two halogen atoms (fluorine or chlorine) in the corticosteroid molecule. A new stage has begun in the history of the creation of steroids - the appearance of halogenated drugs (Fig. 3).
Figure 3. Chemical formulas of betamethasone (a) and mometasone furoate (b).
The introduction of a halogen into the corticosteroid molecule increased its anti-inflammatory activity. In the presence of halogen, the metabolism of the steroid slowed down, i.e., the drug existed longer in an active form, and the binding of the drug to transcortin in the blood was also difficult, which led to an increase in the period of residence of the biologically active fraction of the drug in the blood. Consequently, the risk of side effects, both local and systemic, was higher with halogenated drugs. A correlation has been established between clinical effectiveness and the severity of side effects, especially with long-term and/or regular use of halogenated drugs, primarily in chronic allergic dermatoses. A variety of undesirable reactions occurred: local atrophy of the skin and subcutaneous fat, hypertrichosis, hypo- and hyperpigmentation of the skin, decreased elasticity, telangiectasia, stretch marks, dyschromia, steroid acne, rosacea-like rashes, perioral dermatitis. All these phenomena have given rise to a wary attitude towards topical corticosteroids not only among patients, but also among many doctors. Hormonephobia has emerged, which specialists still have to fight to this day. Complications were especially pronounced when using drugs on the face.
In parallel with work on the activity of the molecule, research was carried out on ways to facilitate the penetration of drugs into the skin for a faster onset of action. The relationship between the rate of onset of the anti-inflammatory effect and the lipophilicity of the steroid has been proven. The latter did not increase the safety of the glucocorticoid, but guaranteed increased affinity for the skin and was ensured by the inclusion of hydrocarbon chains in the steroid ring - propionate, valerate, butyrate, etc.
The history of the creation of topical steroids has reached a natural stage - the need to create strong and at the same time safe agents, which was achieved by replacing halogen atoms with hydrocarbons. Thus, the high anti-inflammatory activity of the corticosteroid was maintained with a significant reduction in the risks of adverse events.
In 1990, the latest generation drug was created - methylprednisolone aceponate (Advantan), which met all modern requirements. The molecule of this drug has a methyl group at position C6, which determines its high activity. The absence of fluorine and chlorine at positions C6, C9 or C12, typical of most strong topical steroids, minimizes local and systemic side effects.
Double esterification (at positions C17 and C21) ensures optimal lipophilicity of the molecule, rapid penetration through the epidermis and high concentration in the dermis. This property fundamentally distinguishes the highly active methylprednisolone aceponate from its weakly active predecessor methylprednisolone.
Methylprednisolone aceponate has special pharmacokinetics: it is active specifically in the lesion and does not affect healthy skin. Due to lysosomal inflammatory enzymes, methylprednisolone aceponate is converted into methylprednisolone propionate, the activity of which is 2.5 times higher. Over the 20 years since the beginning of the use of this drug, significant clinical experience has been accumulated. Since its launch, more than 50 million patients have benefited from treatment with methylprednisolone aceponate (Advantan). Various studies have assessed the effectiveness and safety of more than 15 thousand adults and children.
Modern requirements for topical steroids remain the same: they must be highly effective, proven in studies that meet the standards of evidence-based medicine (multicenter randomized clinical trials that meet GCP standards); have a variety of dosage forms for topical use necessary to achieve an effect at different stages of the inflammatory process and on any area of the skin; be safe (low absorption, minimum side effects, use at any age, possibility of long-term use); be easy to use (application once a day, no odor, no greasy shine, no staining of clothes).
Methylprednisolone aceponate has all of these properties (Fig. 4).
Figure 4. Chemical formula of methylprednisolone aceponate (Advantan).
Firstly, the effectiveness of methylprednisolone aceponate has been confirmed in many Russian and foreign studies. Thus, E. Haneke, in a multicenter, double-blind study using patients with atopic dermatitis (AD) who received methylprednisolone aceponate, proved its high effectiveness, similar to that of betamethasone valerate (Table 1).
P. Fritsch also proved the high effectiveness of methylprednisolone aceponate in a double-blind study involving more than a thousand patients with eczema (Table 1).
At the same time, the safety of methylprednisolone aceponate was proven in patients with both AD and eczema (Table 2).
Thanks to 4 dosage forms (emulsion, cream, ointment, fatty ointment), methylprednisolone aceponate provides rapid elimination of inflammatory symptoms of various types.
Secondly, when methylprednisolone aceponate is used externally, its systemic effect is minimal. R. Zaumseil, H. Fuhrman et al. showed that after applying a significant amount of methylprednisolone aceponate (40 g/day) to large surfaces of the skin, there were no dysfunctions of the adrenal glands: the level of cortisol in the blood plasma and its circadian rhythm remained within normal limits (Fig. 5).
Figure 5. Plasma cortisol levels when the drug is applied to the skin at a dose of 40 g/day.
Methylprednisolone aceponate is indicated for adults and children over 4 months of age with AD, neurodermatitis, eczema, simple and allergic dermatitis. It is important to note that the wide age range, as well as the possible area of application (up to 60% of the body surface) and the duration of continuous treatment (up to 12 weeks in adults, up to 4 weeks in children; up to 2 weeks for emulsion), are clearly indicated in the instructions for use and do not raise questions or double interpretations.
Thirdly, due to the high lipophilicity of methylprednisolone aceponate, a depot is created in the epidermis, which allows the drug to be used only once a day, thereby significantly reducing treatment costs compared to most steroids indicated 2-3 times a day.
The history of the emergence and development of corticosteroid therapy shows the path traveled by pharmacology from the creation of the first topical corticosteroid drugs to the synthesis of topical steroids with an optimal combination of basic properties.