A hematoma is an accumulation of blood in the tissues of the human body, and its occurrence is caused by damage due to falls and blows. In some cases, the appearance of a hematoma is not associated with physical effects, but is explained by the presence of a specific disease in a person.
In most situations (this applies to small hematomas), serious consequences do not occur, and the inflammation itself disappears after some time. However, there are often cases that require medical consultation and qualified treatment. Ignoring a bruise can lead to the formation of a cyst or tissue necrosis.
Why it is not recommended to treat a hematoma on the leg at home
If there is large accumulation of blood under the skin, it must be removed. There are enough videos and articles on the Internet describing this procedure at home, but you absolutely cannot follow such advice. Firstly, a person risks damaging his leg even more and disrupting its normal functioning, even to the point of disability. Secondly, and more likely, you can introduce an infection into the body and provoke even greater inflammation. Thirdly, only an experienced doctor using special equipment will do this carefully, but independent attempts can permanently disfigure the skin and leave unaesthetic scars on it.
Causes
Hemorrhage usually occurs after injury. This could be a bruise of the skin, internal organs, a concussion or bruise of the brain, an injection with thin (sharp) objects. Sometimes blood leaves the vessels and pours into the skin and internal organs as a result of infections, autoimmune diseases, and poisoning. The occurrence of hemorrhages and bruises is promoted by increased fragility of blood vessels, fasting, lack of vitamins in food, high blood pressure, and congenital bleeding disorders.
At CELT you can get a consultation with a traumatologist-orthopedic specialist.
- Initial consultation – 3,000
- Repeated consultation – 2,000
Make an appointment
Treatment of hematoma on the leg
Typically, a hematoma on the leg after a bruise is treated by two methods: conservative and surgical. The first category includes: cold and warm compresses, pressure bandages, taking analgesics, applying ointment, physiotherapeutic manipulations.
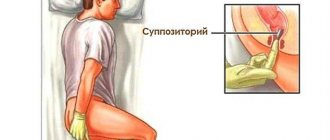
The second group involves performing a puncture - surgical removal of accumulated blood from the site of a bruise with the application of a suture and an aseptic bandage.
Treatment of a serious hematoma on the leg must be carried out under the guidance of a doctor; this will speed up the healing process and prevent unpleasant consequences.
Predisposing factors
The formation of hematomas occurs after injuries, including pinching, blows, squeezing, and bruises. Subarachnoid hemorrhage does not fall into this category, since it does not appear due to trauma, but due to damage to an unchanged vessel. Often small hematomas appear due to eating large quantities of food or drinking alcoholic beverages. This is due to stretching of the gastrointestinal tract and the appearance of cracks.
The development of pathology is influenced by vascular weakness and problems with blood clotting. Often due to a weakened immune system due to infections or age-related changes, the likelihood of pus accumulating in the affected area increases.
Orthopedics and traumatology services at CELT
The administration of CELT JSC regularly updates the price list posted on the clinic’s website. However, in order to avoid possible misunderstandings, we ask you to clarify the cost of services by phone: +7
| Service name | Price in rubles |
| Appointment with a surgical doctor (primary, for complex programs) | 3 000 |
| X-ray of the chest organs (survey) | 2 500 |
| Ultrasound of soft tissues, lymph nodes (one anatomical zone) | 2 300 |
All services
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Introduction
Damage to soft tissues accompanies human life.
A bruise is a closed mechanical damage to soft tissues caused by short-term exposure to a damaging factor, which is not accompanied by the formation of wounds. When a bruise occurs, small vessels always rupture, followed by hemorrhage, the severity of which can vary. Damage to soft tissues, regardless of the cause that caused them, constitutes the majority of visits to primary health care institutions. Bruises usually occur when falling or hitting hard objects. In children of the first years of life, household and play injuries, bruises of the soft tissues of the face and neck predominate. At older ages, the main types of injuries are transport, sports, and street injuries [1]. Damage to superficial soft tissues is always accompanied by swelling of the injury site as a result of the skin being soaked in lymph, blood and local aseptic inflammation. The amount of swelling depends on the area of damage to the subcutaneous tissue at the site of the injury. For example, in the area of the cranial vault, due to the thin layer of subcutaneous fat, edema is insignificant, while even mild bruises of the face are accompanied by the development of pronounced edema [2]. Bleeding that continues deep into the tissue often leads to additional trauma to adjacent tissues as a result of their compression, which is accompanied by a gradual increase in pain and dysfunction. A bruise sometimes accompanies other injuries (fracture, etc.), so you should always exclude more complex injuries and evaluate the consequences of injuries [2, 3]. Soft tissue injuries are accompanied by pain of varying intensity. Thus, with bruises of large nerves and their endings, the pain is always sharp, shooting. With bruises of the torso and limbs (shoulder, thigh), tense hematomas can form, with bursting pain, sometimes with superficial numbness.
Treatment of soft tissue bruises is traditionally aimed at eliminating the above symptoms and excluding more severe pathology [4]. Currently, there are treatment standards - clinical guidelines for the provision of emergency medical care for soft tissue injuries, where a special place is given to the issues of immobilization, wound care and pain relief [5]. The administration of opioid and non-opioid analgesics is recommended in combination with antihistamines (metamizole sodium, trimeperidine, diphenhydramine). It is necessary to perform immobilization as soon as possible. Even with minor injuries, it is better to apply a tight bandage to the bruised area or immobilize with an orthosis. This will ensure peace of the bruised segment, normalize microcirculation, and reduce motor activity. Some orthotic products have a micromassage effect, which also has a beneficial effect on reparative processes. Along with this, analgesic therapy is carried out. These activities must be performed within the first 3 days. Then it is possible to use warming procedures and physiotherapeutic measures. Local therapy with ointments and gels can be used from the 1st day if they do not have a warming effect and do not increase vascular permeability.
Soft tissue bruises, and therefore pain, are inherently interconnected. Pain is a unique psychophysiological state of a person that occurs as a result of exposure to super-strong or destructive stimuli and causes functional or organic disorders in the body. Moreover, pain is subjective in nature, its perception is based on personal experience associated with damage in the early period of life. Its perception is determined not only by the source of pain, but also by such, at first glance, non-obvious factors as the psychophysical and emotional characteristics of the individual, his cultural level, family training and many others. Most often it is characterized as a psychophysical state of a person, which is a characteristic reaction to various organic and functional disorders caused by the action of various stimuli. Pain is both a physical sensation and an emotional reaction to it. Pain expert Margot McCaffrey's pithy definition is "anything that a patient says hurts them."
The functioning of the nociceptive system is mediated by neurochemical mechanisms realized by endogenous peptides and mediators, including histamine, substance P, kinins, prostaglandins, leukotrienes, potassium and hydrogen ions [4–6]. When pain occurs, the processes of hypercoagulation and lipid peroxidation are activated, the content of proteolytic enzymes increases, which causes tissue destruction. Pain contributes to the development of tissue hypoxia, degenerative processes and disruption of microcirculation in tissues. This, in turn, increases the alteration of injured tissues [7].
Thus, pain is a complex psychophysiological phenomenon, which, both from an ethical and legal standpoint, requires treatment aimed at relieving pain [8]. Understanding the complexity of its nature, mechanisms of development and regulation allows us to take a differentiated approach to the issue of choosing analgesic therapy.
One of the most effective means of protecting peripheral nociceptors that does not cause depression of vital functions are non-steroidal anti-inflammatory drugs (NSAIDs). The modern concept of effective pain relief for bruises and other types of injuries involves a multimodal approach - influencing various parts of the pain impulse. In this regard, it is advisable to combine the administration of NSAIDs with opiates or opioids for severe pain syndrome, for example, in case of shockogenic traumatic injuries.
Nonsteroidal anti-inflammatory drugs are the drugs of choice for the treatment of mild to moderate pain. Their anti-inflammatory effect is based on inhibition of cyclooxygenase (COX). One of the representatives of NSAIDs is ketoprofen, produced in various forms (tablets, injections, external ones). The triple effect - anti-inflammatory, analgesic and antipyretic - is due to blocking the enzymes COX-1 and COX-2 and, partially, lipoxygenase, which leads to suppression of the synthesis of prostaglandins (including in the central nervous system, most likely in the hypothalamus) and thromboxanes. Ketoprofen stabilizes in vitro
and
in vivo
liposomal membranes, at high concentrations
in vitro
suppresses the synthesis of bradykinin and leukotrienes. It does not have a negative effect on the condition of articular cartilage [9].
From the point of view of the ratio of anti-inflammatory and analgesic activity, ketoprofen seems to be the optimal molecule. Thus, according to an experimental study using a model of toothache, ketoprofen has the most pronounced anti-inflammatory effect compared to many NSAIDs, while the clinical effectiveness indicator (total reduction in pain after 4 hours) is the greatest for ketoprofen [10]. It is important to note that these experimental data were confirmed by data from a meta-analysis of 13 RCTs: with regard to the relief of moderate and severe pain, ketoprofen is significantly superior to diclofenac and ibuprofen [11].
Despite the fact that ketoprofen is a “traditional” non-selective NSAID, it is less capable of causing NSAID-associated gastrointestinal and cardiovascular complications - data from a Finnish population-based study assessing the causes of 9191 events in the upper gastrointestinal tract ( including cases of bleeding, ulcers and perforation). According to the results obtained, the likelihood of developing serious gastrointestinal complications when using ketoprofen was lower compared to other NSAIDs, such as diclofenac. Ketoprofen demonstrated a similar or even lower risk of developing gastrointestinal pathology than a number of selective NSAIDs [9–11]. The minimal negative effect of ketoprofen on the cardiovascular system has been demonstrated in a number of large-scale epidemiological studies.
In a study of the analgesic effect of ketoprofen in the acute period of injury in victims with various skeletal injuries, the onset of analgesic effect was noted within 12.2 ± 2.6 minutes after intramuscular application of 100 mg of ketoprofen. The use of 200 mg reduced the wait for the development of analgesia to 8.2±2.2 minutes. At the same time, in patients with severe musculoskeletal injury, ketonal was used at a dose of 200 mg in combination with intravenous tramadol (100 mg), and the analgesic effect was realized in 5.8 ± 0.9 minutes, which was faster compared to tramadol monotherapy at the same dosage (6.0±1.2 min) [12].
Purpose of the study:
determine the effectiveness of analgesic therapy for bruises of the upper and lower extremities.