What to do if one day you notice the appearance of discharge from the penis? Should I panic or calm down and wait for it to go away on its own?
First you need to really calm down. Your body is your helper! It gives you a signal that your health is not good.
Very often, unusual discharge from the penis becomes the first, and sometimes the only, symptom of a serious illness. Therefore, a man, paying attention to his genital organ, must pay attention not only to its size, but also to the nature of the discharge.
There is no need to “diagnose” the disease yourself and self-medicate! Your attempts at self-medication will not bring recovery, but will only distort the symptoms of the disease and lead to the loss of time - precious in some serious diseases, and the disease will return with renewed vigor.
The field of urology is quite vast. At Alan Clinic we will help you get rid of many urological diseases.
Necessary examination for discharge in men
In case of strange discharge, the patient should consult a urologist. The doctor carries out diagnostics according to a certain algorithm.
It includes:
- Visual inspection of the penis, head of the penis, perineum, foreskin. The urologist will see whether there are deformities, injuries, signs of inflammation, various rashes, etc.
- Palpation of the lymph nodes in the groin. The doctor determines their size, whether they are hot or not, mobile or in tight contact with the skin, soft or dense. It also matters whether there are different expressions nearby.
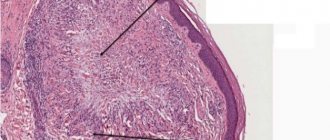
- Palpation of the prostate. With pathology of the organ, the lobes increase. This can be determined by massaging through the rectum. If there is a cancerous tumor, then the growths are uneven. Discharge – blood with clots from the urethra.
Instrumental studies are also needed, such as ultrasound of the pelvic organs, urography and computed tomography. They allow you to clarify the diagnosis. Diagnosis is always carried out in a complex manner, since it is impossible to recognize the exact causes of the disease on the basis of one test.
Diagnostics
The treatment methods that the doctor prescribes will be dictated by the origin of the disease. This is why competent, professional and accurate diagnosis is so important.
A comprehensive examination by a urologist/sexologist includes:
- Inspection (palpation);
- Hardware diagnostics: ultrasound of the prostate gland;
- Ultrasound of the bladder;
- Doppler examination of blood vessels (Dopplerography) - according to indications;
If the doctor deems it necessary, the following may also be prescribed:
- Additional laboratory tests (blood tests, urine tests, prostate secretions, spermogram);
- Computed tomography (CT);
- Needle biopsy;
- X-ray;
- Scintigraphy;
- Urethroscopy;
- Cystoscopy.
Discharge in men due to sexually transmitted infections
Sexual infections most often cause the appearance of atypical discharge from the urethra in men. Sexually transmitted infections are a group of diseases that are most often transmitted through sexual contact. Less commonly - through blood, through everyday contact or during childbirth. All sexually transmitted infections have both similar symptoms and some differences.
They are most often accompanied by discharge from the urethra (sometimes yellow, green, cheesy, foul-smelling), and are also characterized by burning and itching, pain during urination and during sexual intercourse. Sometimes a skin rash and other skin disorders appear.
The allocations are:
- Chronic chlamydia, uraplasmosis, mycoplasmosis (transparent, viscous discharge of moderate amounts). The number of leukocytes in the blood is increased on microscopic examination.
- Acute course of chlamydia, uraplasmosis, mycoplasmosis (white or translucent discharge of mucopurulent consistency). With chlamydia, a purulent substance accumulates on the head of the penis.
- Gonorrhea is characterized by a putrid smell of discharge. They have a thick, sticky consistency, yellow to yellow-green in color. Microscopic examination shows many leukocytes, epithelial cells from the urethra. In addition, itching, burning, and pain when urinating are added.
Often sexually transmitted diseases occur in one patient in combination. This could be gonorrhea along with chlamydia and gonorrhea, or syphilis and gonorrhea along with mycoplasmosis. Any combinations are possible. Therefore, the nature of the discharge can be very different.
Urogenital candidiasis (thrush) is not classified as venereal, since it rarely passes from a sick woman to a man. More often this is a consequence of decreased immunity and injury to the genitourinary system. With this disease, the discharge has a sour odor and a cheesy consistency. They also cause itching and burning when urinating.
Treatment of urethritis in Volgograd
APPOINTMENT WITH DOCTOR OLEG VIKTOROVICH AKIMOV
What is urethritis?
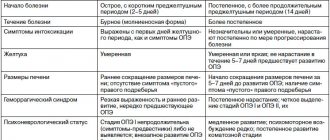
Urethritis is an inflammation of the urethra (urethra), the main manifestation of which is pain when urinating and discharge from the urethra. Urethritis occurs in both men and women. Urethral discharge in men can be physiological, and urethritis can occur without observable discharge. More importantly, some patients with obvious discharge do not realize the presence of the disease, since it does not bother them at all. The main syndrome is inflammation, manifested by dysuric symptoms, expressed to varying degrees (itching, burning in the urethra, pain when urinating, mucopurulent or purulent discharge). In the chronic form of the disease, the clinical picture is blurred, characterized by scant mucous discharge and a slight burning sensation along the urethra. When the spermatic tubercle in the posterior part of the urethra is involved in the process, ejaculation disorders may occur. The causes of infectious urethritis are most often sexually transmitted infections. The main group of pathogens are chlamydia, mycoplasma, ureaplasma, and trichomonas. Urogenital chlamydia affects more than 50 million people worldwide; it occurs 2-5 times more often than gonorrhea. As a result of infection with mixed urogenital flora, chronic forms of the disease dominate, often leading to infertility. In men, the following complications of urethritis are observed: the transition of acute to chronic urethritis, inflammation of the prostate gland (prostatitis), inflammation of the seminal vesicles (vesiculitis), inflammation of the testicle (orchitis), balanitis and balanoposthitis, narrowing of the urethra (urethral stricture). In women, urethritis is most often complicated by: disruption of the vaginal microflora (vaginitis), inflammation of the bladder (cystitis). There may be other very serious consequences - infertility (in both men and women). Urogenital chlamydia accounts for up to 60% of all nongonorrheal urethritis (NGU) in men. Treatment of chronic infectious urethritis currently poses a big problem.
What is the diagnosis of urethritis?
Diagnosis of urethritis is based on identifying complaints and examining the patient. Rarely use instrumental methods - examination of the urethra using a cystoscope. Urethroscopy allows you to determine the nature and stage of urethritis. Laboratory examinations are prescribed - taking material from the urethra. The diagnosis of urethritis is confirmed by the presence of an increased number of leukocytes in analyzes of more than 5 per field of view. Androflor of a scraping from the urethra allows you to determine the type of causative agent of the disease. The patient himself can easily test for the presence of urethritis; flakes or suspension will be visible in the first portion of urine.
What is chlamydia?
Chlamydia is one of the most common sexually transmitted infections (STIs). The cause of the disease is the bacterium Chlamydia trachomatis. Chlamydia infection occurs through sexual contact. The probability of contracting chlamydia through unprotected sex (vaginal sex, anal sex, oral sex) is 70% - 90%. Non-sexual transmission is rare, most often through hands, tools, underwear, and personal hygiene items contaminated with bacteria. This is due to the rapid death of chlamydia outside the human body.
Urogenital chlamydia does not have specific clinical symptoms; it usually proceeds torpidly, with few or asymptomatic symptoms. The initial site of infection is most often the urethral mucosa in men and the cervical canal in women. Chlamydia can also infect other mucous membranes covered with columnar epithelium (rectum, conjunctiva of the eye and pharynx). The danger of chlamydia lies in its asymptomatic course. Of the diseases that chlamydia can cause in men, the most common are urethritis and its complications: epididymitis, prostatitis, and less commonly, proctitis. The latent phase of the disease can last from a week to a month. Usually the clinical picture is mild, and sometimes the patient does not realize that he is infected. The disease can occur in the form of unexpressed inflammation of the urethra (urethritis): the presence in the morning of a cloudy droplet of liquid or an admixture of pus at the exit from the urethra is typical. There may be discomfort when urinating, itching in the urethra, spotting at the end of urination or during ejaculation. But the infection does not stop in the urethra. Microorganisms move into the prostate gland, affecting all the glands of this area, testes, and appendages. As a result, men develop infertility.
What is mycoplasmosis? What is ureaplasmosis?
Human diseases caused by mycoplasmas are grouped into the group of mycoplasmosis. This family is divided into 2 genera - the genus Mycoplasma, which includes about 100 species, and the genus Ureaplasma, which has only 3 species. The wide range of diseases caused by these microorganisms has recently forced scientists to closely study mycoplasmas. They affect the respiratory and genitourinary organs. Mycoplasmas can be transmitted through sexual contact, household contact, airborne droplets, and intrauterine transmission (from mother to fetus). In recent years, the number of mycoplasma and mixed infections has sharply increased, the fight against which poses significant difficulties due to the developing resistance of microorganisms to antibiotics and the characteristics of the body's responses. According to American doctors, mycoplasmas were found in 80% of women with symptoms of genital infection and in 51% of women with reproductive disorders. Moreover, in women they are detected more often than in men, and in higher titers. Numerous studies have shown that during nonspecific inflammation, M. hominis is sown 2 - 2.5 times more often than in healthy women. Diseases caused by mycoplasmas “in their pure form” are usually asymptomatic or even asymptomatic. Usually in the female body, mycoplasmas are located in the vagina, urethra and cervix, and in men - in the urethra and on the foreskin, which can lead to an infectious and inflammatory process. In addition, mycoplasmas can reduce sperm activity, and in some cases even lead to their death. Mycoplasmosis can lead to diseases such as prostatitis, sepsis, arthritis, urethritis, postpartum endometritis and many others. Mycoplasmosis and ureaplasmosis are not entirely clear diagnoses for many. Someone heard something, but not everyone knows what the threat is. Mycoplasmosis can bring a lot of trouble to both women and men. And since mycoplasmas are most often transmitted sexually, it is very important to maintain sexual hygiene and be promptly examined and treated if any infection is suspected.
What are the clinical manifestations of mycoplasmosis and ureaplasmosis?
- Mycoplasma genitalium is a pathogenic microorganism that can cause urethritis, cervicitis, and inflammatory diseases of the pelvic organs.
- M. genitalium most often causes urethritis in men, but low-symptomatic recurrent or asymptomatic forms also occur.
- It has been established that M. genitalium is the cause of mucopurulent inflammation of the cervix in women.
- There is evidence of a relationship between M. genitalium infection and fertility and pregnancy.
- Ureaplasma urealyticum and Mycoplasma hominis are microorganisms whose pathogenic properties occur only under certain conditions.
- U. urealiticum and M. hominis are opportunistic microorganisms that are found in 10-50% of practically healthy individuals of reproductive age.
- Under certain conditions, they can cause infectious and inflammatory processes of the genitourinary organs, often in association with other infections.
- Antibacterial therapy for these infections is indicated in the presence of clinical symptoms, planning pregnancy, or isolation of pathogens in quantities > 104 CFU/ml3.
What is the treatment for urethritis?
Treatment of urethritis begins only after determining the cause of the disease and should be comprehensive and strictly individual. It is carried out using various drugs, primarily antibiotics. Treatment methods depend on the duration of the disease. All sexual partners of the sick person should be treated. The course of treatment averages from 5 to 20 days; the drug and its dosage are selected after a face-to-face consultation, examination and tests. Even after completing a course of therapy, after some time you can again find obvious signs of urethritis. Therefore, monitoring is important, which is usually carried out 10 days after treatment.
UROCOMPLEX SV - intended for complex treatment of infections of the genitourinary system, both men and women:
- prevents the development of urethritis, prostatitis, cystitis, and infertility.
- prevents relapses of chronic genitourinary infections: ureaplasmosis, mycoplasmosis, trichomoniasis, chlamydia, etc.
- relieves the condition of urinary retention, urinary disturbances, and the formation of sand and stones.
- eliminates inflammation and swelling of the prostate, discomfort in the perineum, pain during urination and sexual intercourse.
Composition of OUR COMPLEX SV: sabal palm extract, pumpkin seed extract, African plum root extract, red root extract, bergenia leaf extract, sea buckthorn leaf extract, raspberry leaf extract, zinc, selenium, lycopene, indole-3-carbinol, vitamins B6, B12, AT 9. UROCOMPLEX SV is taken 2 times a day, 1 capsule.
What physical therapy methods are used to treat urethritis?
The goal of physiotherapy for urethritis is: anti-inflammatory and analgesic effect, elimination of the focus of inflammation in the mucous membrane and submucosal layer of the urethra, increasing the overall reactivity of the body, increasing outflow and activating reparative reactions in the focus of inflammation.
- Bactericidal methods: UHF inductothermy of the penile area, endourethral: SMT electrophoresis with antibiotics, electrophoresis with uroseptics, thermotherapy, laser therapy,
- Anti-inflammatory methods: UHF therapy, infrared laser therapy, magnetic therapy, laser therapy.
- Immunostimulating methods: ILBI, heliotherapy, ozone therapy.
Electrophoresis of antibacterial drugs and uroseptics is carried out outside of exacerbation of the disease. The concentration of medicinal substances in the inflammatory focus with this method increases by 1.5 times. It is possible to use intraorgan electrophoresis - galvanization of the urethral area during parenteral or oral administration of medications.
Laser therapy is used in a wide range. The contact technique is carried out on pain points, on the area of projection of the appendages, exposure is 30-60 s, for a course of 7-10 sessions. The intracavitary procedure is done transurethrally.
Thermomagnetic therapy. Superficial heating of the mucous membrane of the urethra and prostate gland to a depth of no more than 5 mm is required in order to sanitize the urogenital tract or provide better conditions for subsequent local drug therapy. For this purpose, special devices have been developed that allow heating of the urethra and gland using a transurethral or transrectal method evenly along the length of the urethra with a gradual rise in temperature from 39 to 45 ° C and automatic control of it directly in the urethra or rectum. For urethritis and prostatitis, urethral and rectal heating are used simultaneously against the background of exposure to a running magnetic field.
To increase immunity, intravenous laser irradiation of blood ; this is the most effective and universal method of laser therapy. Unlike local laser therapy procedures, the therapeutic effect is due to the activation of systemic healing mechanisms of the whole body, increasing the efficiency of the functioning of the blood supply, immune, and other organs and systems, as well as the entire body as a whole.
The effect of ozotherapy is achieved using autohemotherapy with ozone, rectal insufflations with an ozone-oxygen mixture and the use of ozone irrigation in overalls connected to an ozonator. The therapeutic effects of ozone are based on the known mechanisms of its biological action. The immunomodulatory effect of ozone makes it possible to gently correct immunodeficiencies; a decrease in blood viscosity leads to improved microcirculation and gas exchange at the tissue level.
Which doctor deals with men's discharge?
All diseases in men that are accompanied by discharge from the urethra are dealt with by a urologist. A urologist is a specialized specialist who is responsible for the diagnosis and treatment of pathologies of the genitourinary system.
The urologist at our clinic has extensive experience, constantly improves the level of his knowledge, and takes part in practical and educational seminars.
Men of all ages turn to him for help, starting from birth. All services are certified.
Answers to frequently asked questions:
- How to prepare for an appointment with a urologist?
- How to get tested for urological diseases?
- What tests can be done by a urologist?
- What diseases does a urologist treat?
- What symptoms should you consult a urologist for?
- What diagnostics can a urologist perform in your clinic?
- How to call a urologist at home?
- What urological equipment does your clinic have?
- Urological care in the clinic
- Urological care at home
- How to make an appointment with a urologist at the clinic?
Normal or pathological?
The urethra is the male urethra. From there, discharge appears from time to time. There is such a thing as urethrorrhea. It can be physiological or libidinal. A transparent discharge appears from the urethral outlet. This happens in the morning, immediately upon awakening, or when a man is sexually aroused.
Urethrorrhea can be more or less pronounced. The lubricant that is released during arousal contains sperm. Therefore, if you do not want to have children yet, you should protect yourself even during foreplay with the genitals. Discharge in men helps sperm pass through the urethra and into and past the partner's vagina. After all, the environment there is acidic, and this is harmful to the life of sperm.
Defecatory prostatorrhea may be the second cause of discharge in boys and men. When a person pushes, a discharge appears on the head of the penis that is odorless and colorless. They may sometimes contain white-gray inclusions. Their consistency is viscous. This is discharge from the prostate and seminal vesicles. It may appear when emptying the bladder is completed. This is then called voiding prostatorrhea. In extremely rare cases, a man notices such discharge after coughing. This is not a disease, but a disorder that can be cured.
The next type of discharge from the male genital organs is smegma. It includes the secretion of the sebaceous glands of the head of the penis and the foreskin. If a man washes, changes his underwear and does not wear other people's underwear, then these secretions will be washed off. And no attention will be focused on them. If hygiene is not so good, a fairly large amount of smegma may accumulate. Pathological flora will multiply and develop there, so the genitals and underwear will smell unpleasant.
Where to go for discharge in men
For many years, our clinic has been providing medical care to men with diseases accompanied by urethral discharge.
Why people often choose us:
- our clinic is open every day of the week;
- we have branches, so we provide the service to everyone quickly and at a convenient time, there are no queues;
- our medical staff works as a single team, so patients receive comprehensive care and guaranteed results;
- the professionalism of urologists allows a man to be restored to health in a matter of days using advanced treatment methods;
- we use only the best consumables and medicines;
- We provide services at home along with the collection of biomaterials for analysis;
- We maintain medical confidentiality.
In addition, all necessary tests can be performed at our clinic. It’s fast, comfortable, and most importantly – accurate results. The success of treatment largely depends on a correct diagnosis.
Treatment
Treatment of urological problems is a long and scrupulous process. In most cases, only a set of measures can help.
We use methods such as:
- drug treatment;
- physical therapy;
- prostate massage;
- treatment with active oxygen (ozone therapy);
- mud therapy (Dead Sea mud);
- medical and medicinal droppers;
- adjusting the patient’s lifestyle and nutrition;
- development of an individual prevention program;
- monitoring the patient's condition after treatment.
Treatment of discharge in men
Treatment directly depends on the identified pathogen or the cause of such a symptom and the degree of damage to the body:
- Candidiasis is treated with an antifungal cream, applied to the affected areas of the skin if there are no other symptoms other than discharge and redness of the head of the penis. The most commonly used cream is Clotrimazole. If the disease progresses, then treatment is complex. Oral medications are added.
- Ureaplasmosis requires taking antibiotics according to an individual regimen. The average course is 10 days. After a course of antibiotics, treatment to restore intestinal microflora is recommended.
- Chlamydia is also treated with antibiotics (tetracycline, fluoroquinols, macrolides), and in the chronic form this treatment is long-term.
- Mycoplasma is caused by a single-celled parasite. It is destroyed by erythromycin, doxycycline, tetracycline.
Antibiotics are most often used in therapy. The selection of drugs and dose is determined by the doctor. If you consult a doctor in a timely manner, treatment takes on average no more than 10 days. In the case of chronic diseases, therapy requires a longer period.
Discharge with odor
The first possible reason (and the most harmless) is poor hygiene. As mentioned above, smegma is normal (not indicating illness) male discharge. If you do not wash regularly, at least once a day, then smegma accumulates, bacteria multiply in it, causing not very pleasant odors. These odors may differ for different men.
If you follow good hygiene rules and still have an unpleasant odor, your doctor may suspect a metabolic disorder. In such cases, the most common cause is diabetes. Smegma will be released in quite large quantities, so the laundry will be wet.
Infections are also the cause of odor-bearing discharge in men. The pathological process mainly occurs in the urethra. Your doctor may suspect urethritis due to a gonorrheal infection. The nature of the discharge is described above. If the discharge from the penis in men smells sour, urogenital candidiasis is most likely developing.
If the discharge from the genitals smells like fish, most likely the man has gardnerellosis. The same pathogen causes a disease in women called bacterial vaginosis. But these are very rare cases; in women the disease occurs much more often. Gardnerella is an opportunistic flora. It multiplies when the body is exposed to certain factors. Factors for the development of gardnerellosis:
- promiscuity
- tight synthetic underwear (made from non-natural materials)
- long courses of antibacterial drugs or immunosuppressants
- condoms with spermicide
- intestinal dysbiosis
- inflammation of the genitourinary organs
- decreased immunity
Discharge with an odor in men can be caused by balanoposthitis or balanitis. These are inflammatory pathologies. There will also be redness, itching and pain in the penis, and ulcers and wrinkling can be seen on the glans.
Prevention of discharge in men
There are no vaccinations or lasting immunity against diseases that cause pathological discharge from the urethra. Once you get sick, you can get the disease again. There is also a risk of the disease becoming chronic, which occurs with regular relapses. To maintain health, there is only one way out - compliance with preventive measures.
These include:
- protection from casual relationships, using a condom, which protects 98% from sexually transmitted infections;
- regular sex life with a trusted partner;
- compliance with personal hygiene standards - daily washing of the penis while retracting the foreskin, changing underwear daily;
- do not overcool;
- treat colds and other infectious diseases in a timely manner;
- regularly visit a doctor for a preventive examination, since some diseases can hardly be detected for a long time, becoming chronic, leading to irreversible changes;
- do not abuse alcohol.
To these measures you can add strengthening the immune system in all ways - hardening, gymnastics, proper nutrition, giving up bad habits, a positive attitude and the absence of prolonged stress.
Sperm
Sperm is a secretion containing many sperm cells (spermatozoa). Sperm is released during ejaculation, that is, at the moment of peak pleasure during sexual intercourse of a different nature. Also, in a dream, men and boys sometimes have wet dreams, then sperm is also released from the penis.
Wet dreams occur mainly during puberty. This is 2-5 cases per month. But with changes in the balance of hormones, there may be wet dreams even several times a week. If sperm flows out of the penis at a time other than orgasm, it is called “spermatorrhoea.” This is a disease caused by impaired muscle tone in the vas deferens. This mainly happens with diseases of the brain or chronic inflammation in the ducts.
Associated symptoms
In the presence of diseases that are characterized by white discharge, their symptoms may have a pronounced clinical picture.
Diseases may be accompanied by itching, burning during sexual intercourse or urination (candidiasis, ureaplasmosis, mycoplasmosis, trichomoniasis), impaired urination (prostatitis), and decreased erectile function.
Sometimes symptoms do not always appear, which contributes to later detection of the disease (chlamydia).
In any case, it is necessary to conduct an examination if white discharge:
abundant;- quite scarce, but appear regularly;
- accompanied by pain, burning, itching or other symptoms;
- general weakness appears;
- an unpleasant or specific odor appears;
- the color of secretion changes;
- urinary problems occur;
- Erectile function decreases.
Signs of diseases may not always appear immediately, or may not have a pronounced manifestation at all, so preventive measures should be carried out regularly (at least once a year) to detect a possible disease.
Video: “White coating on the penis”