Duodenal ulcer - symptoms and treatment
Mandatory measures in the treatment of gastric and duodenal ulcers include:
- following a gentle diet (mechanical and chemical sparing);
- exclusion of such factors of aggression as smoking, alcohol;
- reducing the dose or limiting the intake of certain medications (NSAIDs).
Drug treatment
Drug treatment is aimed at reducing the level of hydrochloric acid, protecting and increasing the regeneration of the duodenal mucosa. To reduce acidity, proton pump inhibitors (PPIs) are used as the “gold” standard of treatment and H2-histamine blockers.[6] To increase the protective properties of the mucous membrane, coating agents and antacids are used. To increase mucosal regeneration, bismuth and sucralfate preparations are used. If Helicobacter pylori infection is present, first-line or subsequent line eradication therapy is performed.[6] To a lesser extent they are used:
- drugs that regulate the motor-evacuation function of the stomach and intestines - prescribed for peptic ulcer disease combined with reflux and insufficiency of the pyloric sphincter;
- psychotropic drugs - used to relieve depression and stress factors when the disease lasts a very long time and a psychosomatic component is added.
In case of complications, endoscopic or surgical treatment methods are used.
Surgery
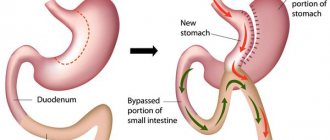
Surgical methods are limited to the treatment of complications such as:
- perforation - the ulcer is sutured or the damaged area of the intestine and stomach is removed with anastomosis;
- penetration—damaged tissue and part of the intestine are removed with anastomosis;
- cicatricial stenosis - resection (partial removal) with anastomosis is performed.
Endoscopic methods primarily include endoscopic hemostasis. This method allows, in most cases, to stop bleeding from an ulcer and prevent its relapse (if the bleeding has stopped).[4] In case of cicatricial stenosis and narrowing of the duodenal lumen, stenting can sometimes be used (if abdominal surgery is contraindicated).
In general, the course of drug treatment for exacerbation of a peptic ulcer or for a newly diagnosed ulcer lasts 1-2 months. Surgical and endoscopic methods are resorted to only when relevant complications develop.
Emergency help during a seizure
Emergency care is provided for complications of a peptic ulcer (bleeding, perforation, stenosis of the duodenal lumen). If these complications develop, you must contact the clinic for a consultation with a surgeon. If there is severe pain, a drop in blood pressure, weakness and other signs of internal bleeding, you must call an ambulance to provide emergency medical care.
To reduce pain, alginates and antacids and/or fast-acting drugs from the group of proton pump inhibitors (PPIs) - rabeprazole - are used as emergency medications.
Diet for peptic ulcers
During the period of exacerbation of duodenal ulcer, a gentle diet with pureed cooking is used. The diet is based on the following principles:
• Mechanical sparing is ensured by choosing food products with a low content of coarse fiber, short stay of food in the stomach and special culinary processing of products (stewing, steaming, grinding food to a puree consistency).
• Chemical sparing is based on increasing the content of fats of plant origin and proteins of animal origin (cottage cheese, cheese, eggs, boiled meat and fish) against the background of the physiological norm of carbohydrates, vitamins, microelements, since fats inhibit gastric secretion, and proteins inactivate hydrochloric acid.
• Thermal sparing is achieved by excluding too cold and hot foods, which injure the gastric mucosa; the optimal temperature for hot foods is +30-40 °C.
• Limiting the volume of food taken at the same time in order to prevent overstretching of the stomach: food is taken 5-6 times a day and in small portions. Eating should correspond to the rhythm of gastric secretion and should be carried out at intervals of 3.5-4.5 hours.
Avoid foods that greatly increase the production of hydrochloric acid by the stomach. Such as: salty seasonings, strong meat, fish or vegetable broths, brown bread, soft bread and pastries, carbonated drinks, strong tea, coffee.
We recommend products that have a medium level of stimulation of hydrochloric acid production: boiled meat, fish, most berries and fruits, and a weak level: soft-boiled eggs, white crackers or dried bread (made from fine flour), cereals, sweet fruits and vegetables.
In a gentle diet with pureed food, the range of dishes includes:
• unleavened cottage cheese, mild and low-fat cheese, pureed;
• pureed soups from prefabricated vegetables (except for cabbage soup and borscht), vegetable and cereal soups, milk cereal soups, with noodles or chopped pasta;
• boiled pureed vegetables - zucchini, cauliflower and Brussels sprouts, tomatoes, carrots, beets (the obligatory exception of white cabbage, turnips, radishes, radishes and legumes, which are rich in plant fibers and essential oils);
• ripe fruits and sweet berries (after heat treatment);
• compotes with pureed dried fruits;
• dried wheat bread.
Dishes are steamed, boiled, boiled until soft, pureed, chopped, and served warm.
The recommended dishes for a gentle diet with unprocessed food are the same as for the option described above. Dishes are steamed, boiled, crushed until soft, but not crushed, served warm 5-6 times a day.
During the period of remission, it is recommended to adhere to the basic principles of a healthy diet. This excludes strong meat and fish broths, mushroom broth, spices, spicy dishes, pickled and smoked foods, which have an irritating effect on the mucous membrane and can increase the formation of hydrochloric acid in the stomach. Limits on pastries, pies, pancakes, coffee, mineral waters and drinks containing large quantities of carbon dioxide. Long-term (more than 10-15 minutes) use of chewing gum is harmful.
Physiotherapy and therapeutic exercises for peptic ulcers
The effectiveness of physiotherapy methods for duodenal ulcers has not been proven, as well as therapeutic exercises. Therefore, these methods are not used in the treatment of peptic ulcer.
Peptic ulcer 12p. guts
The main complications of a duodenal ulcer are penetration, perforation, bleeding and narrowing of the intestinal lumen. Ulcerative bleeding occurs when the pathological process affects the vessels of the gastric wall. Bleeding can be hidden and manifested only by increasing anemia, or it can be pronounced, blood can be found in vomit and appear during bowel movements (black or bloody stool). In some cases, bleeding can be stopped during an endoscopic examination, when the source of bleeding can sometimes be cauterized. If the ulcer is deep and the bleeding is profuse, surgical treatment is prescribed; in other cases, it is treated conservatively, correcting iron deficiency. For ulcer bleeding, patients are prescribed strict fasting and parenteral nutrition.
Perforation of a duodenal ulcer (usually the anterior wall) leads to penetration of its contents into the abdominal cavity and inflammation of the peritoneum - peritonitis. When the intestinal wall is perforated, a sharp cutting-stabbing pain in the epigastrium usually occurs, which quickly becomes diffuse and intensifies with a change in body position and deep breathing. Symptoms of peritoneal irritation (Shchetkin-Blumberg) are determined - when pressing on the abdominal wall and then suddenly releasing it, the pain intensifies. Peritonitis is accompanied by hyperthermia. This is an emergency condition that, without proper medical care, leads to shock and death. Perforation of an ulcer is an indication for urgent surgical intervention.
Penetration of an ulcer is a deep defect that affects the intestinal wall with penetration into adjacent organs (liver or pancreas). It manifests itself as intense stabbing pain, which can be localized in the right or left hypochondrium, radiating to the back depending on the location of the penetration. When changing position, the pain intensifies. Depending on the severity, treatment is conservative; if there is no result, it is surgical.
Duodenal stenosis occurs when there is severe swelling of the ulcerated mucosa or the formation of a scar. When the lumen narrows, obstruction (complete or partial) of the duodenum occurs. It is often characterized by repeated vomiting. The vomit contains food taken long before the attack. Symptoms also include heaviness in the stomach (fullness), lack of stool, and bloating. Regular vomiting contributes to weight loss and metabolic disorders associated with nutritional deficiencies. Most often, conservative treatment leads to a reduction in swelling of the walls and expansion of the lumen, but with severe scar changes, the stenosis can become permanent and require surgical intervention.
Publications in the media
Localization • Most duodenal ulcers are located in its initial part (in the bulb). Approximately 5% of ulcers are located postbulbar. The frequency of ulcers is the same on both the anterior and posterior walls.
Clinical manifestations • Pain is the predominant symptom in 75% of patients. Pain occurs 1.5–3 hours after eating (late), on an empty stomach (hungry) and at night (night). Subjectively, pain is perceived as a burning sensation in the epigastric region. Eating improves the condition (“seized pain”) • Vomiting at the height of pain brings relief (reduction of pain) • Vague dyspeptic complaints - belching, heartburn (early and most common manifestation), bloating, food intolerance • Frequent constipation • Pain is determined by palpation in the epigastric region, sometimes some resistance of the abdominal muscles • Asthenovegetative syndrome • Characterized by periods of remission and exacerbation, the latter lasting several weeks. There is a seasonality of the disease (spring and autumn).
Laboratory tests • Analysis of peripheral blood in uncomplicated cases - unchanged • Analysis of feces for occult blood - Gregersen's reaction. A positive reaction can serve as one of the indirect signs of exacerbation of the process • The level of serum gastrin should be determined in patients with recurrent ulcers, in case of failure of conservative treatment and in cases of suspected endocrine disorders (for example, Zollinger-Ellison syndrome). The normal level of serum gastrin is less than 200 pg/ml.
Special studies
• Detection of H. pylori - see Chronic gastritis.
• Study of gastric secretion - increasing the pH of gastric juice on an empty stomach, with the use of specific irritants (cabbage broth, histamine), increasing the content of pepsin (1.5-2 times compared to the norm).
• X-ray examination with barium suspension; for greater accuracy, use the double contrast method - barium suspension + air •• Direct signs ••• "niche" symptom with radial convergence of folds ••• It is necessary to note the duration of evacuation of barium suspension from the stomach to determine the degree of stenosis (up to 6 hours, 6– 24 hours, more than 24 hours) ••• Typical deformation of the bulb - may complicate the interpretation of radiographs during the period of relapse of the disease •• Indirect signs ••• Pyloric spasm ••• Dyskinesia of the duodenal bulb ••• Jaggedness of the contours of the mucous membrane of the bulb ••• Hypersecretion stomach • Endoscopic examination is the most reliable method for diagnosing peptic ulcer disease; indicated for patients with a typical clinical picture, when fluoroscopy does not reveal a duodenal ulcer (accuracy >95%); allows you to detect a picture of type B gastritis, which often accompanies this type of ulcer • Ultrasound allows you to determine the fluid in the stomach cavity, differentiate the disease from chronic cholecystitis and cholelithiasis.
Concomitant pathology • Familial polyendocrine adenomatosis type I (SPEA I) is often accompanied by the development of gastrin-secreting tumors with the formation of ulcers • Liver cirrhosis and chronic renal failure are often complicated by duodenal ulcers • Zollinger-Ellison syndrome • Lesions of the gastrointestinal tract - chronic cholecystitis (25.6%), reactive pancreatitis, etc.
ICD-10. K26 Duodenal ulcer.