HSG stands for hysterosalpingography . This is a procedure in the field of gynecology, which is used in infertility patients to study the patency of the fallopian tubes.
- Methods for determining pipe patency
- Types of procedure
- Progress of the operation
- Pain during HSG
- Contraindications
- Preparation
- results
- Consequences
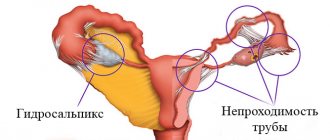
The fallopian tubes are canals that are 10 centimeters long and only 0.1 to 1 cm in diameter. They begin in the uterus and “strive” to the ovaries. Along them, the egg, which has merged with the sperm, moves into the uterine cavity. If the tubes are obstructed, then conception cannot take place, making natural pregnancy impossible.
The pipes may be partially obstructed. Then an ectopic pregnancy occurs. This means that the fertilized egg cannot freely pass through the tube and is attached to it, beginning to develop there. This condition requires urgent surgery because it threatens the health and life of the patient.
Methods for determining pipe patency
Current methods for determining the patency of the fallopian tubes are:
- Diagnostic laparoscopy
- Fertiloscopy and transvaginal hydrolaparoscopy
- Ultrasound hydrosonography, echohysterosalpingoscopy
- GHA
Hysterosalpingoscopy is carried out by introducing contrast and performing X-ray, and then analyzing the information by a doctor. Most contrast agents contain iodine. They have a low toxic effect when interacting with the radiation of an X-ray machine.
Informativeness of hysterosalpingography in comparison with other research methods
The sensitivity and specificity of research methods (hysterosalpingography (HSG of tubes, HSG of fallopian tubes) and hysterosalpingosonography) are approximately the same and amount to about 80% according to data from a number of foreign authors and our own research results. However, their information content, of course, is not 100% - which is recorded when using laparoscopy.
Thus, both methods are highly sensitive and, if the result is negative, can definitely exclude the disease. That is, in the case of patent fallopian tubes, the information content of the methods is quite high and practically gives a complete answer to the question posed when diagnosing infertility.
If the result is positive, the probability of tubal obstruction is above 70%. That is, if during research we receive results indicating that the tubes are not “ideal,” then most likely there is a “tubal-peritoneal factor of infertility.”
The presence of false-negative results is most likely associated with spasm of the isthmic section of the fallopian tubes, or with a violation of the technique of performing this study. The specificity of the methods increases significantly and reaches 90% in the case of bilateral distal occlusion of the fallopian tubes (that is, in the presence of hydrosalpinxes).
The HSG technique allows us to assume the presence of peritubar adhesions based on the use of a number of diagnostic criteria:
- “atypical tube location” is a symptom in which the fallopian tube is located not horizontally, but vertically;
- pronounced “tortuosity” of the fallopian tube – “convulation”;
- the presence of a “corolla” effect around the fallopian tube – “double contour”;
- the absence of spreading of the contrast agent as the fallopian tube exits and its accumulation in the fimbrial region - “loculation”.
Arrow – accumulation of contrast agent. Symptom of "loculation"
Types of procedure
- USGSS (ultrasound HSG/sonographic)
This is an ultrasound diagnosis in which saline, furatsilin or glucose solution is injected into the uterus. This method is considered low-informative. In addition, only one specialist can perform an examination at a time. No pictures are taken, so other doctors cannot see the picture.
Advantages of USGS: speed, minimal pain, minimal invasiveness, no radiation exposure.
- X-ray GSGGGSG
Verografin, Urotrast or Urografin is injected into the patient's uterus through a catheter, and then a series of x-rays are taken. Advantages of the procedure: the ability to be studied by other specialists, the ability to compare images over time, unlike USGSS.
Disadvantages of the method: irradiation of the woman, the likelihood of exacerbation of inflammation in the appendages, pain during and after X-ray X-ray HSG. Although the radiation is not so strong, a woman is not advised to conceive a child during this menstrual cycle, because it may have developmental abnormalities.
Preparing for an ultrasound of the fallopian tubes
A regular ultrasound does not require extensive preparation. To improve the quality of the study, it is recommended to exclude gas-forming foods from the diet. If the diagnosis is carried out using an external sensor, then an hour before the procedure it is recommended to drink a liter of water to fill the bladder.
Ultrasound hysterosalpingography requires serious preparation. First of all, it is necessary to undergo a number of tests before the study:
- Flora smear from the vagina and cervical canal.
- Oncocytology of the cervix.
- Blood tests for HIV, syphilis, hepatitis.
- Conventional ultrasound of the pelvic organs.
Although HSG is a diagnostic procedure, it can be equated in danger to a minor surgical intervention, as the catheter penetrates the uterine cavity through the cervix. Because of this, the risk of infection of the uterus increases, so there should be no pathogenic microorganisms in the vagina and cervix. If the flora is disturbed, you will have to first restore it and then go for an HSG.
Ultrasound hysterosalpingography is not performed during or on the eve of menstruation; the procedure can be performed from 6 to 22 days of the menstrual cycle.
As preparation, doctors prescribe an antispasmodic, for example, drotaverine. This is necessary in order to avoid spasm of the oviducts during the procedure.
It is also recommended to start following a diet 2-3 days before the examination, eliminating gas-forming foods from the diet. Excess gases in the intestines create interference, which is why the pelvic organs are less visualized and the information content of ultrasound is reduced.
Progress of the operation
First, the patient is examined by a gynecologist using mirrors, then local anesthesia is performed. Then they take a cannula (this is a small tube) and insert it into the patient’s cervix. The specialist takes a syringe and injects a contrast agent through the cannula, which blocks the X-ray radiation.
The contrast fills the uterus and enters the tubes. The doctor takes from 4 to 6 x-rays. Then the cannula is removed from the neck. Over time, the contrast agent is absorbed into the blood and removed naturally.
Hysterosalpingography: how is it performed?
Anesthesia is not required during the procedure. The procedure is painless; there may be a slight feeling of heaviness in the lower abdomen when a contrast agent is administered. When using X-rays, the radiation is minimal.
Before taking the picture, the doctor inserts a special tube into the uterus through which the solution is delivered. The image makes it possible to assess the condition of the uterus and the location of the fallopian tubes. The procedure takes on average 35-45 minutes.
In some cases, there may be bleeding for a week. Then the doctor may recommend medications to prevent inflammation. You can learn more about how hysterosalpingography is done from your doctor.
Pain during HSG
Many people are interested in the question of whether it is painful or not to perform HSG of the fallopian tubes. During the procedure, pain is possible, so the doctor administers lidocaine in advance. This is a drug that has a local anesthetic effect. That is, there will be no general anesthesia.
After HSG, there may be aching pain in the lower abdomen for 2-4 days. The pain may be mild, moderate or severe. It depends on the patient’s pain threshold, the condition of her appendages and her uterus. In some cases, even with good local anesthesia, patients feel pain when contrast is injected before taking pictures. After the procedure, their stomach also hurts.
In some cases, abdominal pain may be tolerable and does not cause much discomfort. Moreover, these sensations are stronger when the liquid is administered through a syringe and cannula, and half an hour after the procedure the pain disappears.
Where to do an ultrasound of the fallopian tubes
You can undergo an HSG ultrasound of the fallopian tubes in the MedCenterService clinic network. Medical centers have many advantages:
- High information content and diagnostic accuracy. This is possible thanks to the latest generation equipment.
- Individual approach and competent examination. The clinic employs doctors with extensive experience.
- Fast examination without queues. Appointments are by appointment, at a time convenient for the patient.
- The result is given to you immediately. The patient has the opportunity to independently review the study protocol.
After the procedure, you can immediately consult with a gynecologist to interpret the results and receive recommendations for further actions.
Contraindications
Doctors (and patients themselves) definitely need to know when not to do hysterosalpingography, that is, GHA.
- pregnancy
Before the HSG, the patient is given a pregnancy test to be sure that a fetus is not developing in her body.
- allergy to contrast
The patient may have an allergic reaction to medications that contain iodine. Other active substances with unstable electrons are more toxic and can significantly harm humans.
- any inflammation of the cervix, vagina or appendages
Chronic infection may become active after the procedure, which is explained by the effect of the contrast agent. For this reason, an examination by a gynecologist and a vaginal smear are prescribed. Tests will show how healthy the flora is in the patient’s vagina and whether there is inflammation.
Doctor's opinion
The diagnostic value of hysterosalpingography for determining the causes of infertility is high.
You can immediately examine the uterine cavity and oviducts. Visually see structural anomalies (bicornuate, saddle-shaped), pathologies (polyps, myomatous nodes, synechiae), diseases (hydrosalpinx), adhesions, bends. Determine the level of obstruction and the possibility of prompt elimination. — Malakhova Victoria Yurievna Reproductologist, obstetrician-gynecologist
Contraindications to the procedure:
- acute infectious diseases;
- inflammatory processes of the organs of the reproductive system;
- varicose veins, accompanied by the formation of blood clots;
- menstruation;
- period of childbearing and breastfeeding;
- malignant tumors of the cervix;
- dysfunction of the thyroid gland;
- allergy to iodine;
- renal, hepatic and cardiovascular failure.
If there are contraindications, the doctor will suggest other, safer examination methods.
Preparation
You should know the rules for preparing for HSG, and on what day the procedure is carried out. The preparation is quite simple:
- do not have sex 2 days before HSG
- 7 days before the procedure, stop using intimate hygiene products and douching
- 7 days before HSG, do not use suppositories, vaginal suppositories or tablets, or tampons (switch to pads)
HSG of the fallopian tubes is done after the critical days (within 14 days from the end). The reason is that the uterine mucosa is thin during this period, does not block the entrance to the tubes, and the woman cannot yet be pregnant.
After HSG
The first two to three days after the procedure, there may be mucous or scanty spotting from the vagina, and there may be mild pain or discomfort in the lower abdomen. They usually go away with regular painkillers. After the procedure, due to stress, your period may be delayed by 2-3 days.
Two to three days after the procedure, douching, the use of suppositories and sprays, intimate hygiene products, sexual intercourse, bathing and visiting the sauna are not recommended.
After hysterosalpingography, there is an increase in the likelihood of conception, since a contrast agent, especially with an oil base, activates the functioning of the uterine glands and increases the activity of the endometrium.
This method provides a lot of information, but is not the main one in diagnosis. GHA is used to clarify and supplement previously conducted studies; the accuracy of the study reaches 80-85%.
results
X-rays, if there are no adhesions, show the uterus, which has fluid, tubes and contrast that leaks into the abdominal cavity. The image allows the specialist to assess how passable the patient’s fallopian tubes are.
Sometimes the contrast “slows down” in a certain section of the pipe, which indicates an obstruction. HSG also detects adhesions in the uterus, adhesions outside the tube, hydrosalpinx, fibroids and polyps, if present. If HSG is performed successfully, the results may still be inaccurate.
The effectiveness of the procedure is 65 percent, and the specificity is 80 percent. The last indicator means identifying a specific disease from among the possible ones. To check the uterine cavity, patients also undergo hysteroscopy.
Indications
This diagnostic method is chosen by gynecologists for patients with suspicion and to identify various diseases and pathological changes in the uterine cavity.
Tubal obstruction
Pathology is one of the causes of infertility and occurs if there are congenital or acquired ailments in the anatomy of the tubes (after surgery or functional disorders).
Isthmic-cervical insufficiency - expansion of the cervical canal and its internal os to 5-7 mm
Premature pathological dilation of the cervix, causing spontaneous abortion or premature birth. ICI occurs with congenital malformations of the uterus, injuries received during childbirth, after surgery, with hormonal disorders, etc.
Anomalies of the development of the uterus and appendages
Anomalies and malformations of the uterus include any changes in shape, location, size, etc. Their presence leads to disruptions in the reproductive system and various functional disorders. Without treatment, problems can lead to infertility, pregnancy complications, and miscarriage. Most often, illnesses occur without symptoms, so a high-quality diagnosis is needed.
Submucous fibroids or synechiae (adhesions in the uterine cavity)
Myomas, synechiae and other intrauterine pathologies are often diagnosed as a whole group in one patient (almost all age groups). Pathologies have similar symptoms and require an integrated approach to diagnosis and treatment.
Adenomyosis, endometrioid cancer, polyps, genital tuberculosis
Various lesions of the uterine mucosa are usually associated with infectious or viral diseases, hormonal disorders, inflammation, etc. and serve as signals of serious problems in the female body. Polyps arise and develop against the background of pathologies such as cervicitis or cervical erosion. Adenomyosis affects other tissues of the uterus. Genital tuberculosis leads to cycle disorders, intoxication, infertility, etc.
Consequences
HSG is a safe procedure. Basically there are no complications or consequences. In rare cases, patients develop a severe allergy to the injected contrast. It is necessary to carefully check for allergies those who are prone to allergic manifestations and those who have bronchial asthma.
In rare cases, the procedure is unsuccessful. This happens if the doctor does not have enough experience. It can puncture the uterus, causing bleeding.
If there is a chronic infection, as noted above, a resumption of the process and symptoms may occur. Inflammation of the appendages and endometritis are likely, but such cases are rare.