The term “Early miscarriage” refers to spontaneous abortion that occurs in the first 6-8 weeks of pregnancy. It can occur before 20 weeks of pregnancy for reasons related to the natural conditions of the fair sex. According to statistics, the logical outcome of every fifth pregnancy is a miscarriage. However, quite often a woman at the time her body rejects the fetus does not even know that she was pregnant.
In addition, an interesting pattern has been revealed: artificially induced pregnancies end in miscarriage more often than natural ones. For example, in vitro fertilization, unfortunately, does not always lead to a successful pregnancy and the birth of a baby at term.
How often do miscarriages happen?
According to statistics, 13-17% of all pregnancies end this way. However, the individual risk may be higher. For example, one miscarriage experienced will not change the situation, but if there have already been two in a row, then the risk increases to 36-38%, well, and three such episodes increase the probability to almost 40%.
Women themselves do not always realize that a miscarriage has occurred to them, because if the pregnancy is terminated at a very early stage, it simply looks like a slight delay in menstruation. By the way, up to 80% of miscarriages occur before 12 weeks. If pregnancy continues longer, the risk of spontaneous abortion is significantly reduced.
What is the corpus luteum?
VT occurs in the ovary at the site of an ovulated follicle: VT is a temporary hormonal organ. VT is responsible for the production of progesterone, the main hormone of pregnancy; on ultrasound, VT looks like a round formation of heterogeneous soft tissue. It is impossible to determine progesterone deficiency from the image obtained by ultrasound, however, clinical and laboratory studies make it possible to diagnose this deficiency.
As pregnancy progresses, cysts can sometimes form in the VT. The reason cysts form is that the corpus luteum produces small amounts of fluid. Some of this fluid is resorbed by the blood vessels of the ovary, and some remains inside the ovary, forming vesicles, which form cysts (from the Greek root “cyst” - “bubble”). By 10-15 weeks of pregnancy, the VT cyst completely resolves, as the VT itself decreases. VT cysts do not pose a threat to pregnancy, but sometimes a woman may feel pain in the lower abdomen, mistaking it for a symptom of an impending miscarriage.
For what reasons does a miscarriage occur?
There are many reasons that can lead to a miscarriage. But there are two main ones: this is a problem on the part of the fetus itself and pathology in the mother’s body. Genetic abnormalities in the formed embryo are the main cause of termination of pregnancy in the early stages. With the help of miscarriage, nature often “rejects” embryos, although sometimes it “misses” defective ones.
As for problems on the mother’s side, the most significant are:
- anatomical abnormalities of the uterus, gynecological diseases (uterine fibroids, endometriosis) and inflammatory diseases after artificial termination of pregnancy (chronic endometritis);
- hormonal disorders: lack of progesterone production (a hormone that supports pregnancy), diabetes, malfunction of the thyroid gland (hypothyroidism), adrenal gland diseases, hyperandrogenism (increased levels of male sex hormones). In such cases, appropriate medication adjustment and lifestyle changes can be applied. In cases where the expectant mother develops isthmic-cervical insufficiency, in which the length of the cervix shortens, in order to maintain the pregnancy, a silicone ring (obstetric pessary) is placed on the cervix or sutures are applied, which are removed only at the end of the 36th week;
- immune disorders and disorders in the hemostasis system (tendency to increased thrombosis). Antiphospholipid syndrome, leading to the formation of blood clots in the blood vessels of the placenta, can prevent pregnancy. Timely administration of blood thinning medications helps to carry a child to term in the vast majority of cases;
- infections (herpes, chlamydia, rubella and others). It is better to be examined and treated for possible infections in yourself and your sexual partner 2-3 months before conception, and get vaccinated against rubella (if you have not been sick);
- non-infectious diseases (anemia, autoimmune diseases, bronchial asthma). These reasons often lead not to miscarriages, but to premature birth.
Is it true that the number of miscarriages increases in the spring?
I have not seen any statistics indicating such a pattern. But of the total number of premature births per year, 28.8% occur in spring, 26.5% in winter, 23.3% in summer, and 21.4% in autumn. This is due to an increase in the absolute number of births in the spring.
Should pregnant women in the early stages avoid air travel, intimacy, negative emotions, moderate exercise, and riding on public transport?
If the expectant mother does not have any special problems with the health and course of pregnancy, then all of the above is quite acceptable. Pregnancy is not a disease, so normal everyday stress is not scary for mother and baby. On the contrary, moderate physical activity in the gym or swimming pool will even be beneficial. But, of course, without fanaticism.
Miscarriage - risk factors during pregnancy
Prognosis factors associated with the course of pregnancy that have a significant impact on the risk of miscarriage:
- Location of the gestational follicle
. Follicles located above the internal ostium are more prone to miscarriage than those located below. The location of the gestational follicle can be assessed using ultrasound; - Fetal heart function
. Decreased fetal heart function – bradycardia – is an unfavorable prognostic symptom; - Bleeding
. An unfavorable prognosis factor is bleeding lasting 4 days or more; - Human chorionic gonadotropin (beta-hCG) level.
Lack of growth or a decrease in the level of this hormone is an unfavorable prognosis factor, indicating the presence of a dead fetus. Under normal conditions, the concentration of human chorionic gonadotropin increases every 48 hours by approximately 66%. This hormone is produced by the embryo, and its greatest secretion occurs in the 10th week of pregnancy. Slower growth indicates fetal abnormalities.
Symptoms of uterine tone
How to recognize a threat of miscarriage? What symptoms indicate this? Uterine hypertonicity – is it dangerous?
A miscarriage may be preceded by spotting that turns into bleeding, as well as increasing pain in the abdomen and lower back. There may be other symptoms (vomiting, for example), but pain and blood are the main signs. However, minor bleeding does not always indicate a threat of miscarriage (nevertheless, it is better to go to the hospital or call an ambulance). At the same time, periodically appearing nagging pain in the abdomen and lower back is also not always a pathology. A danger signal is when such pain does not go away after rest, but intensifies over time.
As for uterine hypertonicity, which we diagnose every second expectant mother and, on this basis, offer her hospitalization, this is often a case of overdiagnosis. The uterus is a muscular organ and, like all muscles, cannot help but contract.
Another pregnancy after a miscarriage
If spontaneous abortion occurs in the case of the first pregnancy, doctors usually do not prescribe any specialized examinations. Efforts for another pregnancy can begin at the next ovulation, 2-6 weeks after the miscarriage.
If during a miscarriage it becomes necessary to curettage the uterus, the doctor will tell you when it will be possible to return to trying to conceive a child and to sexual relations in general. The chances of a healthy pregnancy after one miscarriage are estimated at 80-87%, and a second at 72-82%.
Prevention of recurrent miscarriages
Can miscarriage be prevented with treatment or lifestyle changes?
It all depends on the reason for which the threat of termination of pregnancy arose. It is impossible to prevent so-called sporadic (or accidental) miscarriages, the main causes of which are genetic damage in the fetus’ body and severe infections suffered by the pregnant woman. If the pregnancy must be terminated, then so be it. And there is not a single medicine that could prevent this. A “good” pregnancy ends in childbirth.
It's the same with lifestyle. A pregnant woman can lie as long as she wants without moving, but if the fetus has severe pathologies that can later affect the child’s quality of life, a miscarriage cannot be avoided.
Another thing is recurrent miscarriage, which occurs due to some kind of disorder in the mother’s body. Some reasons (alas, not all) can be influenced. But you should start preventing recurrent miscarriages not when the threat of miscarriage is already obvious, but it is better to contact a medical institution, a miscarriage clinic, or a fertility specialist before conception. The doctor will prescribe the necessary tests and, based on their results, will carry out preconception preparation, that is, create optimal conditions for the onset of pregnancy and its progression to full term.
If you still have questions, you can ask your obstetrician-gynecologist online in the Doctis application.
How to maintain pregnancy?
A woman diagnosed with recurrent miscarriage knows that she has a problem with pregnancy. Therefore, she must prepare differently for the next pregnancy - more carefully and for a long time.
First of all, you definitely need to take a break between pregnancies for at least six months or a year in order to understand the reasons that force the body to get rid of the fetus. In order to find the reasons, a series of tests should be done, not only for her, but also for her partner.
- A man should be tested to determine the degree of sperm DNA fragmentation. This analysis is not included in the standard spermogram. If the degree of sperm DNA fragmentation is higher than normal, this means that there is too high a probability that the egg will be fertilized by a sperm with “damaged” DNA and the embryo will not be viable.
- A blood test, including hormone tests, will show the presence of hormonal imbalance, problems of the circulatory system and the presence of infection or inflammation, disease.
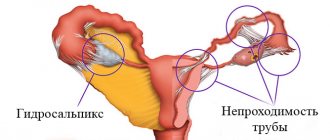
- Ultrasound and, possibly, more detailed studies of the pelvic organs - ovaries, fallopian tubes, uterine cavity.
After receiving the tests, it is also advisable to contact a genetics specialist for advice.
If the analysis shows a high degree of sperm DNA fragmentation, the man is prescribed antioxidants, since it is antioxidants that protect DNA from damage by free radicals. Studies have shown the high effectiveness of the antioxidant complex Synergin in protecting the genetic material of men. The course is usually about three months.
A woman will also benefit from this complex, as it will help protect the maturing egg from adverse environmental influences, which can cause mutations in the egg.
If neoplasms or defects of the female reproductive system are detected, surgical intervention may be required. Infectious diseases will need to be cured completely.
It is important to carefully follow the course of treatment prescribed by your doctor and avoid traditional medicine if it is not approved by your doctor. Often, herbal remedies can be especially dangerous due to side effects on the body.
The causes of recurrent miscarriage have been found and treatment has begun. What else can you do to help your body?
You should definitely give up bad habits (drinking alcohol, psychotropic drugs, smoking). Start eating proper and healthy foods, taking vitamin and mineral complexes, including to prepare for pregnancy.
What else is important to remember when the body is already as healthy as possible and pregnancy has occurred?
After pregnancy, a woman who has already suffered several recurrent miscarriages should consult a doctor as soon as possible. If any deviation is noticed, especially around the time of a usual miscarriage, immediately call an ambulance or go to your specialist. Under no circumstances should you hope that this time “everything will work out.”
First of all, you need to think about your health. Stress greatly affects pregnancy. Therefore, despite the fact that a recurrent miscarriage will never become familiar to any woman in the world, there is always the opportunity to try again with the support of modern medicine and the best specialists.
THIS IS NOT AN ADVERTISING. THE MATERIAL WAS PREPARED WITH THE PARTICIPATION OF EXPERTS.
Recommendations for your inner circle
The most important thing is that at any stage a person should feel supported. It is necessary to find ways of communication that are acceptable to him. He should know that he can contact you at any time of the day, and this is convenient and allowed.
Are you having difficulty conceiving or maintaining a pregnancy? ISIDA clinic specialists have everything necessary to help you find the happiness of motherhood. We will be glad to see you among our patients. Any questions? Call 0, +38 and we will be happy to answer them. Or ask your question on our website and we will definitely answer it .
Dealing with destructive thoughts and feelings
Destructive thoughts and feelings that a woman experiences after pregnancy loss can be directed both at herself and at others.
In relation to oneself, a feeling of guilt is formed, a feeling of being inferior, broken, empty, pathetic and even dirty.
In relation to others, a complex of reducing oneself develops, a false impression of condemnation from others, a lack of sympathy and understanding.
To overcome this condition it is necessary:
- communication with friends and acquaintances;
- expressing your emotions and feelings through painting, poetry, letters, journaling;
- forming a support group of people you trust (this could be close friends, relatives, professional psychologists).
It is very important not to ignore or hide these emotions from yourself, but to live through them and let them go. Be patient, give yourself as much time as you need.
When do you need help from a psychologist?
If your condition does not change and you feel that your emotions are going in a vicious circle, increasing depression and indifference, keep in mind that this may be a sign of the formation of a psychological complication known as complicated grief syndrome .
Its signs: anxiety, numbness, fear of children or fixation on another child, similar memories, nightmares .
Like any complication, this syndrome requires immediate intervention from specialists.
Acknowledging and processing loss is an important component of healing. At the same time, ignoring this fact and repressing emotions hinders recovery and can cause behavioral deviation (actions that do not correspond to generally accepted norms of behavior). A psychologist or psychotherapist can quickly help you break the vicious circle and find a constructive way out of the situation.