During pregnancy, as you know, changes occur in the female body. The musculoskeletal system is also changing. Changes are gradually made in the pelvic bones so that in the future a child can be born without problems.
- Female pelvis
- Symphysite: what is it?
- Symptoms
- Causes of symphysiopathy
- Degrees of symphysiopathy
- The effect of symphysitis on pregnancy
- How does a symphysis rupture manifest itself?
- Dangers of symphysitis
- Diagnostics
- Differential diagnosis
- Treatment of symphysitis
- Exercises for pain
- Treatment of symphysiolysis in newborns
Female pelvis
The pelvis is a closed ring, which includes:
- bones
- coccyx
- sacrum
Pelvic bones:
- ischial
- pubic
- iliac
A woman's pelvis supports her internal organs and is also the passageway for the baby from the mother's belly to the outside world at birth. Therefore, thanks to the hormone relaxin, the cartilage and ligaments of this “ring” can become softer and more dynamic. Thanks to this, the baby can pass through the mother's pelvis with relative ease.
Symphysite: what is it?
This pathology is an inflammatory process in the symphysis pubis. It should be noted that this pathology is rarely recorded by doctors. When the mother has not yet given birth, but is only carrying the baby, doctors can talk about symphysiopathy. The essence of the term: an increase in the distance between the bones by more than 5 mm, too much softening of the cartilage. The gap between the pubic bones of a woman who is not expecting a child (not pregnant): 0.2 cm. When a girl turns 18 to 20 years old, this distance can be greater (maximum 0.6 cm), and then the size becomes smaller.
In some cases, during childbirth, the pubic bones diverge (distance from each other), and the symphysis ruptures. In this case, so-called symphysiolysis is diagnosed. Where the bones of the woman giving birth have separated, inflammation may begin, which is called symphysitis.
Symptoms
Typical symptoms:
- shooting or nagging pain in the pubis
- pain that worsens with physical activity; becomes maximum if the hip is moved to the side
- the pain described above radiates to the abdomen, thighs or back
- palpation (palpation by a doctor) reveals pain in the area of the symphysis pubis
- the gait changes to the so-called “duck”, that is, the girl waddles from foot to foot when walking
- pain in intimate relationships
- there is no pain when the patient's body is completely at rest
- in some cases, the process of bowel movement is disrupted
Pregnant women may have slight pain in the pubic area, and this does not indicate pathology. According to statistics, this manifestation occurs in approximately half of women expecting a child. Discomfortable sensations appear when the symphysis softens and the ligaments are stretched to one degree or another. This is clearly felt in the middle and end of the 9th month of pregnancy. If you notice very severe pain that does not allow you to sleep, or does not allow you to do normal movements, you should worry. This may be symphysitis in a pregnant woman.
Symphysitis as an interdisciplinary problem
For citation. Glazunov P.A., Trofimenko I.A., Zhilyaev E.V. Symphysitis as an interdisciplinary problem // RMJ. 2015. No. 25. pp. 1520–1522.
Pain in the pelvic bones can occur for various reasons. Traditionally, already at the stage of collecting anamnesis, the doctor tries to differentiate pain of mechanical and inflammatory types, which is important for diagnosis and further treatment. However, in some cases the process of making a correct diagnosis can be quite difficult. Below we present a clinical observation of a patient with specific complaints and the history of our diagnostic search.
Patient G., 69 years old,
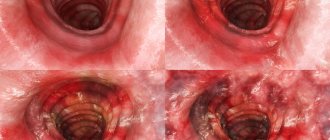
He consulted a rheumatologist with complaints of pain in the area of the pubic symphysis, radiating to the right groin area, aggravated by walking, changing body position in bed, and rising from a lying position. From the anamnesis it is known that he considers himself sick since February 2015 (2 months before treatment), when, a few days after an injury at home (falling from the stairs onto his back), pain appeared in the area of the pubic symphysis, aggravated by walking, with irradiation in the right and sometimes left groin areas. Body temperature – up to 37.8°C. The patient went to one of the clinics in Moscow, where examination revealed leukocytosis of 19.1 × 109/l, an increase in ESR to 50 mm/h, and an increase in the level of C-reactive protein of more than 200 mg/l. In the general urine analysis, leukocyturia – 735–736 per field of view, erythrocytes – 35–36 per field of view, leukocyte esterase +++, total PSA – 0.115 ng/ml. The condition was regarded as an exacerbation of a urinary infection against the background of chronic post-radiation cystitis. The patient was hospitalized, and during parenteral antibacterial therapy (ceftriaxone 2 g/day + amikacin 1.5 g/day), body temperature normalized, the intensity of pain in the pubic area decreased, leukocytosis decreased to 12.0x109/l and ESR to 40 mm/h, decrease in the number of leukocytes and erythrocytes in a general urine test. The patient was discharged to continue treatment as an outpatient. The patient has a history of: 2009 – prostate cancer (Gleason grade 4+5 adenocarcinoma). A radical retropubic resection of the prostate was performed, and radiation therapy (brachytherapy, external radiation therapy) was performed. Subsequently, chronic post-radiation cystitis was diagnosed. In the postoperative period - deformation of the bladder neck, urethral stricture, urinary incontinence. In 2013, transurethral resection of the bladder was performed due to its developed obstruction. After discharge, the patient continued to experience constant pain in the area of the pubic symphysis, the number of leukocytes in the peripheral blood returned to normal, and the ESR remained elevated to 60 mm/h. Computed tomography revealed a moderate widening of the joint space of the symphysis pubis – up to 7 mm. Along the anterior contour of the symphysis pubis there is a compaction of soft tissues without clear contours, measuring about 45 x 35 mm, and the adjacent subcutaneous fat is heavy. Against the background of osteophytes, marginal destruction of the cortical layer of the anterior sections of the pubic bones in the area of the symphysis pubis is determined. In the body of the right ilium there is an osteosclerotic lesion measuring up to 10 mm, with uneven contours. Prostate gland with postoperative changes, in the central part there is a fluid defect, along the edges there are calcifications. The subchondral parts of the acetabulum are sclerotic. Severe calcification and tendinosis are detected along the edge of the iliac crests, in the area of the greater trochanters of the femurs. A tumor (regarded as more likely) or inflammatory process is suspected. On the recommendation of the oncologist, skeletal scintigraphy was performed with Tc-99m-labeled pyrophosphate; no data indicating metastases or arthritis were obtained. The pubic symphysis area was not assessed due to the natural concentration of contrast in the bladder. When examined by a rheumatologist, the condition was of moderate severity due to pain. Lameness on the right leg when walking. On examination, the peripheral joints were unchanged. Palpation of the spinous processes of the vertebrae throughout is painless. There are no restrictions on movements in the cervical spine. The range of motion in the thoracic and lumbar spine cannot be assessed due to increasing pain in the pubic symphysis when attempting to conduct assessment tests. Palpation of the pubic symphysis is painful. Movements in the right hip and knee joints are limited, as the pain in the pubis and right groin area intensifies. The skin in this area is not changed, there is no local hyperemia. The isometric pelvic muscle tension test is positive. For pain relief, the patient was recommended to take NSAIDs, the effect was positive. With additional laboratory examination: procalcitonin <0.5 ng/ml (semi-quantitative method, negative test result), leukocyte count in peripheral blood - 7.6 × 109/l, C-reactive protein - 53.6 mg/l. An MRI of the pelvic bones with contrast is recommended. A few days later, the patient came to the clinic due to acute urinary retention, which resolved on its own after the passage of a dark red “clot.” The patient was examined by a urologist and cystoscopy was performed: closer to the neck of the bladder in the area of the urethrovesical anastomosis at 6 o'clock on the conventional dial, an ulcer-like defect made of fibrin with a diameter of about 2 cm was detected. Areas of bleeding with small fresh blood clots were also found there. The neck of the bladder is narrowed and deformed. The patient was referred for an MRI of the pelvis with contrast (Fig. 1). Along the anterior wall of the formed “pre-bladder” a defect measuring 7×8 mm is determined, communicating with the pubic symphysis widened to 10 mm. Adjacent surfaces of the pubic bones show signs of bone marrow edema. Along the lower edge of the dilated and fluid-filled symphysis pubis, two fistulous tracts are identified, which run at 8 o’clock (length up to 28 mm) and at 4 o’clock (length up to 18 mm) downwards and outwards on both sides of the base of the penis and blindly end in the abductor muscles. In the branches of the ischial bones there are zones of bone marrow edema, in the external obturator and adductor muscles at the symphysis pubis there are zones of inflammatory infiltration (accumulation of a contrast agent is noted). In the cervical section of the bladder there is pronounced swelling of the mucous membrane, along the left side wall of the bladder 6 mm outward from the mouth of the left ureter there is a diverticulum 8x9x12 mm. In the lateral masses of the sacrum, symmetrical, extensive, longitudinally oriented zones of pronounced bone marrow edema are detected. Taking into account MRI data, the condition was assessed as osteomyelitis of the pubic bones with the source of infection in the urinary tract. The patient was hospitalized in a urology hospital, and a cystostomy was installed to reduce pressure in the bladder. Antibacterial therapy was not carried out. After 14 days, clear positive dynamics were observed in the form of a decrease in pain intensity, a slight decrease in ESR and CRP levels. Surgery is planned to restore the tightness of the bladder.
Discussion
Pain in the symphysis pubis can have various causes. Taking into account clinical and laboratory data, a differential diagnosis was made between the following diseases: symphysitis as part of spondyloarthritis, osteitis pubis, tumor lesion of the pubic bones, osteomyelitis of the pubic bones, tuberculous symphysitis. Cases of pain in the area of the pubic symphysis in patients with spondyloarthritis are known, but are rare. However, sometimes pain in the symphysis area is the leading or even the only manifestation of the disease. Isolated symphysitis as a manifestation of spondyloarthritis should be considered primarily due to the high prevalence of spondyloarthritis [1–3]. But if an increase in the level of C-reactive protein, ESR and fever could be associated with spondyloarthritis, then leukocytosis with a band shift, the absence of signs of sacroiliitis on MRI and positive dynamics with the use of antibiotics made us think about alternative diseases. Another disease that is included in the differential diagnosis is osteitis pubis. This is an idiopathic inflammation of the pubic symphysis and surrounding structures. It can develop as a result of various types of movements: rapid acceleration/deceleration, kicking, overload of the adductor muscles or imbalance between the abdominal wall and the strength of the adductor muscles of the thigh, as well as due to avascular necrosis of the pubic symphysis, osteochondritis dissecans. The patient had a history of trauma (a fall at home) that could potentially cause osteitis, but the general inflammatory syndrome observed in the patient is extremely uncharacteristic of osteitis pubis. Despite the oncological history, this version was opposed by fever, lack of involvement of other bone structures, and clinical and laboratory response to antibiotics. On CT, the phenomena of marginal destruction predominated without signs of the formation of new tissue in the symphysis area. Most often, pain in the area of the pubic symphysis is differentiated between osteitis pubis and osteomyelitis. Both conditions are quite rare and are often diagnosed late [4]. Osteomyelitis of the pubic symphysis can develop as a complication of open or laparoscopic operations, as a result of irradiation of the pelvic bones, surgical interventions, penetrating trauma (gunshot wound), sacral injury or epidural anesthesia. Both diseases may have similar clinical manifestations, making diagnosis difficult. The following imaging methods are used: X-ray, MRI, CT, scintigraphy [5]. The most accurate method is a biopsy of the affected area [6, 7]. Osteomyelitis can be hematogenous or as a result of direct spread of infection to the bone from adjacent tissues. The observed x-ray pattern (marginal bone damage) suggests local spread. The location of the damaged areas suggests that the source of infection of the bone was most likely the contents of the bladder. Thus, the sequence of events in the development of the disease can be represented as follows: transurethral resection of the bladder – bladder leakage in the postoperative period – urinary fistula through the symphysis into the prepubic tissue – osteomyelitis. The management plan for such a patient should include stopping the flow of urine into the symphysis area and antibiotic therapy. Of particular interest are the identified changes in the lateral masses of the sacrum (Fig. 2). These zones of restructuring, sometimes called pseudofractures, when symmetrically located in the lateral areas of the sacrum (a pattern previously referred to as Milkman syndrome), should be considered a pathognomonic manifestation of osteomalacia. Osteomalacia may cause pain in the pubic area, but does not explain hyperthermia, inflammatory changes in the blood and destructive changes in the bones. This made it possible to consider it in this case as a concomitant condition.
Osteomalacia is a diffuse skeletal disease caused by impaired bone mineralization. Its causes may be calcium deficiency (most often), phosphorus deficiency (phosphate diabetes in children and oncogenic osteomalacia in adults due to high production of phosphouretic factors), blocking the formation of calcium pyrophosphate crystals in the bones by exogenous substances (bisphosphonate, aluminum osteomalacia). In the case under discussion, all reasons except the first can be fairly confidently excluded. The most common causes of calcium deficiency are vitamin D deficiency, impaired calcitriol formation, malabsorption, and impaired reabsorption of calcium in the renal tubules. The patient was found to have a significant decrease in the measured vitamin D metabolite calcidiol (25-hydroxycholecalciferol) - 6 ng/ml (normal - 30-60 ng/ml) and daily calcium excretion - 0.68 mmol (normal - more than 2.5 mmol). These results, taking into account the normal level of inorganic phosphate in the blood, confirmed the assumption of calcium deficiency against the background of vitamin D deficiency. Combination drugs are traditionally used to correct calcium and vitamin D deficiency. This case seemed very unusual to us, especially for the practice of a rheumatologist. The nature of the complaints, as well as the laboratory picture, required a broad differential diagnosis. This observation seems to us to be a good reason to draw the attention of rheumatologists and therapists to the problem of pain in the pubic area, the diagnosis of which can be a serious test for a doctor.
Causes of symphysiopathy
It must be remembered that pain and changes in the symphysis are not typical for all expectant mothers. There are factors that contribute to this pathology:
- heredity (if your mother, grandmother or sister had symphysiopathy or symphysitis, then you may experience the same thing; you need to be alert)
- characteristics of your connective tissue (not all medical experts recognize this factor; if you have connective tissue dysplasia, then during pregnancy there may be very unpleasant sensations in the ligaments)
- the birth of not the first child
- kidney disease (with renal pathologies, minerals and proteins are released from the body along with urine, which normally should remain in the body and take part in metabolism and tissue formation; this excess excretion leads to the fact that the symphysis becomes softer than necessary, and diverges)
- lack of calcium and vitamin D (the symphysis may be soft because there is very little calcium in your body, this deficiency is quite typical for pregnant women; in parallel with this factor, other symptoms will develop: fractures, split nails, brittle hair and poor appearance)
Possible complications and preventive measures
Considering the typical clinical manifestations of the disease, one cannot ignore the potentially dangerous consequences of damage to the pubic symphysis. These include:
- damage to the bladder, genitals, rectum;
- neurological disorders (radiculitis, paresthesia, muscle wasting);
- internal or retroperitoneal bleeding;
- infectious damage to the joint and surrounding tissues (osteomyelitis, thrombophlebitis);
- gait disturbance, lameness;
- difficulties with childbirth.
- damage to the bladder, genitals, rectum;
- neurological disorders (radiculitis, paresthesia, muscle wasting);
- internal or retroperitoneal bleeding;
- infectious damage to the joint and surrounding tissues (osteomyelitis, thrombophlebitis);
- gait disturbance, lameness;
- difficulties with childbirth.
To prevent pregnancy-related illnesses, you should plan the birth of your child with special care. The expectant mother should take specially developed vitamin complexes that strengthen both the general immune system and the joints.
Simple exercises that can help you strengthen the muscles of your back, abdomen and buttocks will help prevent arthrosis. Air and sun baths will not be superfluous. Fresh air and ultraviolet radiation promote the active production of vitamin D, which is so necessary for the absorption of calcium and phosphorus in the small intestine.
We need to fight excess weight, establish a daily routine, and give up bad habits. People who play sports at a professional level should use a special bandage or orthosis for the hip joint and try to limit the load on the affected joint.
Joint pain not only takes away vitality, but also indicates the presence of disorders in the body that can result in stiffness of the joints of the skeleton bones or even total immobilization.
If you experience even the slightest discomfort in the pubic area, you should see a doctor.
Methods of timely diagnosis and the prescription of adequate therapy will avoid severe complications and prevent further destruction of the cartilage tissue of the symphysis pubis.
Reading time: 10 minutesCommentsPhoto: ainridzuan.com
Degrees of symphysiopathy
The pubic bones can diverge, as we noted above, to different distances. According to this factor, the degrees of symphysiopathy are distinguished:
- first degree – 0.5-0.9 cm
- second degree – 1-2 cm
- third degree – more than 2 cm
This, of course, cannot be seen with the naked eye. Only ultrasound diagnostics can help determine the extent of the condition in question in a pregnant woman. A palpation method is also used, which makes it possible to identify excessive softness of the cartilage and the fact that the pelvic bones are not stable.
The effect of symphysitis on pregnancy
Symphysiopathy does not affect pregnancy in any way. But the condition of a pregnant woman, due to specific symptoms, will be worse than it could be. Remember that stretching the symphysis pubis can lead to its excessive thinness, which is why cartilage rupture occurs during the birth of the baby. This, as we have already written, is called symphysiolysis. A woman who has given birth will lose her ability to work for 2 or more months.
There is a high risk of rupture of the joint in those expectant mothers who have a narrow pelvis (male body type), and at the same time their baby is heavy. If your doctor has diagnosed second or third degree symphysiopathy, he may recommend a cesarean section instead of a natural birth. The same can happen if it is revealed that the fetus is very large and can damage the mother’s birth canal.
Dangers of symphysitis
Symphysiopathy in itself is not a threat to life or even health. But if a rupture of the symphysis pubis occurs during childbirth, this indicates injury: the pelvis is broken. When the bones diverge by two centimeters, the fracture is considered stable. Most likely, it will not lead to dangerous complications. When the bones are more than 5 centimeters apart, there is a threat to the health of the mother in labor.
The edges of the separated bones can damage the clitoris, bladder or urethra. In the area of the joints, bleeding is possible, which subsequently threatens arthritis. In such severe cases, surgery is required. But this is a very small percentage of women giving birth. They spend a month and a half or more lying down, with their legs bent and separated at the knees.
Diagnostics
Pregnant women who complain of pubic pain, have a changed gait after childbirth or swelling of the pubis before or after the birth of the baby should be examined. An ultrasound of the symphysis pubis is performed to assess the distance between the bones of the pubis and to identify the inflammatory process. But, if the discrepancy is small, the woman may have very, very severe pain. And vice versa. Cases may vary. Therefore, ultrasound can only show how much the pubic symphysis has diverged. When making a final diagnosis, the doctor also considers how severe the typical symptoms of the pathology are.
An X-ray of the pelvic bones is taken after the woman has given birth if symphysitis is suspected. The method is also relevant for monitoring ongoing therapy. In rare cases, X-ray pelviometry is performed for those who are still carrying a child. This is necessary to assess the pelvic circumference and head size of the unborn baby.
After the baby is born, high-precision methods such as computed tomography (CT) and magnetic resonance imaging (MRI) are used. They are also needed to identify other pelvic diseases (if any).
Medicines
Photo: sochi-informburo.ru
Nonsteroidal anti-inflammatory drugs (NSAIDs) are used in the treatment of symphysitis to eliminate the inflammatory process. In addition, these drugs have an analgesic (pain-relieving) effect. Currently, the pharmacological market is rich in various representatives of non-steroidal anti-inflammatory drugs, but not all can be used during pregnancy.
In the first and second trimesters of pregnancy, for symphysitis, drugs such as diclofenac and ibuprofen are prescribed, which have a pronounced anti-inflammatory effect. The mechanism of action of diclofenac is based on inhibition (suppression) of the synthesis of substances that play a key role in the process of inflammation (prostaglandins and cyclooxygenase). In addition to the anti-inflammatory effect, diclofenac has an analgesic effect. However, it is worth noting that it is rational to use diclofenac only for moderately severe pain, as it has a slight analgesic effect. Ibuprofen has an anti-inflammatory effect by inhibiting cyclooxygenase and reducing prostaglandin synthesis. As a result, vascular permeability decreases and microcirculation improves. In later stages of pregnancy, taking these drugs is prohibited, as there is a risk of premature closure of the ductus arteriosus in the fetus, impaired renal and liver function in the newborn, etc.
Calcium preparations are used when a deficiency of this microelement is detected in a woman’s body. The following names of drugs exist:
- Calcium-D3 Nycomed;
- Calcium-D3 Nycomed Forte;
- Calcium-D3-MIC;
- Calcemin.
For better absorption, it is recommended to take calcium supplements with meals or immediately after meals. These drugs are well tolerated; in rare cases, side effects such as periodic pain in the epigastric region (upper abdomen), nausea, and bowel disorders such as constipation may occur. A contraindication to taking the drug is individual intolerance to the components. The drug is discontinued if adverse reactions develop, as well as with increased calcium levels in the blood and urine.
Vitamin and mineral complexes are used to strengthen the general condition of the body. They contain a specially combined list of vitamins and microelements necessary for the normal functioning of our body.
Differential diagnosis
Pain may indicate not only symphysitis, but also other pathologies. Therefore, do not remain silent if you suffer from pubic pain during pregnancy or after childbirth. Tell your OB/GYN about this. After examination by a professional doctor, it will be possible to talk about the need for other research methods.
Differential diagnosis of symphysitis is required with:
- sciatica (sciatica)
This term refers to pain in the area of the sciatic nerve. A woman may feel discomfort in the area from the groin and tailbone down the leg to the shin. This is not an independent disease, but a symptom that indicates arthrosis, arthritis, damage to muscle tissue or tumor formations in the patient’s pelvis
- lumbago
This term refers to sudden back pain that occurs due to spinal pathology. This happens, for example, with intervertebral hernia or osteochondrosis. Pain may also be felt periodically in the groin, leg or abdominal area. Often the result of pain is a disorder of defecation or urination.
- infections of the reproductive and urinary system
The above factor can also cause pubic pain. Tingling, pain and a burning sensation in the groin can be manifestations of cystitis, which are the result of sexually transmitted infections or penetration of E. coli into that area. Pregnant women often get cystitis, so if you have pubic pain, your doctor may recommend testing for infections.
- osteomyelitis and tuberculous bone lesions
Such cases are very rare, but they should also be taken into account when diagnosing. It is necessary to take into account if the patient previously had tuberculosis or had a pelvic injury. Diagnostic methods such as radiography and ultrasound are used, and infection is also detected by culture or smears.
How does it manifest?
Damage to the symphysis pubis occurs gradually. Aching pain occurs in the pubic area, then moves to the perineum. As the disease progresses, the pain intensifies, the pain does not stop even at rest, and lameness occurs. There are 3 degrees of development of arthrosis of the symphysis pubis:
- It manifests itself as vague symptoms, mild pain during movement, the formation of marginal bone growths, the muscle structure is in good shape.
- There is an increase in pain radiating to the groin and thigh area. Due to the displacement of the articular parts, stiffness of the hip joint appears, arthritis develops, and osteophytes are abundantly formed.
- There is constant sharp pain, discomfort and movement functions are limited. The tendon junction between the pubic bones contracts, causing lameness.
Return to contents
Treatment of symphysitis
As we have already written, symphysiopathy differs from symphysitis. This condition occurs only in women carrying a child. Symptoms usually go away 4-6 months after the day of birth. But in some cases, the pubis hurts for about a year. No treatment is prescribed. With symphysiolysis, therapy is mandatory. And it depends on the degree of the gap.
If a pregnant woman (who has not yet given birth) has symphysiopathy, then the symptoms can be made a little milder:
- don't sit in one place for a long time
- do not walk or climb stairs for very long periods of time
- when you are stationary, distribute your body weight evenly
- include calcium-rich foods and dishes in your diet
- take calcium supplements (but only if your doctor has prescribed them for you; uncontrolled use of this supplement in the last three months of pregnancy is especially harmful; calcium should not be taken in the last 3 weeks before giving birth)
- control your weight (if you gain excess fat, it can harm your ligaments and joints, which will lead to even more pain)
- wear a prenatal bandage starting 25-28 weeks after conception
Therapy for symphysitis in a pregnant woman should be carefully monitored by her gynecologist or orthopedic dentist. You may need to consult other specialists, such as a neurologist or physiotherapist.
Exercises for pain
These exercises will not help you get rid of your pain 100%, but they will relieve the symptom.
- “cat” pose: kneel and elbows, straighten your shoulders and back, then arch your back, at the same time lowering your head to the floor along with your gaze, while keeping your abdominal muscles tense. These steps must be repeated 3-10 times
- raising the pelvis. Starting position: lying on your back. Bend your knees, then slowly raise your pelvis as much as possible, and then lower it without sudden movements. Repetitions are also needed several times, depending on how you feel.
- Kegel exercises. You should simulate holding and releasing a stream of urine, thereby activating the pelvic floor muscles
Folk remedies
Photo: yandex.ru
Symphysitis should be treated by a qualified specialist. The use of various traditional medicines is strictly prohibited.
At home, a woman who has the problem in question should monitor her diet. First of all, preference should be given to dairy products (cheese, cottage cheese, milk, etc.), which are rich in calcium. You should also be careful about flour products and fatty foods, as their excess consumption leads to weight gain. In turn, excess weight increases the load on the pelvic ring, and as a result, pain increases.
With symphysitis, it is important to reduce excessive physical activity, refrain from climbing stairs, fast walking, and staying in one position for a long time (over 30 minutes - 1 hour). It is also recommended to perform specially designed physical exercises daily that strengthen the gluteal, thigh and perineal muscles. We suggest the following exercises, which should be performed several times a day:
- Take a lying position. Place your feet as close to your buttocks as possible. Then spread your bent knees to the sides as far as possible and stay in this position for a few seconds, after which you close your knees again. It is necessary to repeat this exercise from 5 to 10 times, gradually increasing the number of exercises.
- Take a lying position. Bend your knees and lift your pelvis so that you form a straight line with your body. It is recommended to perform this exercise 5 to 10 times daily, gradually increasing the number of exercises. If pain occurs, you should stop doing the exercise.
- Get on your knees and place your palms on the floor so that they point forward. The correct position should look like this: arms straight, knees bent at right angles to the body, back straight. As you inhale, round your back as much as possible and lower your head down. As you exhale, slowly return to your starting position. Then, while inhaling, bend your body down as much as possible. As you exhale, return to the starting position. The exercise should be repeated 5 – 10 times.
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.
Treatment of symphysiolysis in newborns
Pain relief is needed because this is one of the main symptoms. The doctor prescribes NSAIDs. These are non-steroidal anti-inflammatory drugs. These drugs include ibuprofen and paracetamol. But the drug itself and the dosage must be determined by the doctor, because it is very individual. NSAIDs are prescribed only if the pain is very severe. The drugs have side effects. If taken for a long time and without medical supervision, liver pathology or stomach ulcers may develop.
If you feed your baby naturally, consult your doctor about taking NSAIDs. Not all medications from this group can be taken during lactation, because they can harm the newborn.
The next component of complex therapy for symphysiolitis after childbirth: a gentle regimen. Physical stress on a woman’s body should be minimized. Canes can be used for walking. In some cases, the doctor prescribes wearing a bandage that will capture the trochanters of the femur. This will reduce pain and prevent bone separation in the future. Thanks to the bandage, the symphysis will heal faster.
Physiotherapeutic methods of treatment are used, including magnetic therapy. It is important to combine this method with fixation of the pelvic bones and bed rest. The doctor prescribes strict bed rest for those women in labor whose bones have severely eroded and the symphysis has torn. To speed up the fusion process, you need a special hammock with weights suspended crosswise. Thanks to it, the reduction of the pubic bones will be ensured. A controlled pelvic girdle may also be needed for treatment. It enhances the hammock effect mentioned above.
Old tears can only be treated with surgery. To make the pelvis whole again, plastic materials and rods are used.
Aggravating factors
In addition to hormone production, there are several factors that provoke sprains of the pubic ligaments:
- disturbance of calcium-phosphorus metabolism;
- lack of vitamin D;
- increase in body mass index
- history of three or more pregnancies;
- injuries to the pelvic bones, even old ones;
- hereditary diseases of the musculoskeletal system;
- high fetal weight (the expected weight of the child at the time of birth is 4 kg or more);
- insufficient amount of physical activity of the mother.