Causes of increased C-reactive protein
The formation of increased levels of CRP in the blood is caused by inflammatory processes due to acute and chronic diseases of various origins.
In cases where the analysis indicators range from 10 to 50 mg/l, this may indicate the development of:
- tuberculosis;
- dermatomyositis;
- systemic lupus erythematosus;
- rheumatoid arthritis;
- gout;
- psoriatic arthritis;
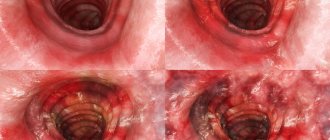
- ulcerative colitis;
- myocardial infarction;
- rheumatoid arthritis.
CRP test results of more than 50 ml/liter indicate serious pathologies with possible death:
- acute pancreatitis with tissue necrosis;
- severe bacterial infections (sepsis, pneumonia, pyelonephritis);
- Crohn's disease in the active phase;
- seronegative spondyloarthritis;
- deep vein thrombosis;
- tumor necrosis.
In some cases, the level of C-reactive protein rises to 100-300 mg/l, which is typical in severe inflammatory processes as a result of extensive burns, injuries, as well as sepsis, including postoperative sepsis.
During the diagnostic process and when assessing the effectiveness of drug therapy, approximate CRP indicators are used, which differ depending on the disease.
| Diseases | Features of increasing C-reactive protein |
| Viral infections (influenza, chicken pox, rubella, viral hepatitis) | Increases slightly (up to 20 units) |
| Bacterial infections (streptococcal, staphylococcal, meningitis, salmonellosis, bacterial pneumonia) | The level of CRP reaches 100 mg/l, but after the start of effective treatment it decreases on the third day of therapy |
| Neonatal sepsis | Increase to 12 mg/l |
| Abscess, thrombophlebitis after surgery | Protein levels do not decrease on the fifth day after surgery |
| Oncological diseases (malignant tumors) | An increase in the level of C-reactive protein in the blood to 20-40 mg/l is due to tumor growth, and more than 100 is due to metastasis |
| Diseases accompanied by tissue necrosis (myocardial infarction, intestinal necrosis, lung necrosis) | Malignant tumors are characterized by high levels of CRP (more than 120-150) in the absence of any acute symptoms |
Elevated CRP – is this always a pathology?
In adults, an elevated CRP value exceeds 5 mg/l, with the exception of smokers, people with obesity or hypertension, for whom the norm is less than 10 mg/l.
In older children, elevated CRP values are considered to be greater than 10 mg/L. As with adults, interpretation of the result should be left to the pediatrician. He will evaluate the result in the context of the child's condition and medical history.
Slightly elevated CRP values up to 40 mg/l may be observed in older people and during pregnancy.
Therefore, when interpreting the results and drawing up a medical report, it is necessary to take into account other laboratory parameters, such as a complete blood count (CBC) with a leukocyte formula.
Reasons for increased C-reactive protein in adults
There are 3 main groups of reasons that can lead to an increase in the content of C-reactive protein in adults - inflammation, oncology and pathology of arterial vessels. They include a huge number of diseases, between which it is necessary to conduct a diagnostic search.
The degree of protein increase helps to roughly navigate the pathologies:
- Less than 19 mg/l - a slight excess of the normal value can occur due to any significant factor affecting the body. However, with constantly elevated CRP, autoimmune and oncological pathologies should be excluded.
- 20-50 mg/l – this level is more typical for human viral diseases, such as mononucleosis, adenovirus or rotavirus infection, herpes and others.
- More than 100 mg/l - such a strong immune reaction is most often observed with bacterial infections (microbial pneumonia, salmonellosis, shigellosis, pyelonephritis, etc.)
But the level of CRP is a very approximate indicator, and even the boundaries indicated above are quite arbitrary. It happens that a patient with rheumatoid arthritis has a CRP above 100 during an exacerbation. Or in a septic patient 5-6 mg/l.
Possible diseases
C-reactive protein will be elevated within the first 6-8 hours from the onset of the disease, and its values will correspond to the severity of the process (the more severe the course, the higher the CRP). Such properties of CRP allow it to be used as an indicator at the onset or course of various inflammatory and necrotic processes, which will be the reasons for the increase in the indicator:
- Bacterial and viral infections;
- Acute cardiac pathology (myocardial infarction);
- Oncological diseases (including tumor metastasis);
- Chronic inflammatory processes localized in various organs;
- Surgical interventions (violation of tissue integrity);
- Injuries and burns;
- Complications of the postoperative period;
- Gynecological pathology;
- Generalized infection, sepsis.
Elevated CRP often occurs with:
- Increased protein in the blood: what does it mean, causes and treatment
- Tuberculosis;
- Systemic lupus erythematosus (SLE);
- Lymphogranulomatosis;
- Acute lymphoblastic leukemia (ALL);
- Jade;
- Rheumatism;
- Cushing's disease;
- Visceral leishmaniasis.
It should be noted that the indicator values for different groups of diseases may differ significantly, for example:
- Viral infection, tumor metastases, rheumatic diseases, which proceed sluggishly, without severe symptoms, give a moderate increase in the concentration of CRP - up to 30 mg/l;
- Exacerbation of chronic inflammatory processes, infections caused by bacterial flora, surgical interventions, acute myocardial infarction can increase the level of the acute phase marker by 20 or even 40 times, but in most cases from such conditions an increase in concentration can be expected to 40 - 100 mg/l ;
- Severe generalized infections, extensive burns, septic conditions can very unpleasantly surprise clinicians with numbers indicating the content of C-reactive protein; they can reach prohibitive values (300 mg/l and much higher).
It is also worth raising a very important issue regarding the increased amount of CRP in healthy people. A high concentration of C-reactive protein with complete external well-being and the absence of signs of any pathology suggests the development of an oncological process. Such patients should undergo a thorough examination.
Reasons for men
In the absence of obvious symptoms suggesting a specific diagnosis, it is recommended to exclude these diseases first:
- Tumors;
- GERD;
- Gastritis;
- Peptic ulcer of the duodenum/stomach;
- Pancreatitis;
- Cholecystitis;
- Crohn's disease;
- Ulcerative colitis.
- Urolithiasis (UCD);
- Glomerulonephritis;
- Prostatitis;
- Infections that are sexually transmitted (chlamydia, mycoplasma/ureaplasma infection, gardnerellosis, etc.)
- Chronic obstructive pulmonary lesions (chronic bronchitis, emphysema);
- Occupational diseases (silicosis, pneumoconiosis, silicotuberculosis and others).
To facilitate the diagnostic search, you should ask your doctor what pathologies are most common in middle-aged and older men.
Reasons for women
First of all, the presence of the following pathologies should be excluded:
- Oncology – it is women 40-60 years old who often experience the debut of tumor growth, for example breast cancer or cervical cancer. In order to detect them promptly and treat them at an early stage, it is strongly recommended to undergo an annual examination by a gynecologist, starting from the age of 35.
- Center of chronic infection. CRP is an excellent indicator of prolonged inflammatory reactions. Despite the fact that they may not bother a person (up to a certain time) and may not reduce his quality of life, their presence is still reflected in the analysis of reactive protein in women.
- Gynecological diseases (endometriosis, endometritis, true cervical erosion, cervicitis and others).
In the first place among girls are lesions of the genitourinary tract: chronic pyelonephritis, cystitis, urethritis, sexually transmitted infections (chlamydia, mycoplasmosis, gardnerellosis, etc.). The next most common are pathologies of the digestive system - pancreatitis, chronic cholecystitis, intestinal dysbiosis and others.
Causes in children
There are a large number of diseases caused by microorganisms, but in children, lesions of the digestive tract and respiratory tract are most common. They can occur acutely with the appearance of pronounced symptoms (dysentery, salmonellosis, pneumonia, ARVI and others) or develop slowly in the body, causing a chronic disease. Bronchitis, tonsillitis, sinusitis, gastritis, etc. can occur in this way.
In second place among the causes of increased C-reactive protein in children are parasitic pathologies. Since at a young age a child’s hygiene is still developing, his risk of introducing the parasite into the body increases significantly. In Russia, the most common types of these microorganisms are:
- Total protein in the blood is low - what does this mean, causes and treatment
- Ascaris;
- Pinworm;
- Giardia;
- Opisthorchus;
- Wide tapeworm;
- Bovine and pork tapeworm.
Only after excluding the listed pathologies should one look for other factors in the child’s body that can increase the concentration of CRP. Of course, this stage can be skipped if there are characteristic symptoms or test results confirming a different diagnosis.
Effect of drugs on CRP concentration
Taking acetylsalicylic acid or aspirin, even in high doses, does not affect the quantitative level of CRP. This is somewhat surprising since aspirin is known for its anti-inflammatory properties.
Patients with high cholesterol who take statins are less likely to have a heart attack because statins not only lower lipid levels but also have anti-inflammatory properties. This is very important because high CRP and low cholesterol are more dangerous than high cholesterol and low CRP. The level of CRP is also reduced by drugs from the group of fibrates and beta-blockers, but less effectively than by statins.
Functions
The synthesis of C-reactive protein is carried out by liver cells (hepatocytes) under the influence of pro-inflammatory cytokines to perform the protective functions of the body:
- binds substances (polysaccharides, nucleic acids, polyanions) located on the surface of bacteria, fungi and parasites;
- activates the work of immune system enzymes for nonspecific protection against infectious processes;
- promotes phagocytosis - the capture and destruction of foreign cells by macrophages, microphages and monocytes;
- activates the work of platelets during bleeding;
- identifies, neutralizes and removes toxic substances formed during the breakdown of its own cells.
Assessing the risk of heart attack using CRP
What does C-reactive protein indicate if a person does not have inflammatory or oncological diseases? Not long ago, scientists discovered the connection of this substance with the development of vascular complications. This study is especially relevant for people with cardiovascular disease or risk factors.
| Diseases | Risk factors |
|
|
For people with any of these conditions, a CRP level greater than 1 mg/L indicates a risk of a vascular complication. These patients are significantly more likely to have strokes, heart attacks, kidney damage, or heart failure.
- A protein level of 1-3 mg/l indicates an average risk of developing pathologies;
- Exceeding the limit of 4 mg/l demonstrates a high risk of vascular accident.
Indications for use
Analysis for C-reactive protein is part of a set of diagnostic measures and is prescribed to identify the following diseases and pathological conditions:
- parasitic, bacterial and viral infections;
- tumors;
- oncological processes;
- assessing the degree of tissue necrosis as a result of injuries, burns, destructive changes in internal organs;
- early detection of postoperative complications;
- diagnosis of transplant rejection;
- assessment of the condition during myocardial infarction;
- tracking the results of therapy for rheumatoid processes;
- determination of cardiovascular risk;
- the effectiveness of antibacterial, anti-inflammatory treatment, immunosuppressive therapy;
- neonatal sepsis.
Complexes with this research
Inflammation of the joints Indicator of the risk of developing systemic manifestations of rheumatoid arthritis 870 ₽ Composition
For those at risk of COVID-19 Diagnosis of diseases complicating the course of coronavirus infection 4,620 ₽ Composition
Women's check-up No. 1 38 studies for annual preventive examination 19,720 ₽ Composition
IN OTHER COMPLEXES
- Advanced anti-aging diagnostics in postmenopause RUB 29,710
- Advanced male anti-aging diagnostics RUB 34,230
- Men's check-up No. 1 RUB 18,920
- Male anti-aging diagnostics RUB 13,520
- Anti-aging diagnostics in postmenopause RUB 12,860
What it is?
C-reactive protein is a two-component molecule consisting of proteins (peptides) covalently linked to several oligosaccharides. The name is due to its ability to interact with C-polysaccharides of bacteria of the Streptococcaceae family, thereby forming a stable antigen-antibody complex (precipitation reaction). This mechanism refers to the protective reactions of the human body to infectious infection.
When a pathogen penetrates, the immune system is activated, which stimulates the process of synthesis of small peptide molecules - cytokines. They provide signal transmission about the manifestation of the inflammatory process and the need to enhance the production of acute phase proteins, which are CRP. After 1-2 days, there is an increase in CRP by tens and hundreds of times compared to normal values.
Norm
Unlike most indicators, the C-reactive protein norm is universal for all groups of the population, regardless of age and gender.
According to the recommendations of WHO doctors, the norm is up to 5 mg/l. In newborns, no more than 15 mg/l.
Exceeding this value, in most cases, allows one to suspect an inflammatory or oncological disease, depending on the presence of certain changes in the person’s body.
With the development of knowledge about this substance and the advent of new high-precision equipment, scientists began to talk about another indicator - it is called the basic value of CRP. This value allows you to assess the risk of damage to the heart and arterial vessels in a person who does not suffer from any inflammatory reaction. The norm for the basic level of reactive protein differs significantly from traditional data - it is less than 1 mg/l.
It is better to take tests in the same laboratory, because CRP is determined by different methods, using:
- ELISA;
- radial immunodiffusion;
- nephelometry,
therefore, repeated results may differ, which will prevent the dynamics from being interpreted correctly.
Comparison with ESR
In addition to C-reactive protein, ESR (erythrocyte sedimentation rate) is also a marker of acute inflammation in the body. What they have in common is that both indicators increase in a number of diseases. What is their difference:
- CRP increases much earlier and decreases faster. Therefore, in the early stages of diagnosis, it is more informative than ESR.
- If the treatment is effective, then the c-reaction. protein decreases on days 7-10, and ESR decreases only after 14-28 days.
- The results of ESR are influenced by the time of day, plasma composition, number of red blood cells, gender (higher in women), but the results of CRP do not depend on these factors.
It becomes clear that the C reactive protein test is a more sensitive method for assessing inflammation than ESR. If you suspect any disease, to establish the cause, determine whether the process is acute or chronic, assess the activity of inflammation and the effectiveness of the therapy, it is more informative and convenient.
CRP and osteoporosis
Until now, doctors continue to study what this test shows, in addition to inflammation and cardiovascular risk. Recent studies have proven the connection of C-protein with depletion of calcium reserves and pathologies of bone tissue, that is, osteoporosis. Why does this condition occur, and why is it dangerous?
The fact is that maintaining the inflammatory process requires a large amount of enzymes and microelements, including calcium ions. If it lasts long enough, the amount of these substances in the blood becomes insufficient. In this case, they begin to arrive from the depot. For calcium, bones are such a depot.
A decrease in its concentration in bone tissue leads to its increased fragility. For a person with osteoporosis, even a minor injury is enough for them to experience a complete fracture or “crack in the bone” (incomplete fracture).
At this time, doctors have not determined the exact cutoff for CRP at which the risk of bone changes increases. However, scientists from the NIIR RAMS have found that prolonged excess of this test norm is a serious risk factor for depletion of calcium reserves.
Preparing for the examination
In order for an analysis to detect the level of CRP in the blood to show a reliable result, it is necessary to properly prepare the child for the test:
- stop taking painkillers and antipyretic non-steroidal anti-inflammatory drugs 1-2 weeks beforehand, after consulting with your doctor;
- 2-3 days before the analysis, remove heavy physical activity;
- the day before the test, remove fatty and fried foods from your diet;
- For 8-12 hours then study, do not eat or drink anything other than water.
The analysis cannot be taken after physiotherapeutic procedures, as well as ultrasound, rectal, x-ray examination, and fluorography.