How does small intestine cancer develop?
Oncology begins with the appearance of just one altered cell in the body. It arises due to exposure to harmful substances, various diseases or simply random failures, grows and multiplies. Over time, there are many of them, they form a tumor and destroy the tissues in which they develop. Most of these cells are identified and destroyed by the immune system, but some of them are able to resist it - they secrete special proteins, thanks to which our natural defense does not consider them dangerous.
The possibilities of cancer do not end there - its cells enter the bloodstream and lymphatic system. The lymphatic system complements the cardiovascular system. The lymph circulating in it - the intercellular fluid - washes all the cells of the body and delivers the necessary substances to them, taking away waste. In the lymph nodes, which act as “filters,” dangerous substances are neutralized and removed from the body. systems, spread throughout the body, become established in various organs and create metastases in them - new foci of the disease.
To better understand the disease, we need to understand how our digestive system works.
After we chew and swallow food, it enters the esophagus, a narrow muscular tube through which it passes into the stomach, where it is partially digested. There it turns into a thick liquid and is excreted into the small intestine, where large molecules continue to be broken down into small ones and most of the nutrients are absorbed.
The small intestine of an adult is about 4.5-6 meters long and consists of 3 sections:
- Duodenum
, which receives substances necessary for digestion and decomposing carbohydrates, proteins and fats - produced by the liver and pancreas. This is where most cancers begin. - The jejunum and ileum,
where nutrients from the foods we eat are absorbed into the blood.
The ileum drains into the colon, where water and some minerals are absorbed, and the resulting waste moves to the rectum, where it is stored until it leaves the body through the anus.
Types of Small Bowel Cancer
Doctors identify several types of dangerous neoplasms in this part of the digestive system, each of which develops in certain cells:
- Adenocarcinomas
are cancers of the small intestine that begin in the glands lining the inner surface of the organ. They account for approximately 1 in 3 cases of cancer. - Carcinoid,
or
neuroendocrine, tumors
arise in cells that help control the secretion of digestive juices and the movement of food through the gastrointestinal tract. - Lymphomas
appear in immune cells - lymphocytes, whose main task is to fight infections and tissue damage. - Sarcomas
develop in various types of connective tissue, such as muscle. Their most common subtype, gastrointestinal stromal tumors, begin in so-called Cajal cells, which signal the muscles of the gastrointestinal tract to contract.
Why does small intestine cancer develop?
To date, the exact causes of the development of small intestinal cancer are not known to scientists and doctors - they only know about the factors that increase the likelihood of its development. Having one, two or three of them does not mean that a person will necessarily become a patient of an oncologist.
These include:
- Crohn's disease
, which causes the immune system to attack the gastrointestinal tract. - Poor nutrition
– an excess of red meat, salty, fatty and smoked foods in the diet, as well as a lack of fruits and vegetables. - Celiac disease
is an abnormal reaction of the body to the protein gluten, which is found in wheat and other types of grains. The immunity of its owners damages the intestinal mucosa, forcing it to produce new cells, each of which may turn out to be tumor cells. - Familial adenomatous polyposis
is the presence of many polyps - tissue growths on the intestinal wall, which over time can turn into a malignant, that is, life-threatening neoplasm. - Age
: this type of cancer most often develops in people aged 60 to 70 years. - Cystic fibrosis
is damage to the glands, respiratory and digestive systems due to the accumulation of thick mucus in organs and tissues. - Smoking and alcohol
: Some studies have shown that inhaling toxic tobacco smoke and drinking alcoholic beverages can trigger the development of the disease. - Other polyposis syndromes
: Lynch, which increases the chances of developing any type of dangerous tumor in people under the age of 50, or Peutz-Jeghers, which leads to the appearance of polyps in various parts of the body. - Having colon cancer
increases the likelihood of developing small intestinal cancer.
Endoscopic department of the oncology center Lapino 2
Classification
Depending on the cause, the following types of enteritis are distinguished:
- Infectious.
- Parasitic. Consequence of helminthiasis or protozoa infection.
- Nutritional. Occurs due to nutritional disorders.
- Postoperative.
- Radiation.
- Autoimmune.
- Secondary enteritis. Develops against the background of existing other chronic gastrointestinal diseases.
During the development of enteritis, atrophy of the intestinal villi may occur. Depending on the degree of atrophic changes, a partial or subtotal form is distinguished. The more villi are lost, the more absorption is impaired.
The disease can be mild, moderate or severe. When diagnosing, it is important to indicate whether a chronic disease is in remission or exacerbation.
Enteritis is often accompanied by functional disorders of the small intestine: chronic disorder of digestion, transport and absorption of food, insufficient production of enzymes, increased loss of nutrients.
If the disease spreads to the mucous membrane of the colon, concomitant colitis develops.
Signs and symptoms of small bowel cancer
The symptoms of the disease are similar to other fairly common health problems. Often people do not pay attention to them or take them for a normal digestive problem, as a result of which a considerable part of patients consult a doctor several months after their appearance.
Abdominal pain is often the first symptom of cancer.
– it comes and goes, often occurs after eating, but does not cause serious discomfort to its owner.
As the tumor grows, the intestinal lumen narrows, the passage of digested food through it slows down, and the discomfort intensifies. When it becomes large enough and completely blocks the passage, a person experiences obstruction of the digestive tract, which leads to severe pain, nausea and vomiting
.
Sometimes the tumor begins to bleed. If the blood flows slowly, the patient's number of red blood cells - cells that carry oxygen from the lungs and deliver them to other tissues - gradually decreases, causing weakness and fatigue
.
If this happens quickly, the patient becomes dizzy and faint,
and his
stool
becomes
black
and
tarry
.
Quite rarely, duodenal cancer causes jaundice
– yellowing of the skin, mucous membranes and whites of the eyes. This occurs when the tumor grows and the bile duct is blocked, due to which the contents of the liver cannot enter the intestines. As a result of this blockage, bile, necessary for digesting food, and the substance it contains, which colors the tissues yellow, enter the bloodstream.
In rare cases, cancer leads to the appearance of perforations - holes in the intestinal wall through which the contents of the organ exit into the abdominal cavity. Signs of this condition may include severe abdominal pain, nausea and vomiting.
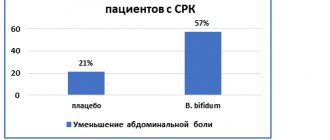
Treatment of irritable bowel syndrome
Therapy for IBS should be carried out comprehensively in several stages. The treatment regimen depends on the individual characteristics of the body, the degree and time of the pathology. Most often, drug therapy is prescribed, which is supplemented by a special diet. In the absence of comprehensive treatment, symptoms will reappear from time to time.
The medications that the doctor prescribes for the treatment of IBS not only eliminate painful symptoms, but also improve the condition of the digestive system, and also prevent relapses and complications. When treating diarrhea syndrome, medications with antimicrobial properties are prescribed. They relieve irritation of intestinal tissues, stop excess flatulence and restore normal intestinal function.
When treating IBS with constipation, the use of natural medicines is indicated that eliminate difficulties with defecation, have a gentle effect on inflamed intestinal tissue and free it from feces. May be in the form of chewable tablets or rectal suppositories.
If the appearance of IBS is associated with neurological disorders, antidepressants are prescribed - they normalize the functioning of the nervous system and improve the psycho-emotional state.
To relieve pain, painkillers and antispasmodics are used - they relax muscle fibers and tissues that are in hypertonicity.
Diet for irritable bowel syndrome
The diet for IBS depends on what symptoms accompany the pathology. If you experience frequent constipation, you should exclude dry, salty foods from your diet. For diarrhea, avoid liquid foods, vegetables, and fruits.
If you suffer from flatulence, you should limit dairy products, nuts, and beans. If there is severe pain in the intestines, fatty, salty, and heavy foods are not allowed.
At the Medunion clinic you can undergo a full examination and treatment of irritable bowel syndrome. We employ practicing doctors with over 10 years of experience. In the diagnostic room you can take all tests and undergo hardware examination in a comfortable environment. For our clients there is a special offer “doctor at home”. If you are unable to visit our medical center yourself, a doctor will come to you and conduct an examination at home.
Take care of your health and make an appointment with a multidisciplinary medical center directly on our website.
Diagnosis of small intestine cancer
Diagnostics is necessary not only to identify oncology - its data allows us to understand how far the disease has spread and what treatment is best for a person.
You can undergo a full examination for small intestinal cancer at Onko. We have the most modern equipment and a team of highly qualified specialists who guide the patient from diagnosis to any treatment.
Diagnosis begins with a physical examination, questioning about symptoms, possible risk factors and family health problems. Then the doctor prescribes a whole list of studies:
- Blood tests
: show its composition and the number of oxygen-carrying red blood cells, the level of which may decrease due to bleeding caused by cancer. - FGDS
-
fibrogastroduodenoscopy
: examination of the duodenum using an endoscope - a thin flexible tube with a light source and a camera at the end. The device is inserted into the mouth, passes through the esophagus and stomach, and allows not only to assess the condition of the tissues, but also to remove small pieces of them, which are then sent to the laboratory. - Capsule endoscopy
: A painless procedure involving swallowing a small capsule about the size of a large tablet. It passes through the entire digestive system, takes thousands of pictures transmitted to a special wearable device, and leaves the body naturally. - Balloon enteroscopy
: insertion through the mouth or anus of a special endoscope equipped with one or two balloons that are secured in place, allowing a close and detailed examination of the intestinal wall. - Colonoscopy
: insertion of a thin, flexible tube with a light source and a camera at the end through the anus. This procedure is used to study the condition of the final part of the small intestine and take tissue samples from suspicious areas. - Imaging tests, such as CT
or
MRI
: create clear images of organs using X-rays, magnetic fields, or radioactive substances. They are prescribed to detect a tumor, search for signs of re-development of the disease and identify metastases - additional foci of oncology, - Biopsy: taking small pieces of tissue and sending them to a laboratory for testing is the only method that allows you to make an accurate diagnosis and determine whether suspicious areas are cancerous. This procedure is usually performed simultaneously with endoscopic examinations or colonoscopy.
Treatment
The acute form of severe enteritis often requires hospital observation. The hospitalization department is selected based on the form of the disease: infectious enteritis is treated in the infectious diseases department, toxic enteritis is treated in the toxicology department. In addition to conservative treatment, diet is important. Patients are prescribed a special diet with a predominance of soft, non-spicy foods with limited carbohydrates and fats, as well as drinking plenty of fluids. If the patient develops symptoms of dehydration, hydration therapy is required.
Treatment of mild forms of acute enteritis is predominantly symptomatic, aimed at alleviating the condition and reducing the risk of complications. Quite often, enteritis is accompanied by the development of intestinal microbial disorders. In this case, diarrhea is first stopped, and then measures are taken to correct the intestinal microflora. If there is a malabsorption of proteins, then the patient is administered solutions with polypeptides (simpler components of protein). On average, treatment of acute enteritis takes 5-7 days.
Hospitalization is considered mandatory for patients with poisoning, since it is difficult to predict the body’s reaction and the further development of the pathology, as well as for patients with severe infectious enteritis. In the latter case, hospitalization is required at least until the pathogen is identified.
During the period of remission, you also need to follow a diet, but less strict. During this period, all the nutrients the body needs must be supplied with food. If necessary, enzyme preparations are prescribed, as well as medications to improve absorption.
Prevention of enteritis consists of following the rules of personal hygiene, proper preparation of food (this will help protect against the infectious form of the disease), as well as following recommendations for a healthy diet.
You can conduct an examination and begin treatment at the CELT multidisciplinary clinic. Modern equipment and advanced techniques used by highly qualified specialists are the key to good health and excellent well-being.
Stages of small bowel cancer
After a person is diagnosed with small intestine cancer, doctors determine the stage of the disease - find out how far it has spread and what tissues it has damaged. Staging allows specialists to correctly assess the situation, imagine the patient’s approximate prognosis and select the most appropriate treatment for him.
For these purposes, the American TNM system is used, each letter of the abbreviation of which describes tissue damage:
- T the
main tumor; - N
describes the condition of the lymph nodes - small organs of the lymphatic system. The lymphatic system complements the cardiovascular system. The lymph circulating in it - the intercellular fluid - washes all the cells of the body and delivers the necessary substances to them, taking away waste. In the lymph nodes, which act as “filters,” hazardous substances are neutralized and removed from the body, retaining and neutralizing hazardous substances; - M1
indicates the presence, and
M0
- the absence of metastases - additional foci of cancer in other organs located far from the main tumor.
As a rule, cancer begins to develop in the mucous membrane
– the inner lining of the intestine, and as it grows it damages the deeper layers:
- second , the submucosa
, consisting of connective tissue; - muscular
, contracting to move food; - subserous
and
serous
, or visceral peritoneum - thin films covering the gastrointestinal tract.
Doctors distinguish 5 stages of adenocarcinoma: 0: tumor cells are present only in the epithelium - the upper layer of mucosal cells. I: they have penetrated deep into the first or second layers of the organ wall. IIA: muscular or subserous membranes are damaged. IIB: the visceral peritoneum or tissues located next to the intestines are damaged. IIIA: Cancer is found in 1 or 2 nearby lymph nodes. IIIB: cancer is present in 3 or more lymph nodes. IV: metastases have appeared in the body - additional tumors in other organs or tissues located far from the small intestine.
Diagnosis of irritable bowel syndrome
If you have all the symptoms of the disease listed above, consult a physician. He will conduct an initial examination and refer you to a gastroenterologist. The purpose of primary diagnosis is to exclude the presence of other life-threatening diseases: tumors, inflammatory processes, growths, infectious diseases.
When visiting a doctor, you need to provide a complete medical history, report the presence and frequency of symptoms, and talk about the presence of chronic diseases. After examination and palpation (feeling), the specialist will refer you for laboratory tests, including:
- General blood analysis. The analysis allows you to determine whether an inflammatory process is present in the body, as well as to determine possible anemia.
- General urine analysis. Determines the presence or absence of blood and parasites in the patient’s body, which allows us to talk about the development of a number of intestinal diseases other than irritable bowel syndrome.
- Blood test for celiac disease. A specific blood test that allows you to identify a disease of the digestive system (celiac disease), in which the intestines cease to properly digest incoming food, which is accompanied by diarrhea.
- Colonoscopy. This is an examination of the colon from the inside using a special device (colonoscope).
- Magnetic resonance imaging of the pelvis and abdomen. This is a non-invasive examination method that allows you to study the structure and condition of the organs and tissue of the pelvis in men and women using magnetic waves.
After all the studies have been carried out and all other intestinal diseases have been excluded, the doctor begins treatment and prescribes complex therapy, based on the patient’s medical history.
Treatment of small intestine cancer
Treatment of any type of oncology is a complex task, the solution of which requires several doctors: a surgeon, gastroenterologist, radiologist, chemotherapy and others.
Onco has a whole team of world-class specialists who care for the patient completely - from examination and diagnosis to prescribing and carrying out any therapy. With us, you don’t have to wonder “what to do next?” – we draw up a clear action plan and carry out all the necessary interventions on time – without queues, delays or wasted time.
Therapy is selected for each person individually - it depends on his age, general health, as well as the type and stage of the disease.
The main treatment for this type of cancer is surgery
. The neoplasm is removed completely if it is located only in the place where it originated - in the small intestine or the tissues closest to it. As it grows and the changed cells spread throughout the body, such an intervention alleviates the patient’s condition and reduces the symptoms caused by the blockage of the digestive system.
Chemotherapy
– introduction into the body of special drugs that enter the bloodstream and destroy cancer cells in any part of the body. It is prescribed in several situations:
In the case of adenocarcinoma of the small intestine, which is not very sensitive to “chemistry,” drugs such as Capecitabine, 5-fluorouracil, Oxaliplatin and Irinotecan are often used. Since these substances affect not only cancer cells, but also healthy cells, people who take it often develop severe side effects. The most common ones are nausea and vomiting, loss of appetite, hair loss, mouth ulcers, diarrhea, shortness of breath - feeling short of breath, bleeding or bruising from minor cuts or injuries, and constant fatigue.
Radiation therapy
– destruction of the tumor using radiation. This method is prescribed to destroy remaining cancer cells after surgery and as palliative treatment. The goal of such an intervention is to alleviate the patient’s condition and improve his quality of life - stopping bleeding or reducing pain. Before it is carried out, a team of specialists makes careful measurements: they find the correct angles at which the rays are delivered and select the exact dose for each individual person. The procedure itself lasts only a few minutes and does not cause discomfort. Its main side effects are fatigue, nausea and vomiting, diarrhea, and skin changes in the treated area such as redness, peeling or blistering.
Immunotherapy
– taking medications that strengthen a person’s own immunity and help him detect and destroy cancer cells.
Be sure to inform your doctor about any changes in your health - he will select the most suitable treatment regimen for you or prescribe medications that will alleviate your condition.
Oncoproctology department of the oncology center Lapino 2
Treatment of operable and inoperable small intestinal cancer
Treatment methods for this type of cancer depend on the possibility of complete surgical removal of the tumor.
Operable neoplasms
– those that can be completely cured with surgery are removed along with a small amount of nearby healthy tissue:
- when it is located in the first part of the organ, pancreatoduodenectomy is usually performed - resection of the head of the pancreas and duodenum;
- if it is detected in the final section, as a rule, removal of part of the colon is required;
- if the cancer is located in other areas of the small intestine, the patient is prescribed resection of the area containing the altered cells.
If nearby lymph nodes are damaged, your doctor may recommend chemotherapy or radiation therapy to kill any damaged cells remaining in the body.
Inoperable
Tumors are considered to be those that have damaged nearby tissue, spread to other organs, or are found in a person unable to undergo major surgery. In such cases, it is possible to carry out chemotherapy, radiation or immunotherapy to stop the growth of the tumor, slow down its development, reduce symptoms and improve the patient’s quality of life.
What is the problem
Malabsorption, or malabsorption in the intestine, is a malfunction in the functioning of this organ, which is manifested by a number of symptoms resulting from a violation of the digestive and transport functions of the small intestine. This definitely affects metabolism. Malabsorption syndrome is often congenital and manifests itself in children in the first 10 years of life. But there are also cases of acquired disease.
Article on the topic The intestines have neurosis. How to properly treat irritation?
Diagnosis directly depends on symptoms. So, for example, if the clinical manifestations of the congenital variant and the moderate and severe form of the acquired variant can actively manifest themselves, then the latent forms of the syndrome do not have clear manifestations and require a different diagnostic approach.
Prognosis and survival for small intestinal cancer
The outlook for each person is individual and depends on a large number of factors - age, general health, type of disease, its stage and response to treatment.
To understand the approximate prognosis for cancer development, doctors use a special term - “five-year survival rate”. It doesn’t say anything about the chances of a particular patient - it’s just statistical data that shows what percentage of patients with a certain type of cancer at a particular stage remain alive 5 or more years after the tumor was discovered.
- at localized stages, while the tumor is located only in the small intestine - approximately 85%
- at regional level, when nearby tissues or lymph nodes are damaged – about 76%;
- with the spread of altered cells to organs far from the intestines, such as the liver - 42%.
For carcinoid tumors of the gastrointestinal tract: 97%, 95% and 67%, respectively. For stromal formations: 93%, 80% and 55%.
The overall five-year survival rate for small intestinal lymphoma is approximately 70%.
Currently, despite the widespread prevalence of gastroenterological diseases, diseases of the small intestine (SI) remain unknown to practicing doctors. Some of these diseases are quite common, others are extremely rare. However, knowledge of the clinical picture of these diseases and methods of therapy can in many cases cure the patient or alleviate his condition and prolong life.
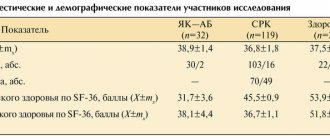
Diseases of the small intestine are characterized by specific morphological changes in the small intestinal mucosa (SIMU) of varying severity. In most cases, TC diseases have a severe, often progressive course. For 1973-2013 In the department of intestinal pathology of the Central Research Institute of Gastroenterology (TsNIIG), 1168 patients with various diseases of the colon were observed (see table).
Typical TC diseases were chronic diarrhea, malabsorption syndrome (MAS) and exudative enteropathy syndrome.
SNV is an indicator of decompensation of the digestive and transport function of the MC. The degree of its severity may change downward under the influence of treatment or increase with inadequate therapy or its absence. Malabsorption syndrome is the leading one in the clinical picture of TC diseases.
There are 3 degrees of severity of SNV [1].
I degree.
Impaired absorption is manifested mainly by a decrease in body weight (no more than 5-10 kg), decreased performance, general weakness, symptoms of vitamin deficiency, a positive symptom of “muscle roll” (an indicator of increased neuromuscular excitability due to calcium deficiency).
II degree.
More often there is a more significant deficiency of body weight (in 50% of patients more than 10 kg), severe symptoms of hypovitaminosis, electrolyte disturbances (potassium, calcium deficiency), hypochromic anemia, and in some patients - hypofunction of the endocrine glands, mainly the genitals.
III degree.
Body weight deficiency of more than 10 kg in the vast majority of patients. All patients have severe symptoms of polyhypovitaminosis, disorders of water and electrolyte metabolism (hypokalemia, hypocalcemia, convulsions, in some cases - osteopenia, osteoporosis), anemia, hypoferremia, hypoproteinemia, hypoproteinemic edema, dysfunction of the endocrine system (polyglandular insufficiency).
In a number of pathological conditions, increased losses of plasma proteins in the gastrointestinal tract (GIT) have been noted - exudative enteropathy syndrome. It is characterized by a decrease in plasma protein levels (often up to 30-40%), primarily due to a decrease in albumin levels. This syndrome differs from SNV in that with a sharp disturbance of protein metabolism (hypoproteinemia, often hypoproteinemic edema), almost no disturbances in other types of metabolism are detected.
Methods for diagnosing chronic intestinal diseases
Anamnesis
When collecting complaints, you should first of all pay attention to the nature of the stool. In chronic TB diseases, diarrhea is most often observed (it is important to take into account not only the frequency of stool, but also its daily quantity). In most cases, with chronic TB diseases, polyfecal matter with severe steatorrhea is observed. In this case, stool occurs not only during the day, but also at night. Polyfecalia with steatorrhea is most typical for patients with celiac disease, intestinal lymphangiectasia, and common variable hypogammaglobulinemia (CVGG).
Visible peristalsis is often observed with dynamic intestinal obstruction in patients with celiac disease and OVGG. Chronic partial intestinal obstruction develops most often as a result of stenosis of the area
TC - with organic damage by a tumor process, Crohn's disease.
When collecting an anamnesis, it is necessary to clarify the time of appearance of the first clinical symptoms - from early childhood (with typical celiac disease, primary lymphangiectasia), in women (connection with gynecological history: exacerbations associated with pregnancy, the postpartum period, which is typical for celiac disease). It is important to clarify the presence of a history of repeated infectious diseases (chronic bronchitis, pneumonia, sinusitis, otitis), which is typical for immunological deficiency (IVGG).
Objective examination
When examining the abdominal cavity in patients with SNV of I and II severity, it is relatively rare to suspect TC involvement. Sometimes there is bloating around the navel (a symptom of a knocked over pot). On palpation, the sound of splashing and rumbling in the cecum is most often detected (Obraztsov’s symptom).
In patients with severe malabsorption in the small intestine (with SNV of severity III), the abdomen is often enlarged, swollen, and flattened in a “frog” shape.
Palpation creates a feeling of “doughiness” and fullness of the abdominal cavity. Splashing and rumbling on palpation are detected not only in the blind, but also in the loops of the TC. Severe INV can be objectively expressed only by loss of body weight. An objective examination can reveal dryness and flaking of the skin, changes in its color (dirty gray tint, age spots on the face, pigmentation of the arms, hands, face and neck, diffuse pigmentation of the skin, especially pronounced in areas exposed to light and friction). Weeping cracks may appear in the corners of the mouth, less often behind the ears and at the wings of the nose. Nails become dull, thinned, cross-striated, flake, and sometimes take the shape of “watch glasses.” There is thickening of the terminal phalanges on the hands (symptom of “drum fingers”).
Symptoms of increased bleeding may appear in the form of petechial or subcutaneous hemorrhages (nasal, gum, uterine, hematuria, gastrointestinal). The language changes. It may be loose, swollen with teeth marks along the edges. In other cases, atrophy of the papillae may occur and then the tongue becomes smooth, as if polished, sometimes crimson-red in color.
Increased neuromuscular excitability often occurs, which is revealed by the positive symptom of a “muscle roll” (convulsive contraction of the biceps brachii muscle when irritated by pinching or tapping). With hypoproteinemia (SNV III severity), swelling of the legs, feet, thighs, and anterior abdominal wall may appear. The most pronounced edema, which occurs before other clinical manifestations of SNV, is observed in the syndrome of exudative enteropathy. Patients often experience severe hypotension [2].
Laboratory methods characterizing metabolic disorders in the body
In TC diseases, the level of hemoglobin in the blood is important. Celiac disease is characterized by the development of iron deficiency anemia. Some TC diseases can be complicated by blood loss (ulcerative jejunoileitis, intestinal angiodysplasia). In severe forms of malabsorption syndrome, mixed anemia (B12-folate-iron deficiency) often develops.
Biochemical blood tests reveal deviations from the norm only in patients with SNV of II-III severity. Hypoproteinemia due to hypoalbuminemia, hypocholesterolemia, hypocalcemia, hypokalemia, hypomagnesemia, hypoferremia may be observed.
In patients with SNV II and III severity, immunoglobulins of all classes are determined in order to diagnose OVGG or isolated IgA deficiency, and antibodies to gliadin, endomysium, tissue transglutaminase, deamidated gliadin peptide of the IgA class are also determined to identify patients with suspected celiac disease [3]. In case of heavy α-chain disease (Mediterranean lymphoma), pathological IgA, whose molecules consist only of heavy α-chains, is detected at an early stage.
Determining the daily amount of feces is of important diagnostic importance. Normally, it does not exceed 200-300 g, and in case of TC diseases it is often 1000-1500 g/day.
If a helminthic or parasitic infestation is suspected, repeated stool tests are performed for protozoan eggs and worm eggs. Determining blood loss through the gastrointestinal tract is of important diagnostic importance, and therefore it is necessary to re-examine stool for the presence of blood pigment.
Microscopic examination of undigested food debris in feces is usually not informative enough. However, it is necessary to pay attention to the presence of undigested fat and large amounts of fatty acids in the feces, which may indirectly indicate a violation of the digestion and absorption of lipids.
Endoscopic examination of the small intestine
Esophagogastroduodenoscopy
with a biopsy from the descending part of the duodenum followed by a morphological study of biopsies of the mucous membrane is used in the diagnosis of patients with celiac disease, Whipple's disease, intestinal lymphangiectasia, and common variable immunodeficiency. Colonoscopy with examination of the terminal ileum is used to diagnose Crohn's disease of the ileum, tuberculous ileotiphlitis, and yersiniosis.
Capsule endoscopy
- a modern method for studying the gastrointestinal tract, which makes it possible to visualize areas of the intestine that are inaccessible to traditional methods of gastro- and colonoscopy. Used for bleeding to identify the source of bleeding, diagnose Crohn's disease TK, lymphoma.
Double balloon enteroscopy
allows you to examine deep areas of the small intestine and, if necessary, take a biopsy of the intestine. This method of endoscopic examination is used to determine the source of bleeding, diagnose Crohn's disease, tumors of the breast, or clarify the nature of the developmental anomalies of the breast revealed by X-ray examination.
X-ray examination of the TC
Despite the increasingly widespread use of double-balloon endoscopy, video capsule, computed tomography and magnetic resonance enterography, conventional X-ray examination of the colon (studying the passage of barium suspension after oral administration from entry into the duodenum to filling the ileocecal region) is an informative method with high sensitivity and specificity, allows you to assess the functional state of the MC (tone, peristalsis, speed and nature of filling), identify intestinal hypersecretion, and assess the condition of the mucous membrane. These changes are non-specific and complement the clinical understanding of the severity of TC lesions and the extent of changes.
With mild lesions of the TC, dyskinesias are observed - hypo-, hypermotor or hyperhypomotor. Violations of tone are observed less frequently and manifest themselves in uneven filling of the TC with barium, regional hypotension or spasms. In severely ill patients, in some cases with pronounced changes in tone and intestinal hypersecretion, horizontal levels of liquid and gas are found in individual intestinal loops.
Changes in the relief of the mucous membrane are characterized by persistent deformation in the form of rough, wide folds of Kerkring (the result of total edema and swelling of the mucous and submucosal layers), as well as uneven accumulations of barium between the changed folds of the mucous membrane after bowel movement. These changes in all diseases are most pronounced during periods of exacerbation and can gradually disappear with long-term stable remission.
If an organic lesion of the mast cell is suspected, it is necessary to additionally study radiological changes in the mast cell under probe enterography.
The method of probe enterography involves inserting a probe and placing the olive behind the duodenal flexure in the proximal loop of the jejunum. Through a probe, with the patient in the supine position, about 600-800 ml of barium suspension is gradually introduced. Then, to obtain a double-contrast picture, 400-800 ml of air is injected through the probe. To ensure artificial hypotension of the TC in terms of differential diagnosis of organic changes and functional strictures, 2 ml of atropine or metacin are administered intravenously. To achieve intestinal hypotension and open the ileocecal valve, in some cases, sublingual administration of 2-3 aeron tablets is used 20 minutes before the start of the study.
Probe enterography is performed if there is a suspicion of tumors, lymphogranulomatosis, lymphoma of the intestine and lymph glands of the abdominal cavity (mesenteric, retroperitoneal), Crohn's disease, tuberculous ileotiphlitis, celiac disease, Whipple's disease, intestinal lymphangiectasia.
In these cases, the X-ray method makes it possible to identify organic stenoses, intraluminal formations, persistent deformation of individual sections of the intestine, gross changes in the mucous membrane, hyperplasia of the lymphoid elements of the submucosal layer. Polycyclicity of intestinal contours is an indirect sign of enlarged lymph nodes. Severe damage to the upper parts of the colon and the absence of changes in the ileum are much more common than in other diseases in celiac disease.
With tumors of the colon, filling defects, invaginations, circular narrowing of the intestinal lumen, deformation of the relief of the mucous membrane, rigidity of the shadow of the intestinal walls and the tumor itself are observed radiologically. In patients with lymphomas, the intestine has polycyclic contours due to external compression by enlarged lymph nodes [4, 5]. However, enlargement of mesenteric and retroperitoneal lymph nodes in lymphomas and other intestinal neoplasms is more often detected during computed tomography.
Ultrasound examination of the intestines
Ultrasound examination (ultrasound) of the TC is performed 4 hours after eating. Used for suspected neoplasm, Crohn's disease. Allows to identify focal or diffuse thickening of the walls of the colon, pathological narrowing of the lumen, pseudopolyposis, characteristic of Crohn's disease. This diagnostic method helps to detect cancer pathology in the early stages of the disease.
Morphological study of SOTC
A morphological examination of biopsy specimens of SOTK is carried out for all patients with malabsorption syndrome and exudative enteropathy syndrome if the presence of celiac disease, Whipple's disease, intestinal lymphangiectasia, OVGG, eosinophilic gastroenteritis is suspected in order to clarify the diagnosis. Intestinoscopy, double-balloon enteroscopy with targeted biopsy are used for morphological examination of biopsy specimens in cases of suspected TB tumors and TB Crohn's disease.
Morphological examination for celiac disease is the “gold standard”. Pathological changes in the STC can vary widely: from minimal enteropathy with a high number of interepithelial lymphocytes to a flat surface, typical for celiac disease, penetrated by deep crypts.
The standard for assessing the severity of pathological changes in the STC and their dynamics during therapy is considered to be histological examination in accordance with the Marsh-Oberhuber classification, according to which there are 4 stages of the disease [6].
The diagnosis of collagenous sprue is made on the basis of a histological examination of the CBF, which is atrophic, and a massive layer of collagen is formed under the enterocyte membrane, aggravating the malabsorption in the TC.
In Whipple's disease, macrophages with large granules in the cytoplasm are found in the STC - the so-called CHIC-positive or RAS-positive macrophages. The same macrophages are detected in the mesenteric lymph nodes. Electron microscopy reveals microorganisms inside macrophages - Tropheryma whippelii
[7]. After treatment with antibiotics in a phase of stable remission, they disappear, and during an exacerbation they reappear.
In case of amyloidosis, the deposition of homogeneous masses in the wall of small vessels and the lamina propria with a positive stain for Congo red and a positive reaction for amyloid is observed in the CTCS. Amyloid is detected under a polarizing microscope [8].
With intestinal lymphangiectasia in the intestinal tract, dilation of the lymphatic vessels is detected in the mucosal and submucosal layers of the intestinal tract. The wall of the mesenteric lymphatic vessels is thickened, their muscle layer is hypertrophied. Dilated lymphatic vessels look like cavernous formations in the submucosal layer of the TC, sometimes in the form of “lakes” filled with thick lymph. Signs of STC atrophy are not detected.
One of the forms of OVGGG is hypogammaglobulinemic sprue, in which the symptoms of OVGGG are combined with the symptoms of celiac disease. The disease is rare. Along with the symptoms characteristic of general variable hypogammaglobulinemia, there are pronounced gastrointestinal disorders. When studying the morphological structure of SOTK, along with the absence of plasma cells characteristic of OVGG, atrophy is revealed, similar to that found in celiac disease [9].
To diagnose Crohn's disease, as a rule, a histological examination of surgical material is used, since a biopsy does not always allow a correct diagnosis. Histological examination of surgical material for Crohn's disease reveals damage to all layers of the intestinal wall. The most characteristic are swelling and hyperplasia of lymphoid elements in the form of follicles in the submucosal layer. In more than half of the cases, it is possible to detect granulomas consisting of giant Pirogov-Langhans cells surrounded by a belt of lymphocytes that do not have clear boundaries. Ulcers, intramural abscesses, and infiltration of all layers of the muscle wall with plasma cells and fibroblasts may be detected.
Thus, the difficulties in diagnosing diseases of the small intestine are largely explained by the peculiarities of the location of the organ, which is almost inaccessible for research, and the similarity of clinical syndromes. Establishing the correct diagnosis is possible by prescribing the most informative laboratory and instrumental diagnostic methods for each disease. The use of such a clinical approach makes it possible to recognize most TC diseases in a regular gastroenterology department.