Table of contents
- Etiology and pathogenesis
- Clinical manifestations
- Principles of treatment
Onychomycosis (fingernail fungus, toenail fungus) is a fungal infection of the toenails or fingernails that affects any component of the nail complex, including the base, bed or plate. The disease can be accompanied by pain, discomfort, and changes in the appearance of the nails, which in some cases leads to serious physical and professional limitations, anxiety for patients and a decrease in their quality of life.
In our company you can purchase the following equipment for the treatment of onychomycosis:
- AcuPulse (Lumenis)
In the USA, onychomycosis of the nails occurs in approximately 2–13% of the population, in Canada - in 6.5%, in England, Spain and Finland - in 3-8%. According to a systematic review of 1914 articles, the prevalence of onychomycosis is as follows:
- general population - 3.22%;
- children - 0.14%;
- elderly people - 10.28%;
- patients with diabetes mellitus - 8.75%;
- patients with psoriasis - 10.22%;
- HIV-positive patients - 10.40%;
- patients on dialysis - 11.93%;
- after kidney transplant - 5.17%.
Onychomycosis accounts for about half of all nail pathologies and is the most common nail disease in adults. As for the affected areas, statistically, the legs are affected much more often than the arms.
The main forms of onychomycosis are:
- Distal lateral subungual onychomycosis
- Proximal subungual onychomycosis
- White superficial onychomycosis
- Endonyx-onychomycosis
- Candidal onychomycosis
Often patients have a combination of these subtypes, or total dystrophic onychomycosis - damage to the entire nail complex.
Modern methods of treating onychomycosis
Onychomycosis is the most common nail disease. It has been established that 50% of cases of changes in the nail plates are associated with a mycotic infection. Epidemiological studies conducted in Russia and foreign countries have revealed a high incidence of onychomycosis, which ranged from 2 to 13% in the general population [1, 2, 3]. The risk of developing onychomycosis is highest in older patients. For example, in people over 70 years of age, the prevalence of onychomycosis of the feet can be 50% or higher [2, 4, 5]. It is believed that this is facilitated by the slow growth of nail plates and disorders of peripheral and main circulation in the elderly [6]. A high frequency of onychomycosis is also detected in patients with immunodeficiency conditions (including AIDS patients) and in patients with diabetes mellitus [6, 7, 8].
Often patients and some doctors perceive onychomycosis as an exclusively aesthetic problem. However, this is a serious disease that occurs chronically and in cases of immunodeficiency or decompensation of endocrine diseases can cause the development of widespread mycosis of the skin and its appendages. Onychomycosis is often accompanied by the development of severe complications, such as diabetic foot, chronic erysipelas of the extremities, lymphostasis, and elephantiasis [9, 10]. In patients receiving cytostatic or immunosuppressive therapy, the disease can cause the development of invasive mycoses. That is why treatment of onychomycosis is necessary and should be carried out in a timely manner [11].
Just a few decades ago, treatment of onychomycosis was labor-intensive, lengthy and unpromising. Medicines used to treat fungal diseases of the skin and its appendages were characterized by low effectiveness and high toxicity. To achieve a positive result, long-term treatment or an increase in the dose of drugs was required, which was often accompanied by severe complications. Some treatments were potentially life-threatening for patients. For example, X-ray therapy, the use of thallium and mercury led to the development of skin cancer, diseases of the brain and internal organs in patients.
The emergence of highly effective and low-toxic antimycotic drugs has greatly facilitated the treatment of fungal diseases of the skin and its appendages. However, the results of using new antimycotics were not satisfactory. Controlled clinical trials have shown that the effectiveness of systemic antimycotics after treatment is from 40 to 80%, and after 5 years - from 14 to 50% [12]. At the same time, the effectiveness of therapy for onychomycosis increases with the use of complex treatment methods, which involve the use of etiotropic drugs and agents that influence the pathogenesis [13]. Also, as a result of clinical trials conducted in European countries, it was found that the effectiveness of treatment of onychomycosis can be increased by an average of 15% with the combined use of systemic antimycotics and antifungal varnish containing amorolfine [14].
Treatment
For the treatment of onychomycosis, drugs are used that differ in chemical composition, mechanism of action, pharmacokinetics, and spectrum of antifungal activity. A common property for them is a specific effect on pathogenic fungi. This group consists of azoles (itraconazole, fluconazole, ketoconazole), allylamines (terbinafine, naftifine), griseofulvin, amorolfine, ciclopirox. To treat onychomycosis, systemic drugs are used that belong to the azole group - itraconazole, fluconazole, as well as to the allylamine group - terbinafine. Griseofulvin and ketoconazole are currently not prescribed for the treatment of onychomycosis due to low effectiveness and a high risk of adverse events. Varnishes and solutions containing amorolfine and ciclopirox are used as external agents for onychomycosis.
Allylamines are synthetic antimycotics. Allylamines primarily act on dermatomycetes, while they have a fungicidal effect. The mechanism of their action is to inhibit the enzyme squalene epoxidase, which takes part in the synthesis of ergosterol, the main structural component of the cell membrane of dermatomycetes. Allylamines include terbinafine and naftifine.
Allylamines are active against most dermatomycetes (Epidermophyton spp., Trichophyton spp., Microsporum spp., Malassezia spp.), the causative agent of chromomycosis and some other fungi.
Indications for the administration of terbinafine orally are onychomycosis, common forms of dermatomycosis of the skin, mycosis of the scalp, chromomycosis. Indications for external use of terbinafine and naftifine include limited skin lesions due to mycoses, pityriasis versicolor, and skin candidiasis. Terbinafine has high bioavailability and is well absorbed from the gastrointestinal tract regardless of food intake. In high concentrations, the drug accumulates in the stratum corneum of the skin, nail plates, hair, and is secreted with the secretions of the sweat and sebaceous glands. Absorption of terbinafine when applied topically is less than 5%, naftifine - 4-6%. The concentration of terbinafine and naftifine in the skin and its appendages significantly exceeds the MIC for the main pathogens of dermatomycosis. Correction of the terbinafine dosage regimen may be required when combined with inducers (rifampicin) or inhibitors of microsomal liver enzymes (cimetidine), since the former increase its clearance, and the latter reduce it.
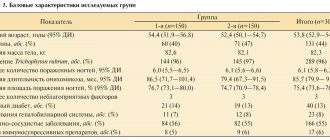
As a result of numerous controlled multicenter comparative clinical trials, it was found that terbinafine is the most effective antimycotic in the treatment of onychomycosis [12] (Table 1).
| Table 1. Comparative effectiveness of antimycotics in the treatment of onychomycosis (based on the results of a meta-analysis of 27 randomized studies) |
Terbinafine is used for widespread skin lesions, onychomycosis, chromomycosis, in such cases terbinafine is prescribed orally. Terbinafine is the drug of choice in the treatment of onychomycosis, as it is most effective against the main causative agents of onychomycosis - dermatomycetes. Contraindications for the use of allylamines are allergic reactions to drugs of the allylamine group, pregnancy, breastfeeding, age under 2 years, liver diseases accompanied by impaired liver function (increased transaminases).
Azoles are the largest group of synthetic antimycotics. In 1984, the first systemic antifungal drug from the azole group, ketoconazole, was introduced into practice, in 1990, fluconazole, and in 1992, itraconazole.
Azoles used as systemic drugs have predominantly fungistatic activity. An important advantage of azoles over other drugs is their wide spectrum of antifungal activity. Itraconazole is active in vitro against most pathogens of onychomycosis - dermatomycetes (Epidermophyton spp., Trichophyton spp., Microsporum spp.), Candida spp. (C. albicans, C. parapsilosis, C. tropicalis, C. lusitaniae, etc.), Aspergillus spp., Fusarium spp., S. Shenckii, etc. Fluconazole is active against dermatomycetes (Epidermophyton spp., Trichophyton spp., Microsporum spp. .) and Candida spp. (C. albicans, C. parapsilosis, C. tropicalis, C. lusitaniae, etc.), but does not affect Aspergillus spp., Scopulariopsis spp., Scedosporium spp.
The pharmacokinetics of different azoles is different. Fluconazole (90%) is well absorbed from the gastrointestinal tract. For good absorption of itraconazole, a normal level of acidity is necessary. If a patient taking these drugs has low acidity, their absorption decreases and, consequently, their bioavailability decreases. The absorption of itraconazole solution is higher than that of itraconazole capsules. Itraconazole capsules should be taken with food, and Itraconazole solution should be taken on an empty stomach.
Itraconazole is metabolized in the liver and excreted from the body through the gastrointestinal tract. It is also secreted in small quantities by the sebaceous and sweat glands. Fluconazole is partially metabolized and is mainly excreted unchanged by the kidneys (80%).
Itraconazole interacts with many drugs. The bioavailability of ketoconazole and itraconazole decreases when taking antacids, anticholinergics, H2 blockers, proton pump inhibitors, and didanosine. Itraconazole is an active inhibitor of cytochrome P450 isoenzymes and can alter the metabolism of many drugs. Fluconazole affects drug metabolism to a lesser extent. It is unacceptable to take azoles with terfenadine, astemizole, cisapride, quinidine, as deadly ventricular arrhythmias may develop. Concomitant use of azoles and oral antidiabetic drugs requires constant monitoring of blood glucose levels, as hypoglycemia may develop. Taking indirect anticoagulants of the coumarin and azoles group may be accompanied by hypocoagulation and bleeding; therefore, hemostasis control is necessary. Itraconazole can increase the blood concentration of cyclosporine and digoxin, and fluconazole - theophylline and cause the development of a toxic effect. Dose adjustments and constant monitoring of drug concentrations in the blood are required. The combined use of itraconazole with lovastatin, simvastatin, rifampicin, isoniazid, carbamazepine, cimetidine, clarithromycin, erythromycin is contraindicated. Fluconazole should not be used with isoniazid and terfenadine.
Itraconazole is used for dermatomycosis (athlete's foot, trichophytosis, microsporia), pityriasis versicolor, candidiasis of the skin, nails and mucous membranes, esophagus, vulvovaginal candidiasis, cryptococcosis, aspergillosis, phaeohyphomycosis, sporotrichosis, chromomycosis, endemic mycoses, for the prevention of myco call for AIDS.
Fluconazole is used for the treatment of generalized candidiasis, all forms of invasive candidiasis, including in immunocompromised patients, genital candidiasis, candidiasis of the skin, its appendages and mucous membranes. Recently, due to its safety and good tolerability, fluconazole is increasingly used for the treatment of patients with dermatomycosis with damage to both the skin and its appendages (nails and hair).
Amorolfine is part of a varnish used to treat onychomycosis. The mechanism of action of amorolfine is to disrupt the synthesis of ergosterol, the main component of the cell membrane of the fungus. It has fungistatic and fungicidal effects. Has a wide spectrum of action. The concentration of amorolfine in the nail plate significantly exceeds the MIC for the main pathogens of dermatomycosis for 7 days. Therefore, the drug can be applied no more than 1–2 times a week, which makes its use economically profitable. Contraindications: allergic reactions to amorolfine, infancy and young children. Varnish as monotherapy is prescribed when no more than 1–3 nail plates are affected and no more than 1/2 of the area from the distal end is affected. Amorolfine can also be used in combination with systemic antimycotics for more widespread nail lesions (Table 2).
Ciclopirox has a fungistatic effect. Active against dermatomycetes, yeast-like and filamentous fungi, molds, as well as some gram-negative and gram-positive bacteria. Ciclopirox (varnish) is used as monotherapy when no more than 1-3 nail plates are affected by no more than 1/2 of the area from the distal end. Ciclopirox can also be used in combination with systemic antimycotics for more widespread nail damage. Contraindications: allergic reactions to ciclopirox, infancy and early childhood, pregnancy and lactation.
List of recommended laboratory tests when prescribing systemic antifungal drugs.
- Clinical blood test.
- General urine analysis.
- Biochemical blood test (ALT, AST, bilirubin, creatinine).
- Ultrasound of the abdominal organs and kidneys (preferred).
- Pregnancy test (preferred).
Treatment of underlying diseases. The effectiveness of the use of antimycotics increases with the correction of pathological conditions that contribute to the development of onychomycosis. Before starting antimycotic therapy in patients with somatic, endocrine, neurological diseases, and with circulatory disorders in the extremities, it is necessary to conduct an examination to identify the main symptom complex that contributed to the development of dermatomycosis. Thus, the main objectives of pathogenetic therapy are to improve microcirculation in the distal parts of the extremities, venous outflow of the extremities, normalize the level of thyroid-stimulating hormones in patients with thyroid diseases, carbohydrate metabolism in patients with diabetes mellitus, etc. As a result of many years of research conducted at the Military Medical Academy and St. Petersburg Medical Academy of Postgraduate Education, it has been established that one of the main causes of the development of dermatomycosis is disorders of the pituitary-hypothalamus-gonadal system. This leads to circulatory disorders in the distal extremities, microcirculation disorders, and peripheral innervation. A set of measures aimed at correcting these disorders includes acupuncture, transcranial electrical stimulation of the subcortical centers of the brain, and the prescription of drugs that correct the functioning of the sympathetic and parasympathetic autonomic nervous system. All this makes it possible to achieve a faster clinical effect in the treatment of dermatomycosis. It is advisable to prescribe pathogenetic therapy in patients with dermatomycosis with underlying diseases before the start of etiotropic treatment and continue it during the entire course of taking antifungal drugs.
Symptomatic therapy of dermatomycosis, aimed at reducing subjective complaints of patients and objective manifestations of the disease, cannot replace etiotropic therapy. However, its use in combination with antifungal drugs makes it possible to quickly improve the condition of patients, reduce the feeling of discomfort and eliminate cosmetic defects. With onychomycosis, the greatest concern for patients is caused by deformed, significantly thickened (hypertrophied) nail plates - onychogryphosis. To correct this condition, hardware pedicure is used. Using a device that resembles a dental turbine, in a short period of time, altered areas of the nails, hyperkeratotic areas, horny masses from the skin, and calluses are mechanically removed. In this case, there is no trauma to the nail matrix, and the patient remains functional after the procedure.
For limited damage to nails (no more than 3 nail plates and no more than 1/2 in area from the distal edge), topical preparations are used. It is recommended to begin treatment by cleaning the affected area of the nail plate using the Mycospor set, hardware pedicure or keratolytic agents. Next, antifungal drugs are applied to the affected nail plate. An amorolfine solution containing ciclopirox is applied to the nail plate 1–2 times a week. Before applying the varnish, you do not need to first clean the nail plate of previous layers of the preparation. The varnish is applied daily until the healthy nail plate grows completely. On the 7th day, the nail plate is cleaned using any cosmetic nail polish remover. There are conflicting reports in the literature about the effectiveness of this treatment method. The percentage of cure for patients is indicated from 5–9 to 50%.
In case of widespread damage to the nail plates on the fingers, a complex of treatment measures should include the prescription of a systemic antimycotic, cleaning of the nails and external therapy with antifungal drugs. In order to prevent re-infection, it is necessary to treat the patient’s gloves and disinfect personal hygiene items (washcloths, towels, nail files, graters and scrapers for treating skin and nails).
The drug of choice for the treatment of onychomycosis of any localization is terbinafine. It is prescribed to adults and children weighing more than 10 kg, 250 mg per day for 6 weeks. Children over 2 years old weighing less than 20 kg are prescribed terbinafine at the rate of 67.5 mg/kg per day, from 20 to 40 kg - 125 mg/kg per day for 6 weeks. Reserve drugs are products containing itraconazole and fluconazole. Itraconazole is used in two regimens: 200 mg daily for 3 months or 200 mg twice daily for 7 days in the first and fifth weeks from the start of therapy. Itraconazole is not prescribed for the treatment of onychomycosis in children. Fluconazole is recommended to be taken 150 mg once a week for 3–6 months.
Carrying out complex therapy, consisting of taking a systemic antimycotic, cleaning nails, local use of antifungal drugs, as well as anti-epidemiological measures, ensures high efficiency in curing onychomycosis of the feet. Terbinafine is prescribed to adults and children weighing more than 10 kg, 250 mg per day for 12 weeks or more. For children over 2 years old weighing less than 20 kg, the drug is prescribed at the rate of 67.5 mg/kg per day, from 20 to 40 kg - 125 mg/kg per day for 12 weeks. Fluconazole is recommended to be used at a dose of 150–300 mg once a week for 6–12 months. Itraconazole is used in two regimens: 200 mg daily for 3 months or 200 mg twice daily for 7 days in the first, fifth and ninth weeks. If the big toes are affected, it is recommended to carry out the 4th course of pulse therapy in the thirteenth week from the start of therapy. Itraconazole is not used for the treatment of onychomycosis in children.
The criteria for mycological cure of onychomycosis are negative results of microscopic and cultural examination of the nail plate. After treatment with itraconazole and terbinafine, healthy nail plates do not grow back completely, so complete clinical recovery can be observed only 2–4 months after the end of taking antifungal drugs.
Literature
- Kornisheva V. G. Mycoses of the skin and subcutaneous tissue, clinical pathogenesis, treatment: abstract. Dis... Dr. med. Sci. St. Petersburg, 1998. 34 p.
- Levy A. Epidemiology of onychomycosis in special-risk populations // J. Am. Podiatr Med. Assoc. 1997; 87:546–550.
- Herikkila H., Stubb S. The prevalence of onychomycosis in Finland // BJ Dermatol. 1995; 133:699–703.
- Rukovishnikova V. M. Mycoses of the feet. M., 1999. 317 p.
- Sergeev Yu. V., Sergeev A. Yu. Onychomycosis. Fungal nail infections. M.: GEOTAR - Medicine, 1998. 126 p.
- Cribier BJ, Bakshi R. Terbinafin in treatment of onychomycosis: a review of its efficacy in high-risk populations and in patients with nondermatophyte infections //BJ Dermatol. 2004; 150: 414–420.
- Yosipovitch G., Hodak E., Vardy P. et al. The prevalence of cutaneous manifestations in IDDM patients and their association with diabetes risk factors and microvascular complications // Diabetes Care. 1998; 21:506–509.
- Rich P. Special patient population: onychomycosis in the diabetic patient // J. Am. Acad. Dermatol. 1996; 35: 10–12.
- Lykova S. G., Nemchaninova O. B., Petrenko O. S., Borovitskaya O. N. Rational antimycotic therapy of foot mycoses in patients with metabolic syndrome // Russian Journal of Skin and Venereal Diseases. 2005. No. 6. P. 58–60.
- Sotirion E., Konssidon-Eremondi Th., Kastoridon Ch. et al. Erysipelas and tinea pedis: a 4 year review // JEADV 2004; 18 (2): 385.
- Kornisheva V.G., Shlyapnikov S.A., Nasser N.R., Pak E.Yu. Frequency of occurrence of mycoses of the feet in patients with erysipelas of the lower extremities // Problems of medical mycology. 2005. T. 7. No. 2. P. 51–52.
- Gupta AK, Ryder C., Johnson S. Cumulative meta-analysis of systemic antifungal agents for the treatment of onychomycosis // Br J Dermatol. 2004; 150:537–544.
- Raznatovsky K.I., Rodionov A.N., Kotrekhova L.P. Dermatomycoses. St. Petersburg: Publishing house SPbMAPO, 2003. 159 p.
- Baran R., Feuilhade M., Datry A. et al. A randomized trial of amorolfine 5% solution nail lacquer combined with oral compared with terbinafine alone in the treatment of dermatophytic toenail onychomycosis affecting the matrix region //Br J Dermatol. 2000; 142:1177–1183.
L. P. Kotrekhova , Candidate of Medical Sciences, Associate Professor K. I. Raznatovsky , Doctor of Medical Sciences, Professor N. N. Klimko , Doctor of Medical Sciences, Professor of St. Petersburg Medical Academy of Postgraduate Education, St. Petersburg
Etiology and pathogenesis of onychomycosis
Onychomycosis is caused by three main classes of fungi: dermatophytes, yeasts, and nondermatophytic molds.
Dermatophytes are the most common cause of the disease. Two main pathogens are responsible for 90% of all cases of onychomycosis: Trichophyton rubrum (70%) and Trichophyton mentagrophytes (20%). Onychomycosis, caused by non-dermatophytic mold fungi of the genera Fusarium and Aspergillus, as well as Scopulariopsis brevicaulis, is an anamorphic (asexual) representative of the genus Ascomycota, is gradually spreading throughout the world. Today they are responsible for 10% of cases of the disease. As for candidal onychomycosis, it is caused by Candida albicans and is quite rare.
In distal lateral subungual onychomycosis, Trichophyton rubrum is usually detected. Proximal subungual onychomycosis is typical in immunocompromised patients . The same type of onychomycosis, but with periungual inflammation, is caused by non-dermatophytic molds. White superficial onychomycosis of the nails is caused by Trichophyton mentagrophytes, and its deeper forms are caused by non-dermatophytic molds. Candida nail infection is often observed in premature infants, immunocompromised patients, and individuals with chronic mucosal candidiasis.
Risk factors for developing onychomycosis:
- family history;
- elderly age;
- warm and humid climate;
- weakened body;
- nail injury;
- regular fitness classes;
- immunosuppression (drug, HIV, etc.);
- visiting public swimming pools, baths and saunas;
- tight shoes.
Repeated microtrauma of the nails in tight and uncomfortable shoes provokes onycholysis (detachment of the nail from the soft tissues of the finger) and other degenerative conditions that contribute to the penetration of fungi into the nails.
Diagnosis of onychomycosis
Treatment of nail fungus begins with a diagnostic examination aimed at identifying the pathogen and includes a number of stages:
- medical examination and collection of information about the patient’s living conditions and medical history;
- microscopic examination of samples of affected nails, nail scrapings and subungual contents;
- bacteriological culture with determination of its type and sensitivity to antifungal drugs.
To distinguish fungal nail infections from non-infectious onychodystrophy, which is similar in symptoms, a comprehensive differential diagnosis is carried out.
Clinical manifestations of nail onychomycosis
At first, onychomycosis is asymptomatic - patients can see a doctor because of visible cosmetic defects of the nail plate, but without any discomfort. As the disease progresses, paresthesia, pain and discomfort occur in the affected area. This makes walking difficult and interferes with sports and everyday life.
Clinical manifestations of onychomycosis depend on its type:
- Distal lateral subungual onychomycosis - there is subungual hyperkeratosis and onycholysis, the plate becomes yellow-white. In its central part, yellow stripes and/or yellowish onycholytic areas are visible.
- Proximal subungual onychomycosis - represented by leukonychia (white spots and stripes) in the proximal parts of the nail plate, which move distally (towards the edge) as the nail grows. If mold fungi are among the pathogens, periungual inflammation occurs.
- White superficial onychomycosis - small white speckled spots form on the toenails, the nail plate becomes rough and crumbles easily. Variations are possible with a deeper spread of the pathological process into the nail, depending on the causative agent of the disease.
- Endonyx-onychomycosis - the color of the nail plate becomes milky white. Unlike distal onychomycosis, there are no signs of subungual hyperkeratosis or onycholysis.
- Candidal onychomycosis of the nails is associated with chronic mucocutaneous candidiasis or immunosuppression, in which several or all nails are affected at once with the presence of periungual inflammation. The fingers of such patients often take on the shape of a bulb or drumsticks.
To assess the severity of the disease, the Onychomycosis Severity Index (OSI) has been developed. The result is obtained by multiplying the lesion area scores by the proximity scores of the lesion to the nail growth zone. Mild degree – 1–5 points, moderate – 6–15, severe – 16–35. Dermatophytoma (spots or longitudinal stripes) more than 2 mm with subungual hyperkeratosis is scored 10 points.
In its manifestations, onychomycosis is similar to many other nail pathologies. For example, leukonychia (stripes) resemble trauma to the nail plate. To confirm the diagnosis, it is necessary to perform a laboratory mycological study. Interestingly, a negative result does not rule out onychomycosis, since microscopy can be false negative in 10% of cases and culture in 30% of cases. A more reliable, although more expensive, method is PCR research (polymerase chain reaction).
Rice. 1. Distal lateral subungual onychomycosis (Dr. Antonella Tosti)
Rice. 2. Proximal subungual onychomycosis (Dr. Antonella Tosti)
Rice. 3. White superficial onychomycosis (Dr. Antonella Tosti)
Rice . 4. Endonyx-onychomycosis (Piraccini B., Alessandrini A. Onychomycosis: A Review. J Fungi 2015; 1: 30–43)
Rice. 5. Candidal onychomycosis (Dr. Antonella Tosti)
What is nail fungus?
Mycoses are a collective concept that unites a wide group of diseases caused by various types of opportunistic and pathogenic fungi.
Due to the nature of their work, specialists at the Clinic of Podology have to deal with three types of pathogens that provoke fungus of the nails and skin of the feet:
- yeast-like;
- moldy;
- dermatophytes.
Most often, fungal infection of the nails (onychomycosis) occurs in older people, and in men it is 2-3 times more common than in women. Factors that can provoke the development of the disease include vascular pathologies, obesity and foot diseases. In addition, nail plate fungus is detected in 1/3 of patients with diabetic foot syndrome developing against the background of diabetes mellitus.
The introduction of a fungal pathogen can be caused by calluses, corns, flat feet, valgus deformity of the big toes (“bunions”), excessive dryness or excessive sweating of the skin and constant trauma to the feet. An important role in the development of the infectious process is played by insufficient adherence to the rules of personal hygiene when visiting swimming pools, saunas, baths, fitness centers and other public places with high humidity and air temperature, which are favorable for infection with mycosis.
Treatment of nail fungus with innovative PinPointe laser
The Podology Clinic uses the latest nail treatment method using the PinPointe FootLaser micropulse laser. The treatment is quick, painless and guarantees complete elimination of the fungus. But most importantly, laser therapy allows you to do without removing the nail plate!
During the treatment, laser pulses delivered by beams heat the nail to 79° and destroy the causative agent of the disease after the first procedure. Pulse modulation ensures uniform heating of the treated area and prevents burns to the tissues of the nail fold.
Important! Failure to follow recommendations and deviation from the treatment plan will not only not bring the desired result, but can also lead to progression of the disease.
If you are faced with a fungal infection, do not despair and hide your nails from prying eyes in closed shoes. Podology Clinic specialists will help you find a safe and effective solution to your problem and return your feet to a healthy and well-groomed appearance!
Video review of the PinPointe FootLaser laser and interview with Dmitry Zakharchenko (CEO) on the latest device for treating onychomycosis:
Single and double pulse technology
ALMA-Q operates in standard and quasi-long-pulse modes, emitting laser energy using “flat beam profile” technology. In this case, the peak energy in a pulse can reach up to 2 J. The flat profile of the beam helps, even at maximum peak power, to evenly distribute energy in the working spot and minimize the risk of damage to the epidermis. Single and dual pulse modes are available for all ALMA-Q Q-switch Nd:YAG laser wavelengths, including 1064 nm, 532 nm, 585 nm and 650 nm.
Prevention of nail fungus
It is more rational to adhere to simple rules of prevention now than to treat nail fungus in the future.
- Regularly check and inspect your nails, feet, and skin between your toes for spots, peeling, and cracks.
- Be responsible when purchasing shoes - they should be moderately loose, made from natural materials that allow air circulation.
- Use replaceable shoes in public places, such as: bathhouse, sauna, swimming pool, beach.
- Don't use someone else's shoes.
- For nail care services, choose trusted nail salons that sanitize tools after each client.
- To avoid acquiring toenail fungus, you should wash and dry the areas of your lower extremities between your toes every day.
- Socks, knee socks, and tights should be made from natural materials and changed regularly.
- To avoid re-infection, you should disinfect everything that the infected person has interacted with: clothing, bedding, shoes, floors, bathtub, shower, etc.
Introduction
Onychomycosis is often viewed as a natural cosmetic problem, although in reality it is classified as a debilitating disease. It has negative physical and physiological effects on the patient. For example, onychomycosis can lead to complications and disability. The costs associated with treating complications and the number of workdays lost due to illness lead to significant financial losses. Physiological consequences include loss of self-esteem, depression, anxiety and social isolation. Thus, it is very important to treat fungal nail diseases. Preferred treatment outcomes vary depending on the perspective: the patient's goal is to completely restore the nail plate to normal, while the doctor's goal is to destroy the fungus that caused the disease and prevent relapse - a longer-term goal that requires the patient to fully comply with the treatment regimen . Treatment adherence usually increases when comfort with treatment increases and the risk of side effects decreases. Moreover, patients stop treatment as soon as their nails begin to look normal, allowing the fungus to return to full-blown disease. Thus, it is very important that the medicine remains on the nail for some time after stopping treatment.
MANIPOLES
Focus
Capable of treating spots of 7 sizes: from 1 to 7 mm, reaching areas with disturbed pigmentation at various depths, including those with tattoos of any kind. The Focus handpiece can be used in several operating modes: Q:switch, quasi-long-pulse (short-pulse mode), long-pulse mode.
HomoGenius
Treats areas of discolored pigmentation and tattoos using a uniform laser beam with universal energy intensity, preventing excessive heating of the area. A square beam with spot sizes of 3x3 mm2 or 5x5mm2 allows you to treat areas without overlap. The HomoGenius handpiece can be used in Q-switch laser mode.
Pixel manipulator (with depth control)
The pixel arm uses fractional beam splitting to create photoacoustic columns in a 7x7 non-ablative pattern without affecting surrounding tissue. Such microtraumas trigger the regeneration process in the affected areas, collagen synthesis is stimulated, and skin turgor is restored.
Collimated handpiece
The collimated handpiece delivers parallel beams of energy to the tissues of the target area with minimal scattering, regardless of the distance to the skin. This allows you to regulate the course of the procedure without maintaining prolonged contact with the skin, also providing better visualization of larger treated areas. A handpiece with a spot size of 8 mm has a high coverage ratio and high processing speed. The collimated handpiece can be used in all pulse delivery modes.
Y-spectrum and R-spectrum handpieces
Additional Spectrum Handpieces expand ALMA-Q's capabilities by offering two additional wavelengths for color tattoo removal. The Y-spectrum handpiece (585 nm) is especially effective at removing blue light, and the R-spectrum handpiece (650 nm) is especially effective at removing green and blue-green colors.