About the disease
Among the deformations of the skull there are congenital and acquired.
Congenital ones appear during pregnancy, and the child is born with a certain malformation. Acquired ones occur after childbirth, most often as a result of injury or certain intervention, such as surgery. Craniostenosis in children can be either congenital or acquired after birth. This defect is a premature fusion or absence of sutures in the bones of the skull, which normally should remain plastic for the natural growth and development of the child's brain. As a result, intracranial pressure increases and the shape of the skull changes. If we are talking about a developmental defect, craniostenosis in newborns may be accompanied by other defects that affect the brain and other organs of the body. In the case of an acquired disease, suture fusion occurs due to injury or surgery.
Craniostenosis occurs in one in 1000 newborns.
3242
send an SMS with the donation amount to this number
Seams that allow movement
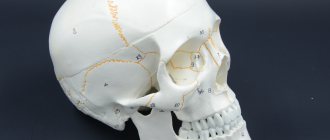
The newborn's skull consists of five main bones: a pair of frontal bones, a pair of parietal bones and one occipital bone. These bones are connected by fibrous sutures that allow the bones to move relative to each other, facilitating birth and brain growth.
Normally, the coronal suture separates the two frontal bones from the parietal bones. The metopic suture separates the frontal bones. The sagittal suture separates the two parietal bones. The lambdoid suture separates the occipital bone from the two parietal bones.
But sometimes something goes wrong... Genetic mutations, which can be local in one area or have a systemic, widespread nature, lead to the sutures closing prematurely.
If the closure of one or another suture is accompanied by other anomalies, such craniostenosis is called “syndromic”. Syndromes characterized by premature closure of cranial sutures: Crouzon Syndrome, Apert Syndrome, Pfeiffer Syndrome, Satpre-Hotzen Syndrome, Carpenter Syndrome and others.
Craniostenosis can be a component of various hereditary syndromes. But in most cases, the hereditary nature of the disease is not confirmed, and craniostenosis does not appear in subsequent generations.
An unusually strong degree of craniostenosis (type scaphocephaly) was present in the so-called “Stettian weaver” (Bonnet, 1904). It was a worker from one of the weaving factories in Stettin. His skull was so long and narrow that the back of his head rested against his back when the unfortunate man tried to raise his head. It was said about the “Stettin weaver” that he never saw the sky and always looked gloomily at the ground. Persecuted for his ugliness by ridicule, he died of pleurisy in the 38th year of his sad life...
Sometimes not one, but several seams are subject to early overgrowth. This also leads to deformation of the skull.
In cases where sutures such as the coronal and sagittal close prematurely, the small dimensions of the upper part of the child’s skull seem to be fixed and their increase stops. Since the growth of bones in the preserved sutures of the skull continues, the so-called “tower” head appears in the adult. The skull becomes elongated upward and slightly backward.
Why is craniostenosis dangerous?
The absence of movable sutures in the skull severely limits the brain. Therefore, the sooner help comes for craniostenosis, the higher the likelihood of a complete cure for the child in the future. Compensation mechanisms in infants under 2 years of age are very high, but rehabilitation after this age turns out to be more complex and lengthy. If not treated promptly, the disease can cause the following conditions:
If you do not receive treatment in a timely manner, the disease can cause the following conditions:
- delayed physical, mental, intellectual development;
- disruption of normal brain functions;
- skeletal underdevelopment;
- compression and atrophy of the optic nerve up to complete loss of vision;
- headache;
- ophthalmological diseases;
- death.
Craniostenosis. Treatment at the Neurology Department of the Schneider Clinic
The Department of Pediatric and Adolescent Neurosurgery , including the head, allows us to eliminate the problem of craniostenosis in its initial stage. To do this, they use gentle surgical techniques. The operations are safe thanks to modern equipment, which allows for complete monitoring of the patient’s brain state during the intervention. Specialists from the departments of neurosurgery and neurology at the Schneider Clinic will help you get rid of the disease at the earliest stages. This will allow the child to grow and develop normally. A slight increase in the volume of the skull by surgeons will give impetus to natural changes in the child’s body and the symptoms will subside on their own.
What is craniostenosis in children?
First of all, it depends on whether the child has other developmental defects. Sometimes pathology accompanies various syndromes - then it is called syndromic. For example, it can occur simultaneously with fusion of fingers or toes, cleft palate or lip, or cerebral hernia.
If fusion of the sutures in the bones of the skull occurs without other developmental defects, it is considered non-syndromic, that is, independent.
Doctors classify the disease into types based on which cranial sutures are fused:
- metopic,
- lambdoid,
- coronary,
- sagittal.
Synostosis - or suture fusion - can involve one to several sutures. There is a concept of pansynostosis - complete overgrowth of all seams. This type of pathology can be considered the most severe; it is less common than others.
Diagnostics
The pathology can be determined during a physical examination, since the clinical picture is quite specific; differentiation with other developmental anomalies is not required.
However, to determine further treatment tactics and the nature of the pathological process, the following diagnostic measures are required:
- radiography;
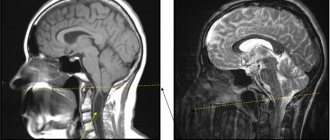
- CT head;
- MRI of the head.
Additionally, standard laboratory tests may be required (general and biochemical blood tests, general urinalysis). After visiting specialized specialists (neurosurgeon, neurologist, pediatrician), an additional consultation with a medical geneticist may be required.
How is craniostenosis treated in children?
There is only one way to eliminate the pathology - surgery. It is performed to restore the shape of the skull bones. After the bones take their natural shape, they are held together with mini-screws or mini-plates and surgical wires, which are removed after a year. They are removed after a year. During the operation, doctors use modern, technologically advanced biodegradable material, which does not need to be removed surgically - it gradually dissolves on its own, and in its place, the patient’s own bone tissue grows. This greatly simplifies the patient's recovery.
The best results can be expected if the surgery is performed between 3–4 months and 2 years of age. Severe deformations of the skull can sometimes be noticed only after the bones have completed their formation, that is, at the age of 5–6 years. In such cases, the pathology manifests itself as severe headaches, blurred vision and increased intraocular pressure, increased fatigue and irritability.
If the disease occurs as a response to craniotomy or after injury, the deformed section of the bone is removed and an implant made of modern material - polymer, metal or ceramic - is installed in its place.
Treatment methods
The main treatment for positional plagiocephaly in infants is the reposition method : repeated changes in body position throughout the day. The child should lie on his back as little as possible when he is awake. Minimize wearing in a sling and carrier, transportation in a car seat. An effective technique is to change the child’s position relative to the light source (stimulates turning over).
Physical therapy is also indicated for children older than 7 weeks It is aimed at:
- stimulation of motor development and correction of positional preferences;
- Stretching the neck muscles for torticollis – increasing the range of motion in the cervical spine.
Involves placing the baby on his stomach while awake under adult supervision.
For moderate and severe deformities, as well as when conservative treatment is ineffective, orthosis – helmet therapy – is indicated. The orthosis is made to individual measurements in an orthopedic workshop. The child wears it 23 hours a day until healing or the need to change the size of the helmet.
Conservative treatment and orthotics lasts several months. The bones of the skull gradually assume a physiological position, while no damage is caused to the brain and neurological diseases do not develop.
If the deformity is due to a congenital anomaly, surgery is indicated. As a rule, it is done at the age of ~7-9 years. The use of orthopedic pillows for newborns is contraindicated, as they sometimes cause infant death.
Sources:
- https://www.ncbi.nlm.nih.gov/pubmed/25382999 Mawji A, Vollman AR, Fung T, Hatfield J, McNeil DA, Sauvé R. Risk factors for positional plagiocephaly and appropriate time frames for prevention messaging // Paediatr Child Health. 2014 Oct;19(8):423-7.
- https://www.ncbi.nlm.nih.gov/pubmed/30151193 Renz-Polster H, De Bock. Deformational plagiocephaly: The case for an evolutionary mismatch // Evol Med Public Health. 2022 Aug 8;2018(1):180-185. doi: 10.1093/emph/eoy019. eCollection 2022.
- E.V. Mamedov. Plagiocephaly. II. Synostosis, deformation and compensatory // Pediatric surgery, 2003, No. 5, pp. 45-50.
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
Symptoms
The severity of symptoms of craniostenosis depends on how many sutures are closed and during what period it occurred. With intrauterine growth, the clinical picture is more pronounced.
The main external manifestation of the pathology is skull deformation, which occurs due to compensatory bone growth perpendicular to the affected suture (Vikhrov’s law). The characteristics of the deformation are determined by which seams closed prematurely. There are three types of pathology:
- scaphocephaly - overgrowth of the sagittal suture, which divides the head in the parietal part into the right and left halves;
- plagiocephaly - closure of the coronal suture, which runs perpendicular to the sagittal one from ear to ear;
- trigonocephaly - closure of the metopic suture dividing the forehead into two equal parts;
- brachycephaly - fusion of the lambdoid and coronal sutures.
Sagittal craniostenosis (scaphocephaly) is the most common type of disease. The width of the skull is reduced, its length in the longitudinal (antero-posterior) direction is increased. The occipital and frontal bones overhang. The temples seem depressed. The child's face has a narrow oval (scaphoid) shape. Neurological symptoms are not typical for scaphocephaly.
Plagiocephaly can be frontal (frontal) or occipital, and unilateral or bilateral. The most common finding is unilateral frontal coronary craniostenosis. In this case, the skull is deformed asymmetrically. On one side, the forehead thickens, the eye socket and eyebrow rise, the auricle protrudes, the nose bends, the cheekbone flattens, the jaw shifts, and so on. Morphological changes occur as the child grows older. Strabismus develops.
Brachycephaly is characterized by an increase in the transverse diameter of the skull and a decrease in its height. Supplemented by ophthalmological and neurological signs.
Trigonocephaly is accompanied by a wedge-shaped protrusion of the forehead forward - a bone keel is formed, running from the large fontanelle to the glabella. The deformity is combined with hypotellorism and visual impairment.
Other possible signs of craniostenosis (usually appear after 12 months):
- hydrocephalus;
- intracranial hypertension;
- headache;
- nausea, vomiting;
- convulsions;
- protruding eyes (exophthalmos);
- delayed intellectual development;
- meningeal symptoms.
Modern neurosurgical techniques
In modern neurosurgery, many surgical techniques are used to correct craniosynostosis, the choice of which is made based on the results of the examination, taking into account the form of craniosynostosis and the required volume of intervention. This:
- linear craniotomy;
- circular craniotomy;
- unilateral and bilateral flap craniotomy;
- fronto-orbital extension;
- reconstructive operations with remodeling of the skull bones and various methods of osteosynthesis;
- total reconstruction of the skull bones;
- endoscopic cranioplasty;
- combined reconstructive techniques, for example, a combination of craniotomy and distraction devices or cranial orthoses (orthopedic devices).
Craniotomy operations involve cutting the skull bones parallel to the fused suture and removing 5-10 mm of bone tissue along the cut. Over time, the bone tissue grows and the integrity of the skull is restored. To prevent new premature fusion of bones, their edges are treated with special compounds.
In the case of polysynostosis, flap surgical techniques and multiple fragmentation of the skull bones are often used. In this case, individual small fragments of bone are removed, creating the opportunity for unhindered growth of the skull and brain. Bone flaps correctly aligned during surgery are fixed with bioabsorbable plates and suture material. By the time the physiological shape of the skull is restored, they are utilized by the body, without requiring a new intervention for removal.
If not only the brain, but also the facial skull is deformed, the frontal bone and orbital region are reconstructed and the position of the upper jaw is corrected. Titanium distraction devices of various designs are especially often used for reconstruction of the facial skull. They are installed during surgery. Spring structures begin to gradually move the bones apart immediately after surgery; other models are adjusted manually, starting from the 7th day after surgery in increments of 1 mm per day. Over the course of six months, the distractors form the correct shape and size of the skull, and then are removed.
Classification
Scaphocephaly is classified according to its clinical picture. There are two types of pathological process:
- a syndrome in which there is a significant protrusion of the skull in the frontal region;
- a syndrome in which the frontal part is normal, but the occipital part is much larger than normal for age.
The impact of both the first and second forms of pathology, if correct treatment is not started in a timely manner, is extremely negative: the consequence may be irreversible mental retardation. Scaphocephaly is one of the most latent forms of craniostenosis, since cognitive impairment occurs only in the absence of therapy.
Diagnostics
Parents of a newborn should pay attention to:
- on the unusual shape of the baby’s head;
- early closure (up to 1 year) of the fontanelle;
- psychomotor developmental delay;
- child's anxiety when weather conditions change.
If these symptoms appear, parents should immediately contact the following specialists:
| BELOW ARE THE BEST SPECIALISTS IN YOUR REGION |
- Neurologist. Assess the delay in the rate of mental development of the child and the presence of neurological symptoms.
- Ophthalmologist. Determines the presence of intracranial hypertension (pressure) and assesses visual acuity.
- Pediatrician. Will assess the state of somatic (physical) pathologies.
- Geneticist. It will reveal the hereditary nature of the disease and developmental anomalies of other organs. Will give a prognosis for the recurrence of the disease in the next child.
Instrumental diagnostic methods include:
- Ultrasound of internal organs. Other developmental anomalies are being identified.
- Ultrasound (venography) of the main vessels of the neck and head reveals a violation of the venous outflow of blood from the skull and the presence of intracranial hypertension.
- Echocardiography. Detects heart defects.
- Craniometry (cephalometry). Anthropological parameters of the skull are measured.
- An ECG reveals disturbances in the frequency and rhythm of heart contractions.
- Computed tomography of the skull.
- MRI of the brain.
Differential diagnosis
Craniostenosis must be differentiated (distinguished) from diseases:
- cephalohematoma;
- Down's disease;
- microcephaly;
- deformations of the skull after suffering from rickets.