1.Burkitt's lymphoma and its types
Burkitt's lymphoma is a form of non-Hodgkin's lymphoma.
in which cancer begins in immune cells.
Burkitt's lymphoma is recognized as the fastest growing tumor in humans
, and if treatment is not started in time, it quickly leads to death. But intensive chemotherapy helps to significantly prolong the life of patients with Burkitt's lymphoma in more than half of the cases.
Burkitt's lymphoma is named after British surgeon Denis Burkitt, who first diagnosed the disease in 1956 among African children. In Africa, lymphoma affects children who also have malaria and the Epstein-Barr virus, which causes infectious mononucleosis. It is likely that malaria weakens the immune system's response to the Epstein-Barr virus, allowing it to attack infected cells and turn them cancerous.
Outside of Africa, Burkitt's lymphoma is rare. People infected with HIV, the human immunodeficiency virus, are more prone to developing this disease. According to statistics, the incidence of Burkitt's lymphoma in HIV-positive people is 1000 times higher than in those who are not infected.
Types of Burkitt's lymphoma
The World Health Organization classification identifies three types of Burkitt lymphoma:
- Endemic
(African lymphoma), which we described above; - Sporadic Burkitt's lymphoma
. This form of lymphoma occurs throughout the world. According to statistics, sporadic Burkitt lymphoma accounts for 1 to 2% of all cases of lymphoma in the adult population. - Lymphoma associated with immunodeficiency.
This type of Burkitt's lymphoma most often occurs in people with HIV/AIDS. But it can also develop in people with congenital conditions that cause immunodeficiency, as well as in patients who have had organ transplants and take immunosuppressive drugs (suppress the immune system).
A must read! Help with treatment and hospitalization!
Discussion
By 2009, 101 cases of a combination of NHL and pregnancy were described in the literature [3]. By 2013, 74 papers describing 121 clinical observations were presented in the foreign literature [15]. At the same time, in recent decades there has been an increase in the incidence of NHL, which makes this problem urgent [16–18]. The most common type of NHL diagnosed during pregnancy is primary mediastinal B-cell lymphoma [16].
Basic data on pregnancy-associated NHL are limited to individual case reports, which makes it difficult to develop tactics for the treatment of lymphoma and management of pregnancy against the background of hematological malignancy [15]. The combination of LB and pregnancy is even less common; isolated similar cases have been described in the world, some of them are presented in Table 1.
Collaborative prospective studies are needed to further characterize the pathophysiological and clinical aspects of this disease, which complicates pregnancy [15].
Pregnancy management in the Russian Federation is currently carried out in accordance with Order No. 736 of the Ministry of Health and Social Development of Russia dated December 3, 2007 “On approval of the list of medical indications for artificial termination of pregnancy.” Termination of pregnancy before 12 weeks. indicated for patients in the following cases: lymphomas from high-risk groups (follicular NHL, diffuse NHL, peripheral and cutaneous T-cell lymphomas, other and unspecified types of NHL, malignant immunoproliferative diseases, multiple myeloma), lymphogranulomatosis stages III–IV. In the second and third trimesters, the issue of termination of pregnancy is decided in each individual case by a council with the participation of a hematologist, oncologist, obstetrician-gynecologist, neonatologist, therapist and, of course, the mother of the unborn child and her relatives.
The standard treatment for LB are protocols that include high doses of methotrexate and cytarabine: R-Hyper-CVAD, R-CODOX–M/IVAC, NHL-BFM. However, due to their ability to penetrate the blood-placental barrier, they cannot be used during pregnancy. The R-DA-EPOCH program is included in the Russian national clinical guidelines as a protocol for patients who, due to the severity of their condition, cannot undergo more intensive chemotherapy. In our case, the choice of this chemotherapy program allowed us to achieve remission and provided the opportunity to prolong pregnancy.
2.Symptoms of Burkitt's lymphoma
Symptoms of Burkitt's lymphoma depend on its type. Endemic (African) lymphoma usually begins with a tumor
jaw or other facial bones. It can also affect the gastrointestinal tract, breasts and ovaries, and spread to the central nervous system, causing nerve damage, weakness and paralysis.
Sporadic and immunodeficiency Burkitt lymphomas usually begin in the intestines and form large tumors in the abdomen. Later, the liver, spleen and bone marrow are often affected. The growth of cancer cells in Burkitt lymphoma can also begin in the ovaries, testicles or other organs, spreading to the brain and cerebrospinal fluid.
In addition to tumor growth, symptoms of Burkitt's lymphoma may include:
:
- Loss of appetite;
- Weight loss;
- Fatigue;
- Sweating at night;
- Unexplained fever.
Visit our Oncology page
Key signs of the disease
Externally Burkitt's lymphoma
represents single or multiple neoplasms that appear on the kidneys, ovary, peritoneal cavity, pancreas, intestines, and other vital organs.
The tumor quickly increases in size, affecting soft tissues or destroying bones, as a result of which the patient may experience difficulty breathing, dizziness, and increased body temperature. Further development of Burkitt's lymphoma
leads to compression of the spinal cord roots, permanent bone fractures or paralysis. Other important signs of this disease include:
- deformation of the nasal septum;
- swallowing dysfunction;
- intestinal obstruction or abdominal pain;
- the presence of neoplasms in the jaw area, etc.
Depending on the form of development of the disease, the symptoms of Burkitt's lymphoma
may be accompanied by a number of other painful sensations, if they occur, you should immediately consult a doctor.
3. Diagnosis of Burkitt's lymphoma
Because Burkitt lymphoma spreads so quickly, early diagnosis is critical to a patient's recovery.
If Burkitt's lymphoma is suspected, a biopsy
enlarged lymph nodes or other suspected foci of disease. Taking a tissue sample and further examining it under a microscope will help confirm or rule out the diagnosis of Burkitt's lymphoma.
Additional methods for diagnosing lymphoma may be:
- Computed tomography of the chest, abdomen and pelvis;
- Chest X-ray;
- PET, or positron emission tomography;
- Bone marrow biopsy;
- Cerebrospinal fluid examination;
- Blood tests to evaluate kidney and liver function;
- Testing for HIV infection.
About our clinic Chistye Prudy metro station Medintercom page!
Clinical observation
Patient P., 39 years old. I went to the antenatal clinic in the Republic of Crimea due to the onset of spontaneous pregnancy.
Pregnancy 3rd. The birth is due on the 1st.
History: 1st pregnancy (2005) - spontaneous miscarriage at 12 weeks of gestation, abrasio cavi uteri
(no complications);
2nd pregnancy (2011) - spontaneous miscarriage at 9 weeks of gestation, abrasio cavi uteri
(without complications).
History of the disease: on the 6th week. During this pregnancy, a cyst of the right ovary was detected. She was under the supervision of an obstetrician-gynecologist at a antenatal clinic in the Republic of Crimea. From October for 3 months. lost 20 kg. She did not actively complain.
On December 1, 2016, magnetic resonance imaging (MRI) of the pelvic organs was performed. Conclusion: pregnancy 20 weeks. MR signs of a space-occupying lesion in the right ovary (the right ovary is not visualized in its typical location). Above the uterus on the right, a formation measuring 46×31×30 mm is detected, the nature of the signal is similar to the ovary. Next to it, a formation measuring 174 × 152 × 128 mm with clear, sometimes bumpy contours is determined, probably emanating from it, intimately adjacent and moderately compressing the upper wall of the uterus. In the groin areas, enlarged lymph nodes are visualized: on the right up to 18 mm, on the left up to 14 mm. Free fluid is detected in the retrouterine space and in the abdominal cavity, more on the right.
Taking into account the MRI data, for the purpose of further examination and deciding on further management tactics, the patient was sent to Moscow and on December 9, 2016 was hospitalized in one of the hospitals in Moscow. According to the results of an MRI of the pelvic organs dated December 9, 2016: MRI picture of a space-occupying formation, apparently coming from the right ovary. Ascites.
On December 20, 2016, laparotomy, right adnexectomy, multiple peritoneal biopsy, and subtotal omentectomy were performed.
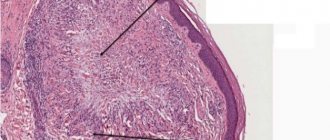
Results of a histological examination of the removed tumor dated December 20, 2016: the tumor is represented by a diffuse infiltrate of monomorphic cells with eosinophilic cytoplasm, a large nucleus with 2-3 nucleoli, high mitotic activity and macrophages diffusely located in the tumor (a “starry sky” picture). Conclusion: diffuse large cell lymphoma of the ovary, probably LB.
Immunohistochemical study of an ovarian tumor dated December 20, 2016: CD45, CD79a - pronounced cytoplasmic expression in 100% of tumor cells; Vimentin is highly expressed in the tumor stroma. Inhibin alpha, S100, Keratin Pan - no expression.
FISH study of an ovarian tumor from December 20, 2016: translocation t (8;14) (q24; q32), rearrangements of BCL2
and
BCL6
was not detected.
For further examination, treatment and determination of further management tactics, on December 30, 2016, the patient was transferred to the City Clinical Hospital No. 52 of the Department of Health. At the time of admission, there were symptoms of intoxication, a 20 kg weight loss due to pregnancy, and night sweats.
MRI of the abdomen and pelvis dated December 30, 2016: in three mutually perpendicular planes in T1, T2 and fat suppression modes, in diffusion-weighted image mode, without intravenous contrast: the liver is enlarged in size - 123 mm (sagittal anteroposterior size at the level of the right lobe ) × 82 mm (antero-posterior size of the left lobe) × 230 mm (frontal size) × 160 mm (vertical size of the right lobe), has smooth and clear contours, the signal characteristics of the parenchyma are not changed. The intrahepatic bile ducts are not dilated. No focal changes in the parenchyma were detected during the native study. The gallbladder is 70x32 mm in size, with heterogeneous liquid contents (due to sedimentation of bile). The common bile duct is dilated to 5.5 mm, stones in the gallbladder and ducts are not reliably visualized. At the site of surgical manipulations on the left there are cicatricial changes with slight swelling of the subcutaneous fatty tissue. There is soft tissue compaction along the anterior abdominal wall, postoperative changes. The pancreas is not enlarged - 22×19×22 mm, the structure is heterogeneous due to small fatty inclusions, the contours of the gland are clear, small-lumpy. Additional formations in the projection of the pancreas are not identified. The Wirsung duct is not dilated, its diameter is up to 2.5 mm, visualized along its entire length, and not deformed. Parapancreatic tissue without reliable signs of inflammation and infiltration. The dimensions of the spleen are 116 × 46 × 98 mm (sagittal × frontal × vertical), its contours are clear and even. The structure is homogeneous. The right and left adrenal glands are without any features. The kidneys are typically located, have dimensions: right - 108x58x56 mm, left - 119x53x58 mm, the parenchyma is not thinned, no focal changes in the parenchyma were detected. The pyelocaliceal system is not dilated or deformed. Lymph nodes are not enlarged, the number of mesenteric lymph nodes is not increased. No free fluid was detected in the abdominal cavity and retroperitoneal space. In the pelvic projection, an increased amount of free fluid is not detected. The rectum was without visible changes, no thickening of the walls or neoplasms were detected. The bladder is moderately full, the walls of the bladder are not completely straightened, without areas of altered signal, including on diffusion-weighted images. The contents are liquid, no stones were detected. Paravesical tissue without features.
Pregnancy 24–25 weeks. One fetus is visualized in the uterine cavity. The amount of water is moderate. The placenta is along the anterior wall in the fundus area. Adjacent to the uterus to the right with a wide radius (in the projection of the right ovary) is a solid formation with clear coarse-lumpy contours of an inhomogeneous structure, predominantly hypointense in T2, T1 and fat suppression modes, with a high signal on an isotropic series of diffusion-weighted images - with dimensions 46×21×48 mm (anteroposterior × bilateral × vertical). The left ovary measures 38×21×30 mm, contains a few follicles up to 7.5×3.0 mm in size, the rest of the structure is without features, no areas of diffusion restriction were identified in the diffusion-weighted image mode. The contours of the ovary are clear, even, the accumulation of fluid around is not detectable. The lymph nodes are not enlarged: the size of the iliac nodes is up to 4–5 mm, the inguinal nodes on the right are up to 11×5 mm, the inguinal nodes on the left are 8×12 mm. Their differentiation is not impaired. No bone destructive changes were detected. Conclusion: MR picture of a space-occupying lesion on the right (in the projection of the right ovary). Pregnancy 24–25 weeks. A picture of mild hepatosplenomegaly, congestive gallbladder, diffuse changes in the pancreas (Fig. 1).
Myelogram dated December 31, 2016: blasts 0.8%, lymphocytes 6%. In the cerebrospinal fluid as of December 31, 2016, cytosis was 2/3.
According to ultrasound and Doppler examination of the fetus dated 01/09/2016: pregnancy 26–27 weeks. Breech presentation. Blood flow indicators are normal.
Based on complaints, medical history, results of laboratory and instrumental studies, a diagnosis was made.
Main disease.
Burkitt's lymphoma, stage III according to SB Murphy with damage to the right ovary (bulky), ascites. Condition after laparotomy, right-sided adnexectomy, multiple peritoneal biopsy, subtotal omentectomy (12/20/2016). Continued tumor growth. Pregnancy 27 weeks.
For cytoreductive purposes, a prephase was carried out from December 31, 2016 to January 4, 2017 (cyclophosphamide 400 mg, dexamethasone 20 mg).
On January 5, 2017, chemotherapy was started under the R-DA-EPOCH program (rituximab - etoposide - prednisolone - vincristine - cyclophosphamide - doxorubicin) with intrathecal administration of cytostatics (prevention of neuroleukemia). After two courses, the tumor was not detected by MRI. Remission of the disease was stated. The 3rd course of the R-DA-EPOCH program was conducted.
Each intercourse period, the patient was observed in the pregnancy pathology department of the maternity hospital of City Clinical Hospital No. 52. At a gestational age of 29–30 weeks. the course of pregnancy was complicated by the development of gestational arterial hypertension. The pregnant woman had an increase in blood pressure to 140/90–150/90 mmHg. Art., tests showed moderate proteinuria. Against the background of antihypertensive therapy, hemodynamic stabilization was achieved, proteinuria remained at the same level (daily protein loss less than 0.3 g/l, in a general urine test proteinuria did not exceed 0.3 g/l).
On February 27, 2017, during the next hospitalization in the intercourse period, Doppler measurements revealed disturbances of the uteroplacental blood flow of the 3rd degree with zero diastolic blood flow. Considering the decompensation of placental insufficiency and critical blood flow disorders in a primigravida at the age of 39 years with a burdened obstetric-gynecological and somatic history, it was decided to deliver the pregnant woman by cesarean section as an emergency in the interests of the fetus.
On February 27, 2017, a lower median laparotomy was performed, a cesarean section in the lower uterine segment with a transverse incision under spinal epidural anesthesia. A live premature girl with a body weight of 1930 g, length 46 cm, with an Apgar score of 6/6 points was extracted. The operation was performed without any technical difficulties. The early postoperative period proceeded without complications.
From March 2, 2017, the course of the late postpartum period was complicated by the development of myelotoxic agranulocytosis after a course of chemotherapy. On 03/05/2017, a temperature swing of up to 38.1 °C was observed without visible foci of infection. Due to the development of a complication, the postpartum woman was transferred to the hematology department.
Data from multislice computed tomography of the neck, thoracic and abdominal organs, and pelvis dated 03/09/2017: axillary and mediastinal lymph nodes are not enlarged, there is no fluid in the pleural cavities. Pulmonary parenchyma without focal changes. Mesenteric and retroperitoneal lymph nodes are not enlarged. A single lymph node measuring 23×8 mm was noted in the left groin area. The spleen is of normal shape and size (vertical size 81 mm), with clear, even contours; the structure and density of the parenchyma are not changed in the native study. The liver is not enlarged, the density of the parenchyma is 47 HU, and no foci of pathological density were detected during the native study. No volumetric formations were found in the parenchymal organs or interintestinal spaces. Conclusion: No CT evidence of lymphadenopathy was obtained. No focal pathological changes in the chest organs, abdominal cavity, retroperitoneal space, or pelvic cavity were identified. Thus, remission of LB was maintained.
In order to relieve neutropenic fever, antibacterial therapy with piperacillin, tazobactam and amikacin was administered intravenously; during therapy, restoration of blood counts and normalization of body temperature were noted.
From March 16, 2017 to May 17, 2017, 3 more courses of polychemotherapy were conducted under the R-DA-EPOCH program. According to the results of positron emission tomography combined with computed tomography (PET-CT), after 6 courses of polychemotherapy, the patient achieved a complete metabolic response.
Subsequently, the patient with a healthy newborn, who was safely discharged from the second stage of nursing, went to her place of permanent residence.
Over the next two years, the patient was under the supervision of hematologists of the State Budgetary Healthcare Institution “City Clinical Hospital No. 52 DZM”: every six months a CT study with contrast was carried out, and the clinical status was assessed. The last follow-up examination (PET-CT) was carried out on March 12, 2019: the patient remains in remission of LB. Taking into account the absence of late relapses of the disease in LB (all events occur within the first year after completion of treatment), we can talk about the patient’s recovery [14].
4. Treatment of Burkitt's lymphoma
Intensive intravenous chemotherapy
, which is usually performed in a hospital, is the most effective treatment for Burkitt lymphoma.
Because Burkitt's lymphoma can spread to the fluids surrounding the brain and spinal cord, chemotherapy drugs may be injected directly into the cerebrospinal fluid. This treatment method is called intrathecal chemotherapy.
drugs may be used to treat Burkitt's lymphoma
. For example, cyclophosphamide, cytarabine, doxorubicin, etoposide, methotrexate, vincristine and others.
Intensive chemotherapy can be either an independent treatment method for Burkitt lymphoma or an integral part of complex treatment. Along with chemotherapy, the following are used:
- Rituximab
is a monoclonal antibody that sticks to proteins in cancer cells and stimulates the immune system to attack the cancer cells; - Autologous stem cell transplantation
. These are stem cells that have previously been taken from the patient and stored in a stem cell bank; - Radiation therapy;
- Steroid therapy.
Burkitt's lymphoma is a fatal disease if left untreated. In children, prompt, intensive chemotherapy usually cures lymphoma and predicts long-term survival in 60-90% of cases. In adult patients, the results are very different, but on average, timely treatment means long-term survival in 70-80% of cases, which is also significant.