There are many causes for hypocalcemia and hyperphosphatemia. But secondary hyperparathyroidism, which develops in patients receiving renal replacement therapy, deserves special attention. A progressive decrease in the number of functioning nephrons in chronic renal failure causes disruption of all links in the regulation of phosphorus-calcium metabolism.
When hyperphosphatemia occurs, there is a response decrease in ionized calcium. Hyperphosphatemia and hypocalcemia directly stimulate the synthesis of parathyroid hormone (PTH) by the parathyroid glands. Calcium affects the processes of PTH synthesis through calcium receptors present in the parathyroid glands, the number and sensitivity of which decrease. As the decline in renal function progresses, a deficiency of calcitriol, the active metabolite of vitamin D3 synthesized in the kidneys, also occurs, and the number of calcitriol receptors in the parathyroid glands decreases. As a result of these processes, the inhibitory effect of calcitriol on the synthesis and secretion of PTH is weakened, and skeletal resistance to the calcemic effect occurs, which is also accompanied by hypersecretion of PTH.
Symptoms of hyperparathyroidism
Initially, with the development of hyperparathyroidism, patients feel nothing but general weakness. However, as the disease progresses, symptoms such as:
- pain in bones and joints;
- muscle weakness;
- fatigue;
- decreased tone;
- fractures;
- manifestations of urolithiasis, due to excessive load on the kidneys due to the need for increased excretion of calcium from the body;
- gastrointestinal disorders due to mineral disturbances and changes in appetite;
- increased atherosclerotic changes due to calcium deposits in the walls of blood vessels;
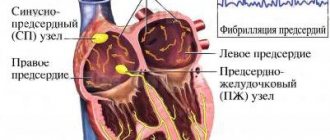
- cardiac dysfunction;
- manifestations of peptic ulcer disease due to impaired blood supply to the walls of the mucous membrane of various parts of the gastrointestinal tract and the formation of peptic ulcers;
- psychoneurological disorders due to metabolic disorders of nerve fibers.
Read also
Osteoporosis
Osteoporosis is a progressive metabolic disease of the skeletal bones, which results in a decrease in bone density and disruption of its internal structure.
The result of osteoporosis is... Read more
Itsenko–Cushing syndrome
Itsenko-Cushing syndrome is a disease that occurs against the background of chronic hypercortisolism, i.e., an increased level of the hormone cortisol in the blood secreted by the adrenal cortex, or long-term treatment...
More details
Diabetes mellitus, type 2
Diabetes mellitus (DM) is a group of metabolic diseases characterized by chronic hyperglycemia, which results from impaired insulin secretion, insulin action, or both...
More details
Symptomatic arterial hypertension
Arterial hypertension is a very common disease of the human cardiovascular system. According to statistics, 20-30% of the population suffers from arterial hypertension, aged 60 years and above...
More details
Complications of diabetes
Diabetes mellitus (DM) is a systemic disease caused by absolute (type 1) insulin deficiency or insulin resistance (type 2), which causes impaired carbohydrate metabolism, manifested by chronic...
More details
Classification
Primary hyperparathyroidism
Occurs in patients with a tumor of the parathyroid glands (adenoma), which microscopically represents a genetically similar focal growth of tissue; usually only one parathyroid gland is affected.
Secondary hyperparathyroidism
develops as a response to a long-term decrease in the level of Ca2+ in the blood due to vitamin D deficiency, manifestations of chronic renal failure or severe absorption disorders in the gastrointestinal tract, as well as due to hemodialysis in patients. Microscopic changes. At this stage, regression of the disease is still possible with adequate correction of the causes that caused it, reverse development of morphological changes in the parathyroid glands and stabilization of the patient’s PTH level.
Tertiary hyperparathyroidism
occurs with long-term secondary hyperparathyroidism, with the formation of adenomas, amenable only to surgical correction.
The approach to the treatment of different forms of hyperparathyroidism, indications for surgery, as well as the scope of required surgical intervention differ significantly. Specialists at the Endocrine Surgery Clinic can determine your individual treatment plan after conducting the necessary diagnostic tests.
Publications in the media
Regarding the treatment of this disease, you can contact the Surgical Department No. 2 of the Clinic of Faculty Surgery named after. N.N. Burdenko
Hyperparathyroidism is a disease of the endocrine system caused by excessive secretion of PTH and characterized by severe disturbances in the metabolism of calcium and phosphorus. There are primary, secondary and tertiary hyperparathyroidism • Primary. Hyperfunction of the parathyroid glands due to their hyperplasia or neoplasm. Two thirds of cases of primary hyperparathyroidism occur in postmenopausal women • Secondary develops compensatoryly and is usually found in chronic renal failure in conditions of vitamin D deficiency and prolonged hyperphosphatemia or malabsorption syndrome in conditions of chronic hypocalcemia • Tertiary is caused by a developing adenoma of the parathyroid glands against the background of long-standing secondary hyperparathyroidism • Pseudohyperparathyroidism ( ectopic hyperparathyroidism) is observed in malignant tumors of various locations (bronchogenic cancer, breast cancer, etc.); associated with the ability of some malignant tumors to secrete PTH.
Statistical data. 1 case per 1000 population (primary hyperparathyroidism). Predominant age: 20–50 years. The predominant sex is female (2.5:1).
Genetic aspects • Familial primary hyperparathyroidism with multiple ossifying fibromas of the jaw (*145001, Â) • Familial primary hyperparathyroidism (*145000, Â) due to hyperplasia of the chief cells of the parathyroid glands • Congenital primary hyperparathyroidism with hypercalciuria (239199, r). Clinically: nephrocalcinosis, renal tubular acidosis, developmental delay, nausea. Laboratory: elevated PTH levels, hypercalcemia, hypercalciuria • Congenital familial hyperparathyroidism (#239200, r or Â) - the disease is caused by homozygosity for the mutant parathyroid calcium receptor gene, which in the heterozygous state causes familial hypocalciuric hypercalcemia (145980). Clinically: congenital primary hyperparathyroidism, developmental delay, decreased appetite, constipation, thirst, hepatomegaly, splenomegaly, polyuria, renal calcinosis, arterial hypotension, multiple fractures, metaphyseal abnormalities, osteoporosis, narrow chest, shortness of breath, anemia. Laboratory: hypercalcemia, hypophosphatemia, hypercalciuria, hyperphosphaturia, aminoaciduria, increased levels of parathyroid hormone in the blood serum, hyperplasia of parathyroid cells.
Risk factors • Age over 50 years • Female gender • Ionizing radiation.
Etiology and pathogenesis • Primary hyperparathyroidism •• Single parathyroid adenoma - 80–90% of cases; hyperplasia of all four glands causes 10–20% of cases of primary hyperparathyroidism. Parathyroid cancer is rare •• PTH increases blood calcium levels by stimulating the formation of vitamin D and its conversion to calcitriol (important for calcium absorption in the gastrointestinal tract), increasing renal tubular calcium reabsorption, decreasing renal tubular phosphate reabsorption, and mobilizing calcium from bones •• Elevated levels of circulating calcium ions inhibit PTH synthesis. It is believed that the parathyroid adenoma is capable of functioning autonomously, producing, despite a high level of serum calcium, an excessive amount of PTH and leading to primary hyperparathyroidism • Secondary hyperparathyroidism •• Most often observed in chronic renal failure with the development of adaptive hyperplasia and hyperfunction of the parathyroid glands due to prolonged hypocalcemia. Other causes: rickets, Fanconi syndrome, malabsorption syndrome •• Impaired production of calcitriol in the kidneys due to vitamin D deficiency leads to impaired absorption of calcium in the gastrointestinal tract and hypocalcemia •• Damage to the renal parenchyma leads to hyperphosphatemia •• Resistance of bone and renal tissue to PTH.
The clinical picture depends on the concentration of calcium in the blood serum. The disease usually manifests as mild asymptomatic hypercalcemia, although patients with classic signs of advanced kidney and bone damage are sometimes observed. When calcium levels exceed 11–12 mg%, neurological and gastrointestinal symptoms appear. At a content of 14–20 mg%, a hyperparathyroid hypercalcemic crisis develops, manifested by uncontrollable vomiting, thirst, muscle and joint pain, symptoms of an acute abdomen, an increase in body temperature to 40 ° C and impaired consciousness. Mortality is 50–60%. Manifestations of hyperparathyroidism itself: • Renal •• Hypercalciuria and urinary tract stones •• Chronic hypercalcemia leads to the deposition of calcium salts in the renal parenchyma (nephrocalcinosis), renal failure occurs •• Polyuria and thirst due to hypercalciuria with damage to the epithelium of the renal tubules and a decrease in the sensitivity of renal tubular receptors to ADH • Skeletal. Excess PTH increases bone resorption by osteoclasts and leads to a disorder of bone metabolism (parathyroid osteodystrophy, or von Recklinghausen's disease) • Gastrointestinal •• Anorexia •• Weight loss •• Constipation •• Nausea •• Vomiting •• Abdominal pain •• Ulcers are common illness and pancreatitis • Neurological and mental •• Emotional lability •• Intellectual impairment •• Fatigue •• Muscle weakness • Cardiovascular •• Arterial hypertension •• Shortening of the Q-T interval • Articular and periarticular •• Arthralgia •• Gout •• Pseudogout • Ophthalmic •• Keratopathy •• Conjunctivitis due to calcium deposition in the conjunctiva • Skin - itching.
Concomitant pathology. Familial polyendocrine adenomatosis.
Age characteristics. Older people are more likely to have secondary hyperparathyroidism.
Differential diagnosis • Tumors (see Hypercalcemia in Malignant Tumors) • Sarcoidosis causes hypercalcemia due to the production of calcitriol by granulomatous tissue. In the absence of elevated PTH levels and signs of sarcoidosis, ex juvantibus therapy is recommended. In most cases of sarcoidosis, a decrease in serum calcium levels is observed within 1 week after administration of GC (for example, 40 mg prednisolone daily), but this is not observed in primary hyperparathyroidism • Familial hypocalciuric hypercalcemia (*145980, 3q21–q24, mutation of the HHC1, FHH, Â). Mild to moderate hypercalcemia, complications (urinary stones and renal failure) are rare •• PTH levels are normal or slightly elevated, parathyroid hyperplasia is possible, but subtotal parathyroidectomy does not reduce hypercalcemia •• The key to diagnosis is the familial nature of the disease and low urinary calcium excretion •• Due to the ineffectiveness of surgical intervention, this condition should be excluded in patients with primary hyperparathyroidism • Hypervitaminosis D • Milk-alkali syndrome is caused by the consumption of large quantities of calcium and absorbable alkalis; characterized by hypercalcemia, systemic alkalosis and kidney damage due to nephrocalcinosis. The risk of this syndrome increases with daily intake of more than 5 g of calcium carbonate (or 2 g in terms of calcium), which is 2 times the dose recommended for the prevention or treatment of osteoporosis • Other causes of hypercalcemia •• Hyperthyroidism causes hypercalcemia due to increased bone turnover •• Thiazide diuretics reduce urinary calcium excretion but rarely cause hypercalcemia; they are not prescribed to patients with hyperparathyroidism •• Prolonged immobilization can lead to hypercalcemia due to bone resorption. The problem especially often occurs in children who are bedridden for a long time (for example, in the case of a corset in the treatment of multiple fractures) •• Osteitis deformans •• Recovery from acute renal failure caused by necrosis of skeletal muscles is often accompanied by hypercalcemia. During the first 2–3 days after muscle injury, local deposition of calcium and phosphate occurs due to the destruction of myocytes. When kidney function normalizes, calcium and phosphates leave the areas of muscle damage and enter the bloodstream, causing hypercalcemia. This disorder usually occurs 2–3 weeks after acute muscle injury.
Laboratory Findings • Hypercalcemia is the cardinal sign of primary hyperparathyroidism • Hypophosphatemia • Serum chloride to phosphate ratio is usually elevated (>33), which is explained by increased serum Cl– (due to PTH-induced bicarbonaturia) • Serum ALP activity is increased only in patients with significant bone loss pathology • Hypercalciuria, but due to the Ca2+-reabsorbing action of PTH, in approximately one third of patients the calcium content in the urine is normal • An increase in the level of PTH in the blood in the presence of hypercalcemia is a strong argument in favor of primary hyperparathyroidism, because for other reasons for increased calcium, a decrease in PTH is observed. However, in some cases, a negative test result does not definitively exclude the possibility of primary hyperparathyroidism.
The influence of drugs. Lithium preparations, thiazide diuretics or ergocalciferol may increase serum calcium levels.
Special studies • Ultrasound, CT, MRI and isotope scanning are non-invasive methods that detect parathyroid adenomas in 60-80% of cases • Selective venous catheterization - collect blood samples from veins draining various areas of the neck and mediastinum. A significant increase in PTH concentration makes it possible to determine the location of the adenoma. The procedure is performed on patients before re-operation after an unsuccessful revision of the neck area.
TREATMENT
Lead tactics. In patients over 50 years of age without clinical symptoms and with serum calcium levels no higher than 11.4–12 mg%, the disease often does not progress for 10 years or more. Patients are under observation; surgical treatment is recommended if calcium levels increase, the patient develops kidney damage, skeletal damage, or other manifestations characteristic of a severe course of the disease.
Surgical treatment is the only radical and effective method.
• Preoperative preparation •• Ergocalciferol 2-3 days before surgery •• In case of dehydration - intensive rehydration •• Sanitation of the urinary tract • Anesthesia - general anesthesia • Intraoperative tactics •• In most cases, a single adenoma is found to be removed •• Three glands are removed and part four •• Remove all tissue of the parathyroid glands with transplantation of part of the tissue into the muscles of the forearm •• In approximately 10% of cases, during initial revisions of the neck area, it is not possible to identify altered tissue of the parathyroid gland
• The postoperative period •• Usually proceeds relatively easily •• Patients recover within a few weeks.
• Postoperative complications •• Damage to the recurrent nerve •• Tetany •• AKI •• Acute pancreatitis •• Transient hypocalcemia •• “Hungry bone” syndrome.
Conservative treatment is indicated if there are contraindications to surgical treatment, the patient refuses surgery or is unsuccessful • Increased fluid intake and physical activity help reduce serum calcium levels • Phosphates in doses of 1–2 g per day orally. The main complication is extraosseous calcification (very rare) • Estrogens (postmenopausal replacement therapy) reduce mildly elevated serum calcium levels by decreasing bone resorption.
Emergency treatment of hyperparathyroid hypercalcemic crisis.
• Forced diuresis (up to 4 liters of 0.9% sodium chloride solution intravenously in combination with the administration of furosemide intravenously).
• Bisphosphonates (pamidronic and etidronic acids) cause a decrease in serum calcium levels within 1–7 days •• Pamidronic acid 60–90 mg IV once a day; if necessary, the administration is repeated after 7 days •• Etidronic acid 7.5 mg/kg IV over 4 hours 1 time per day for 3–7 days.
• Gallium nitrate 200 mg/m2/day as a long-term infusion for 5 days. Use is limited by potential nephrotoxicity.
• Calcitonin 4 IU/kg IM or SC every 12 hours (acts faster, more briefly, weaker than plicamycin, gallium nitrate and pamidronic acid, but less toxic).
• GCs do not affect serum calcium levels in patients with hyperparathyroidism.
Course and prognosis • The prognosis is extremely favorable for primary hyperparathyroidism after surgical treatment • The prognosis is not very favorable for secondary and tertiary hyperparathyroidism (determined by the functional state of the kidneys).
ICD-10 • E21 Hyperparathyroidism and other disorders of the parathyroid [parathyroid] gland
Diagnostics
Even before clinical manifestations, patients suffering from hyperparathyroidism experience an increase in calcium levels in a biochemical blood test, an increase in urine calcium levels, and an increase in blood PTH levels. Often, especially in postmenopausal women, insufficient levels of vitamin D in the blood are detected.
Densitometry (examination of bone tissue) reveals severe osteoporosis due to increased bone tissue breakdown under the influence of PTH.
To visually identify and determine the location of altered parathyroid glands, the following is performed:
- Ultrasound of the neck area
- Scintigraphy of the parathyroid glands, which allows you to determine the hyperfunction of the parathyroid glands and establish the form of the disease (primary or secondary).
Currently, puncture biopsy of the parathyroid glands is not performed, which is associated with the usually high density of the formation, often its small size (up to 1 cm) and the high risk of tumor disintegration and spread of parathyroid cells along the puncture channel, which contributes to the progression of the disease and complicates further surgical treatment .
The wide range of manifestations and variability of the course of the disease require comprehensive examination and treatment of patients by highly qualified specialists.
However, with already pronounced changes in calcium-calcium-phosphorus metabolism, even with minimal symptoms, the only option for productive treatment is surgical intervention.
Treatment of hyperthyroidism:
The main treatment for hyperparathyroidism is surgery. The parathyroid adenoma or hyperplastic thyroid gland is removed.
If the patient has been diagnosed with a hypercalcemic crisis, then conservative treatment is carried out aimed at reducing calcium in the blood: forced diuresis (intravenous infusion + plenty of fluids).
Glucocorticoids; if the calcium level is more than 3.5 mmol/l, emergency extracorporeal detoxification (hemodialysis session) is indicated.
Forecast
In the absence of treatment and severe course of the disease, disability occurs. Life-threatening is hypercalcemic crisis , the mortality rate of which reaches 60%. Detection of the disease at an early stage and timely surgical treatment prevent the occurrence of osteovisceral complications.
After surgery, the symptoms of the disease disappear, recovery occurs in 90% of cases. During the first year after surgery, bone mineral density increases by 15-25%.
I. Introduction
Clinical guidelines for the provision of medical care to patients with primary hyperparathyroidism (PHPT) are compiled in accordance with the requirements for the development of clinical guidelines by medical professional non-profit organizations in accordance with Part 2 of Art. 76 of the Federal Law No. 323-FZ 21.11.11 “On the fundamentals of protecting the health of citizens in the Russian Federation” in accordance with methodological recommendations published as a result of a meeting with the main freelance specialists of the Ministry of Health chaired by the First Deputy Minister of Health of the Russian Federation I.N. Kagramanyan, held on March 16, 2016 at the Russian Ministry of Health.
Clinical recommendations are based on evidence-based clinical experience describing the doctor’s actions in diagnosis, differential diagnosis, treatment, and rehabilitation of patients with PHPT.
Clinical recommendations are intended for endocrinologists, and can also be useful for rheumatologists, orthopedists, traumatologists, internists and general practitioners, nephrologists, urologists, gastroenterologists and doctors of other specialties, who are approached by patients with a variety of symptoms of PHPT, characteristic of other diseases of the skeletal system, kidneys, gastrointestinal tract (GIT). Health care providers should adhere to these recommendations when making clinical decisions. At the same time, the recommendations do not replace the personal responsibility of medical workers when making clinical decisions, taking into account the individual characteristics of patients and their wishes.
Methodology for the formation of clinical recommendations
The basis for these clinical recommendations were the existing consensuses and recommendations: materials of the consensus group on primary hyperparathyroidism - “Guidelines for the diagnosis and treatment of asymptomatic forms of primary hyperparathyroidism” - 2009 and 2014. [12]; American Society for Bone and Mineral Research Medical Guide for Clinical Practice on Metabolic Diseases of the Skeleton and Disorders of Mineral Metabolism, 2013[3]; Guide to diseases of the parathyroid glands [4] “Algorithms for examination and treatment of patients in endocrinology, part II. Hyperparathyroidism” - 2009, Russia [5], as well as the results of scientific work on this issue in the Russian Federation.
Description of the method for validating recommendations
These guidelines have been peer-reviewed in draft form. Experts were asked to comment, among other things, on the clarity and accuracy of interpretation of the evidence base underlying the recommendations.
The comments received from the experts were carefully systematized and discussed by the chairman and members of the working group. Each point was discussed and the resulting changes were recorded in the recommendations.
The draft clinical recommendations were posted on the website of the Federal State Budgetary Institution Scientific Research Center of the Ministry of Health of the Russian Federation and on the website of the RAE on 05/11/2016 and presented for discussion to a wide range of specialists on 05/19/2016 within the framework of the Congress “Innovative technologies in endocrinology: diagnosis and treatment of osteoporosis and other metabolic diseases of the skeleton” on the basis of the Federal State Budgetary Institution ENC M.Z. Russia, Dmitry Ulyanov street, 11, Moscow, May 19-20, 2016
Thus, the draft clinical recommendations were discussed among specialists of the teaching staff, health care organizers in the field of endocrinology and practitioners dealing with the problems of hyperparathyroidism.
Methods used to collect/select evidence:
search in an electronic database using keywords. Assessing the quality and relevance of the found sources (Agree).
Description of methods used to collect/select evidence:
the evidence base for the recommendations was publications included in the Cochrane Library, EMBASE and MEDLINE databases, and e-library. The search depth was 10 years due to the presence of two editions of the 2002 consensus revision of international clinical guidelines for the diagnosis, management and treatment of mild forms of PHPT (2008 and 2014), and the publication of practical guidelines on PHPT in 2012 and 2013. When specific medical methods of prevention, diagnosis, treatment and rehabilitation were included in clinical recommendations, the level of strength of evidence, the feasibility of their use was indicated, taking into account the unified scale for assessing the quality of evidence and the strength of recommendations for the use of medical technologies GRADE (used on the recommendation of the Ministry of Health of Russia in collaboration with the American College of Physicians - American College of Physicians: level of evidence (A-D), strength of recommendations (Table 1) [1, 2].
Table 1. Levels of evidence and classes of recommendations
Description of methods used to collect/select evidence:
The evidence base for recommendations is publications included in the Cochrane Library, EMBASE and MEDLINE databases, and e-library. The search depth was up to 10 years.
Methods used to assess the quality and strength of evidence:
• expert consensus;
• assessment of significance in accordance with levels of evidence and classes of recommendations (attached).
Methods used to analyze evidence:
• reviews of published meta-analyses;
• systematic reviews with evidence tables.
Description of the methods used to analyze the evidence.
When selecting publications as potential sources of evidence, the methodology used in each study is examined to ensure its validity. The outcome of the study influences the level of evidence assigned to the publication, which in turn influences the strength of the resulting recommendations.
Methodological examination is based on several key questions that focus on features of the study design that have a significant impact on the evidence and acceptability of the results and conclusions. These key questions may vary depending on the types of studies and questionnaires used to standardize the publication assessment process.
Particular attention was paid to the analysis of materials, original articles, meta-analyses, reviews published after 2006.
The assessment process can undoubtedly be affected by the subjective factor. To minimize potential bias, each study was assessed independently, i.e. by at least two independent members of the working group. Any differences in assessment were discussed by the entire group. If it was impossible to reach consensus, an independent expert was involved.
Evidence tables:
evidence tables were completed by members of the working group.
Methods used to formulate recommendations
: expert consensus.
Good Practice Points (GPPs):
Recommended good practice is based on the clinical experience of the guideline working group members.
Economic analysis:
No cost analysis was performed and pharmacoeconomics publications were not reviewed.
Conflict of interest:
The authors and experts had no conflict of interest when creating clinical guidelines.
Who is at risk?
The following are at risk of developing hyperparathyroidism:
- persons with long-term and severe vitamin D or calcium deficiency;
- women during their menopause;
- persons taking lithium preparations;
- persons suffering from rare hereditary diseases in which the activity of part of the endocrine glands is disrupted;
- patients undergoing radiation therapy.
The following are at risk of developing hypoparathyroidism:
- persons whose close relatives suffer from this disease;
- persons who have undergone certain surgical interventions in the neck area, especially removal of the thyroid gland;
- persons suffering from autoimmune diseases (with such diseases, cells of the immune system begin to destroy the structures of their own body);
- patients undergoing radiation therapy.