Urticaria is one of the most common skin diseases, characterized by the appearance of a skin rash, the primary element of which is a blister.
According to epidemiological studies, urticaria is observed at least once throughout life in 15-25% of the population, and 25% of them have a chronic course of the disease. According to various authors [1–4], 75–95% of patients have chronic idiopathic urticaria (CIU). Chronic urticaria is more common in adults than in children, and is significantly more common in women. Typically, the onset of the disease occurs in the third or fourth decades of life.
Patients complain of low mood, poor sleep, and emotional discomfort, which is partly associated with limited social activity. Although the rash is transient, more than half of patients report problems associated with the disease in daily life.
Clinically, urticarial rashes are accompanied by itching, turn pale when pressed, and present as limited swelling of the papillary dermis. Urticaria rashes can occur in any location, including the scalp, palms and soles. In the head and neck area, the number of skin mast cells per unit area is increased compared to other areas of the skin, therefore urticaria and itching in this localization are characterized by greater intensity [5-10].
Timely initiation of adequate therapy is of great importance for reducing the symptoms of chronic urticaria and improving the quality of life of patients [11-15].
The pathogenesis of urticaria is based on the release in large quantities of the main mediator of mast cells, histamine, into the surrounding tissues and blood. Histamine is synthesized from histidine in mast cells and stored in vesicles called granules. In addition to mast cells, histamine is also released by other cells - basophils, histaminergic nerve cells, however, it is mast cells that are of key importance in the release of the mentioned biologically active substance.
Obviously, research by pharmaceutical companies was aimed at finding drugs that can block the effect of histamine on the body. In 1942, a new era began in the treatment of allergic diseases: the first antihistamine drug was synthesized. The importance of this discovery can hardly be overestimated, as evidenced by the fact that in 1957 Daniel Bovet received the Nobel Prize for the synthesis and study of the properties of antihistamines. The basic therapy for both acute and chronic urticaria is antihistamines. In this regard, histamine H1 receptor blockers are considered the first-line treatment for acute and chronic urticaria. These drugs are reversible H1 receptor agonists and reduce histamine-mediated allergic reactions [16–20].
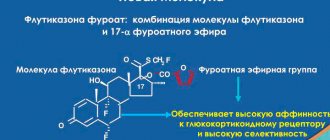
First generation antihistamines (chloropyramine, diphenhydramine, clemastine, cyproheptadine, promethazine, fencarol, hydroxyzine) made it possible to make a significant step forward in the treatment of allergies, but at the same time they had pharmacological features that limited the possibility of their use in a wide range of diseases, especially in chronic allergosis, requiring long-term treatment. They were distinguished by the short duration of the therapeutic effect, which required repeated administration of the drug during the day. Incomplete binding to H1-histamine receptors (about 30%) determined relatively high therapeutic doses of drugs. Due to their properties, first generation drugs are used to achieve a quick effect: they are prescribed in the acute period of an allergic reaction, both as monotherapy and in combination with representatives of other generations of antihistamines. Drugs in this group are indispensable for acute allergic reactions, such as urticaria, angioedema, drug allergies, anaphylactic shock, etc. They have a pronounced antihistamine and anticholinergic effect [21-25].
However, with long-term antiallergic therapy, such drugs have more disadvantages than advantages. This was the reason for the appearance in the second half of the twentieth century of antihistamines of the second generation (terfenadine, astemizole, arivastine, dimethendene, loratadine, levocabaxine, azelastine). They were distinguished by high affinity for H1 receptors, rapid onset of action and sufficient duration. The high selectivity of the drugs ensures the absence of blockade of other types of receptors, which minimizes side effects during use. A low degree or even complete absence of patency of the blood-brain barrier determines the absence of sedation and the dependence of its manifestation on alcohol consumption. A convincing argument in favor of long-term therapy with drugs of this group is the lack of addiction.
The main goal of treating patients with chronic urticaria, regardless of the etiological factor, is to control clinical manifestations and subjective symptoms. They are largely mediated by histamine. In accordance with the clinical recommendations of the II International Conference on Urticaria, the basic therapy drugs are selective H1 receptor blockers. The advantages of these drugs are not only a pronounced effect on the main symptoms of the disease and good tolerability, but also the presence of anti-inflammatory properties. It has been suggested that for treatment-resistant chronic urticaria, it is acceptable to increase the dose of antihistamines in this group up to 4 times compared to the recommended regimens, although the safety and effectiveness of such a choice must be further confirmed in clinical studies.
One of the modern second-generation H1 receptor blockers is bilastine.
- a drug approved for use in the treatment of urticaria, as well as allergic rhinitis.
The purpose of the study is to establish the effectiveness of Nixar
a modern histamine type 1 receptor blocker bilastine in patients with chronic idiopathic urticaria.
Material and methods
On the basis of the clinical diagnostic FSBEI HE Siberian State Medical University of the Ministry of Health of the Russian Federation. From 2022 to 2022, 51 patients diagnosed with “L50.1” were examined. Chronic idiopathic urticaria" aged from 21 to 53 years (average 36.4±3.4 years), including 36 (71%) men and 15 (29%) women. The duration of the disease ranged from several months to 12 years (group average 4.2±1.6 years). All patients had a frequently recurrent course of urticaria (more than 4 exacerbations per year; on average 5.3±0.9 times per year). The main sensitizing factors were household (36.7%), food (13.4%) and epidermal (11.9%) allergens. In the majority of patients with CIC, an exacerbation of the process was noted against the background of concomitant somatic pathology. Diseases of the gastrointestinal tract predominated - in 13 (25.4%) patients; ENT diseases - in 9 (17.6%) patients and endocrine pathology - in 12 (23.5%).
The examination of patients with CIC was carried out in accordance with the standards for diagnosing allergic diseases and included general clinical research methods and a specific allergological examination (R.M. Khaitov et al., 2009).
During the initial consultation, anamnestic data was collected and analyzed, an objective examination was carried out, and data from referral documentation and outpatient observation cards at the place of residence were studied.
The laboratory examination included a complete blood count with a leukocyte count, a general urinalysis, a biochemical blood test (liver function tests, levels of creatinine, urea, cholesterol, protein, glucose), rheumatological tests to determine the level of rheumatoid factor, circulating immune complexes, C-reactive protein, IgA, IgM, IgG, copro-ocystoscopy, as well as examination of patients’ blood serum for the presence of RW, HIV, HBsAg markers. Of the instrumental research methods, ultrasound examination of the abdominal organs and fibrogastroduodenoscopy were mandatory. If concomitant pathology was detected, the patient was referred for consultation to related specialists.
A specific allergological examination included analysis of allergological history data, skin tests with household, epidermal, and pollen allergens. In addition, if the presence of a physical form of urticaria was suspected, a cold application test, determination of the presence of urticarial dermographism, and an exercise test were performed if the presence of a cholinergic form of urticaria was suspected. In order to determine the autoimmune form of CIC, an intradermal test with autoserum was performed. The level of total IgE in the blood serum of patients was also determined. In order to objectify the severity of the main clinical symptoms of CU and evaluate the effectiveness of the therapy, an individual patient diary was developed, in which dynamic changes in the characteristic symptoms of the disease were recorded. It should be noted that patients were randomized into groups.
Criteria for inclusion in the study:
1) age over 18 years;
2) chronic continuous course of urticaria;
3) treatment with antihistamines and/or antileukotriene drugs.
Exclusion criteria from the study:
1) urticaria with an established cause of an infectious, allergic, medicinal or physical nature;
2) histologically confirmed urticarial vasculitis;
3) treatment with glucocorticosteroids, cyclosporine or methotrexate at the start of the study or during the last month before the study;
4) pregnancy and lactation;
5) carriage of hepatitis B and C viruses;
6) mental illness, low level of cooperation, tendency to antagonism, reluctance to participate in the study.
All patients received treatment: Nixar
(bilastine) at a dose of 20 mg/day (group 1,
n
=24) and at a dose of 40 mg/day (group 2,
n
=27). The duration of prescribed drug therapy was 15 days.
The effectiveness of treatment in patients with CIC was assessed using the Dermatological Quality of Life Index (DIQL) and the Urticarial Activity Score (UAS 7), which allows the patient to make a summary assessment of the main symptoms of the disease (number of rashes and intensity of itching). Disease activity is assessed every 24 hours for 15 consecutive days (see table).
Assessing urticaria activity Note: Indicator rating: 0 - no itching or rash; 0-6 points - well-controlled urticaria; 7-15 points - mild severity of urticaria; 16–27 points—moderate urticaria; 28-42 points - severe urticaria. This scale makes it possible to objectify the assessment of the severity of the disease and the dynamics of its course, as well as to monitor treatment. UAS7 indicators can be a significant criterion for justifying a change in therapy.
The physical and psycho-emotional state of patients, as well as the comfort of treatment, were assessed using the quality of life index. We used a standardized questionnaire in the form of patients assessing their condition, which has advantages in terms of simplicity and speed of use. The DQQ included 10 questions, each of which was scored on a 3-point system (the maximum possible score is 30 points). The questionnaire is filled out by patients independently.
Nixar tablets 20 mg, 10 pcs.
Manufacturer
Faes Pharma S.A., Spain
Compound
Active substance:
- bilastine - 20.00 mg;
Excipients:
- microcrystalline cellulose - 103.00 mg,
- sodium carboxymethyl starch (type A) - 1.00 mg,
- colloidal silicon dioxide - 0.50 mg,
- magnesium stearate - 0.50 mg.
pharmachologic effect
Antiallergic agent - H1-histamine receptor blocker.
Pharmacodynamics:
Bilastine is a long-acting antihistamine that selectively blocks peripheral H1 receptors.
A significant therapeutic effect is observed one hour after taking the drug, the antihistamine effect persists for 24 hours.
A slight penetration of bilastine through the blood-brain barrier is possible, but bilastine does not have a significant effect on the central nervous system and does not cause a sedative effect.
Does not have anticholinergic effect. There is no prolongation of the QT interval on the ECG.
Pharmacokinetics:
Suction. After oral administration, bilastine is rapidly absorbed from the gastrointestinal tract. The time to reach maximum plasma concentration (TCmax) is 1.3 hours. The bioavailability of bilastine when taken orally is 61%. Concomitant food intake reduces the bioavailability of bilastine by 30%. No accumulation of the drug is observed. Connection with blood plasma proteins - 84-90%.\
Metabolism and excretion. Bilastine is metabolized slightly; after a single dose, up to 95% of bilastine from the dose taken is excreted unchanged by the kidneys (28.3%) and bile (66.5%). The half-life (T1/2) averages 14.5 hours.
In renal failure of moderate severity (glomerular filtration rate (GFR) 30-50 ml/min/1.73 m2) and severe severity (GFR < 30 ml/min/1.73 m2), the rate of bilastine elimination slows down, which can lead to to increase the concentration of bilastine in the blood plasma.
Changes in pharmacokinetic parameters do not affect the safety profile of bilastine, since the concentration of bilastine in the blood plasma in patients with renal failure remains within acceptable values.
In case of liver failure, clinically significant changes in the pharmacokinetic parameters of bilastine do not occur, since bilastine is slightly metabolized in the liver.
The pharmacokinetic parameters of bilastine in elderly patients are similar to those in young patients.
Indications
- Allergic (seasonal and year-round) rhinoconjunctivitis: elimination or relief of symptoms (sneezing, feeling of nasal congestion, itching of the nasal mucosa, rhinorrhea, burning and itching sensation in the eyes, redness of the eyes, lacrimation);
- urticaria: elimination or reduction of skin itching, rash.
Contraindications
- Hypersensitivity to bilastine or auxiliary components of the drug;
- age up to 12 years (efficacy and safety have not been established);
- pregnancy and breastfeeding period.
Side effects
Possible side effects are listed below in descending frequency of occurrence: very common (≥ 1/10), common (≥ 1/100, <1/10), uncommon (≥1/1000, <1/100), rare (≥1 /10000, < 1/1000), very rarely (< 1/10000), including isolated messages.
Gastrointestinal disorders Uncommon: dry mouth, diarrhea, dyspepsia, gastritis, abdominal pain, upper abdominal pain, stomach discomfort, nausea.
Skin and subcutaneous tissue disorders Uncommon: pruritus.
Nervous system disorders Common: drowsiness, headache; Uncommon: dizziness.
Mental disorders Uncommon: anxiety, insomnia.
Metabolic disorders Uncommon: increased appetite, weight gain.
Hearing and labyrinthine disorders Uncommon: tinnitus, vertigo.
Disorders of the respiratory system, chest and mediastinal organs. Uncommon: shortness of breath, dry nasal mucosa, discomfort in the nose.
Cardiovascular disorders Uncommon: right bundle branch block, sinus arrhythmia, prolongation of the QT interval on the electrocardiogram, other changes on the electrocardiogram.
Infectious and parasitic diseases Uncommon: herpetic lesions of the oral cavity.
Other: Uncommon: thirst, increased fatigue, asthenia, fever, increased concentration of triglycerides in the blood plasma, increased concentration of creatinine in the blood plasma, increased activity of liver enzymes (aspartate aminotransferase, alanine aminotransferase, gamma-glutamyltransferase).
Interaction
With simultaneous use of bilastine with ketoconazole or erythromycin, the area under the concentration-time curve (AUC) of bilastine increased by 2 times, and the maximum concentration (Cmax) increased by 2-3 times.
With simultaneous use of bilastine at a dose of 20 mg and diltiazem at a dose of 60 mg, the Cmax of bilastine increased by 50%. Such effects can be explained by interaction at the level of carrier proteins (including P-glycoprotein) responsible for the excretion of drugs from intestinal cells, the substrate of which is bilastine.
With the simultaneous use of bilastine and other drugs that are substrates or inhibitors of P-glycoprotein (for example, cyclosporine), the concentration of bilastine in the blood plasma may increase.
Grapefruit and other fruit juices reduce the bioavailability of bilastine by 30%. This interaction is due to the ability of fruits to suppress the activity of the organic anion transport protein OATP1A2, for which bilastine is a substrate. Medicines that are substrates or inhibitors of OATP1A2 (for example, ritonavir or rifampicin) may reduce the plasma concentration of bilastine.
Bilastine does not enhance the effect of ethanol on the central nervous system.
With the simultaneous use of bilastine and lorazepam, no enhancement or suppressive effect of lorazepam on the central nervous system was detected.
How to take, course of administration and dosage
Inside.
Unless otherwise prescribed by your doctor, the following doses of Nixar are recommended to relieve symptoms of allergic rhinoconjunctivitis and urticaria:
Adults and children over 12 years of age: 1 tablet of Nixar, which corresponds to 20 mg of bilastine, once a day.
The maximum daily dose of bilastine is 20 mg, since increasing the dose does not lead to an increase in the therapeutic effect. The tablet is taken one hour before a meal or 2 hours after a meal (or fruit juice).
For allergic rhinoconjunctivitis, the drug is used throughout the entire period of contact with allergens.
For urticaria, treatment is continued until symptoms disappear or improve.
In patients with impaired liver and kidney function, no dose adjustment is required.
In elderly patients, no dose adjustment is required. There is little experience with the use of Nixar® in people over 65 years of age.
Overdose
Symptoms: when using bilastine at a dose 10-11 times higher than the recommended dose, side effects occurred 2 times more often than when using placebo.
The most frequently reported symptoms were: dizziness, headache, nausea. No serious side effects, including significant prolongation of the QT interval, were noted.
Treatment: symptomatic and supportive therapy. There is no specific antidote.
Special instructions
In patients with moderate renal failure (GFR 30-50 ml/min/1.73 m2) and severe renal failure (GFR < 30 ml/min/1.73 m2), simultaneous use with P-glycoprotein inhibitors may lead to increased concentrations of bilastine in blood plasma, which increases the risk of side effects.
In this regard, in patients with moderate to severe renal failure, caution must be exercised when using bilastine simultaneously with P-glycoprotein inhibitors (ketoconazole, erythromycin, cyclosporine, ritonavir, diltiazem, etc.).
Impact on the ability to drive vehicles. Wed and fur.:
In a study conducted to evaluate the effect of bilastine at a dose of 20 mg on the ability to drive vehicles, no negative effect of the drug was detected.
However, patients should be warned that in very rare cases, dizziness and drowsiness may occur, which in turn may affect the ability to drive or perform other activities that require increased concentration.
If the described adverse events occur, you should refrain from performing these activities.
Active substance
Bilastine
Conditions for dispensing from pharmacies
On prescription
Dosage form
pills
Purpose
For children over 12 years old, For adults
Indications
Allergic conjunctivitis, Allergy, Urticaria, Allergic rhinitis
Barcode and weight
Barcode: 4013054022887 Weight: 0.010 kg
results
During the research work, informed consent was obtained from patients to participate in this research project. In the 1st group, patients used the drug in a daily dose of 20 mg; in the 2nd group, patients with CCI used Nixar
(bilastine) at a daily dose of 40 mg. An increase in the dose of a second generation antihistamine was carried out in accordance with the federal clinical guidelines for the management of patients with urticaria RODVC (2015) in patients of the 2nd group, whose history was marked by resistance to previous therapy.
For an objective assessment of the therapeutic effectiveness of Nixar
(bilastine) in patients with CHI, the dynamics of clinical manifestations of urticaria were observed (the number of morphological elements during the day) using the UAS7 urticaria activity severity scale; the psycho-emotional state of patients, as well as the comfort of treatment, were assessed using the DIQ before treatment, at 5, 10 and 15 -th day.
During observations of patients with CIC, the following results were obtained: changes in the urticaria activity scale (Fig. 1)
Rice.
1. Change in urticaria activity scale UAS 7 when taking Nixar at a dose of 20 mg/day (n=24) and 40 mg/day (n=27). in the group with a daily dose of 20 mg were 30.4, 23.6, 15.2 and 9.4 points ( p
<0.05) before treatment, on days 5, 10 and 15, respectively;
in the group with a daily dose of 40 mg, this indicator was recorded at the level of 31.1, 20.1, 12.1 and 3.6 points ( p
<0.05), respectively, before treatment, on the 5th, 10th and 15th day.
In accordance with the data obtained, in the group with an increased daily dose of the drug Nixar
(bilastine), a decrease in scores on the urticarial activity scale UAS 7 (Urticarial Activity Score) was recorded by 61.8% compared to group 1, where the drug was used at a daily dose of 20 mg.
When analyzing standardized DIQL questionnaires for patients participating in a post-registration clinical trial, the following results were obtained (Fig. 2):
Rice.
2. DIG when taking Nixar at a dose of 20 mg/day (n=24) and 40 mg/day (n=27). in group 1 on days 5, 10 and 15, respectively 18.3, 14.6, 8.4 and 5.3 ( p
<0.05), in group 2 - 19.1, 12.1 , 4.2 and 2.3 (
p
< 0.05).
According to the data obtained, the quality of daily life over time changed more positively in group 2, where the daily dose of the drug Nixar
(bilasin) was 40 mg, which was reflected in a more pronounced change in the DIQI index by 46.6% compared to group 1 .