What you need to know about spotting
The content of the article
Any blood loss that occurs outside of the normal menstrual cycle should be assessed by a gynecologist, whether it is mild (spotting) or heavy bleeding.
However, note that, according to numerous scientific sources, one of the most common causes of intermenstrual bleeding is stress, so this symptom should not lead to premature alarms and concerns about malignancy.
Bleeding often occurs as a single symptom, but it can also be accompanied by other symptoms associated with the underlying pathology:
- pain in the abdomen or pelvis;
- vaginal discharge;
- asthenia and general malaise;
- nausea and vomiting;
- fatigue and feeling tired;
- pallor and tachycardia.
Tachycardia
Diagnosis of such conditions is based on recognition of the symptom and associated signs. It is also important to immediately perform instrumental tests, for example, transvaginal ultrasound, which is necessary to identify organic pathologies.
Therapy depends on the cause of the bleeding, as well as on the woman’s age and her desire to have offspring; the choice of method lies with the gynecologist.
Determination of intermenstrual bleeding in the middle of the cycle
Menstruation is one of the phases of the menstrual cycle of the female body, characterized by the release of blood from the vagina. The beginning of the menstrual cycle is counted from the first day of menstruation.
Sometimes it can be difficult to distinguish dysfunctional uterine bleeding from normal menstruation. Many girls do not remember when their menstrual cycle began and do not know how to calculate their menstrual cycle, so they may mistakenly think that menstruation came earlier or later than expected. For each woman and girl, the duration of the monthly cycle is individual
How to calculate the monthly cycle? It is not difficult. The easiest way is to keep a monthly calendar. It needs to mark 1 day of the onset of menstruation and 1 day of the next menstruation. The number of days between them will be the duration of the menstrual cycle. You need to know that normal menstruation lasts 2-7 days, and the normal menstrual cycle is 21-35 days. The most optimal duration of the monthly cycle is 28 days. Women who experience an irregular menstrual cycle should consult a gynecologist.
Ovulation is the process of the release of a mature egg from the follicle. In women with a normal monthly cycle, ovulation occurs approximately on the 14th day from the start of menstruation. With an irregular menstrual cycle, it may occur earlier or later than this time. After ovulation, the level of estrogen in the female body decreases, and bleeding does not occur because the corpus luteum maintains hormonal balance. A sharp increase or decrease in the level of the hormone estrogen during ovulation can provoke uterine bleeding between, before and after menstruation, and this is not a deviation from the norm. This phenomenon is observed in 30% of women.
The main causes of vaginal pathological bleeding
There are many causes of vaginal bleeding, but they can generally be grouped into 5 broad categories:
Complications during pregnancy (sometimes undiagnosed, that is, which the woman does not yet know about) include:
- abortion (miscarriage);
- ectopic pregnancy;
- gestational trophoblastic disease.
Dysfunctional reasons:
- anovulatory cycles;
- polycystic ovary syndrome;
- less often metrorrhagia.
Benign organic pathologies:
- uterine fibroids;
- uterine polyps;
- adenomyosis;
- endometriosis;
- genital infections.
Malignant organic pathologies:
- endometrial cancer;
- cervical cancer;
- vaginal cancer;
- sarcomas.
Common systemic causes:
- blood clotting pathologies;
- leukemia;
- hypothyroidism;
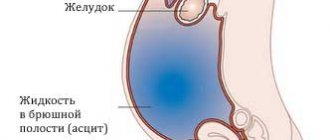
- liver and kidney failure.
Spotting may occur during the first cycles of taking hormonal contraceptives (birth control pills) and after using the hormonal IUD.
Bloody discharge during pregnancy
Light spotting is common in the early weeks of pregnancy, but heavy bleeding can occur in the third trimester of pregnancy and poses a serious risk to both mother and fetus.
The severity of bleeding is assessed by:
- volume - small drops or real bleeding;
- duration;
- blood characteristics;
- accompanying symptoms.
There are many reasons for bleeding during pregnancy, including:
- urinary tract infections or hemorrhoidal disease (bleeding in which is misunderstood as blood loss of genital origin);
- polyps in the cervix;
- cervical carcinoma;
- placenta previa (abnormality of the placenta);
- placental abruption before childbirth;
- abortion (miscarriage);
- ectopic pregnancy (the embryo, instead of implanting in the uterus, implants in other areas, especially often in the fallopian tubes);
- gestational trophoblastic disease.
Polyps in the cervix
Both in the presence of bloody discharge and in case of more significant blood loss, the patient is always recommended to consult a doctor. If spotting in the first trimester is physiological in nature, when the bleeding was especially heavy, hospitalization would become mandatory.
Almost always in the third trimester of pregnancy, therapeutic treatment includes:
- If the presentation is mild, close monitoring of symptoms is necessary until vaginal delivery eventually occurs;
- If the clinical picture is severe, emergency treatment with continuous cardiotocography (for fetal monitoring) and immediate cesarean section should be performed.
Intense bleeding in the first weeks after childbirth or after an abortion can occur when the uterus has not yet restored its physiological size, or in case of imperfect (insufficient) cleaning of the internal walls.
Poor blood flow during pregnancy
During pregnancy, it is extremely important to continuously monitor the state of the maternal body of the mother and the baby, it is important that they perform all vital functions. One of the most significant studies is the analysis of blood flow in the arteries of the uterus, the woman’s umbilical cord, as well as cerebral vessels and the fetal aorta. The main causes of perinatal morbidity and mortality include disorders of the uteroplacental blood flow of 1A, 1B, second and third degrees.
Blood flow in the placenta
The placenta, in which the fetus is located, supplies the embryo with nutrients, as well as oxygen from the mother’s blood; it also removes waste products from the child’s body. It is this organ that unites two rather complex vascular systems - the female, which connects the vessels of the uterus and placenta, and the fetal, which passes into the umbilical arteries and leads to the child.
The circulatory systems mentioned above are separated by a membrane, which does not allow maternal and child blood to mix. The placenta is a kind of barrier that is resistant to numerous harmful substances, as well as viruses.
Often, for completely different reasons, placental insufficiency may appear, which inevitably affects the performance of transport, metabolic, trophic, endocrine and other vital functions of the placenta. In this condition, the metabolism between the maternal and child organisms deteriorates significantly, which is fraught with various consequences.
What are the causes of impaired placental blood flow?
Poor circulation in the uterine cavity can be caused by pneumonia, increased blood pressure, various intrauterine infections, as well as insufficient oxygen supply to the child’s body (hypoxia).
To diagnose the blood flow system in modern obstetric practice, three-dimensional ultrasound (so-called Doppler ultrasound) is used, with which the vessels are visible in a 3D (three-dimensional) image. With the help of this diagnostic technique, there is a prospect of diagnosing retroplacental bleeding and assessing cardiac malformations by monitoring blood flow. This technique is irreplaceable, since with its help it is possible to examine defects even in the most microscopic vessels that form the microvasculature, to observe the peculiarities of the formation and development of intraplacental hemodynamics, and in addition to control the amount of nutrients, as well as oxygen, that should enter the fetal body . New prospects have opened up for the early detection of obstetric complications, and if treatment or correction is started without wasting time, then circulatory disorders and subsequent pathologies associated with it can be almost completely avoided.
Hemodynamic disorders during pregnancy
Hemodynamic disorders are divided into 3 degrees of severity:
1. 1st degree includes two subtypes:
- disturbance of patello-placental blood flow 1Is the mildest. Fetal-placental blood circulation is preserved with it. Intrauterine infections often lead to this problem;
- in degree 1B, uteroplacental blood flow is preserved, but fetal-placental pathologies appear.
2. Grade 2 is characterized by the presence of disturbances in both blood flow systems, however, these disturbances do not carry any fundamental changes. 3. In grade 3, uterine circulation disturbance causes defects in normal blood circulation at the level of the fetus.
In the case of the first degree of violations, timely detection and adequate treatment can avoid fetal death. In the case of the second degree, perinatal mortality is about 13.3 percent, in the case of the third - 46.7 percent. During Doppler diagnostics, it was revealed that treatment aimed at correcting placental insufficiency in women with third-degree uterine blood flow disorders was ineffective. In this situation, with conservative childbirth, perinatal mortality was 50 percent, then, thanks to a cesarean section, losses can be avoided. 35.5 percent of newborns are admitted to the intensive care unit with grade 1 blood flow disorders, 45.5 percent with grade 2, and 88.2 percent with grade 3.
Dysfunctional reasons
Anovulatory cycles are those cycles during which normal ovulation does not occur. The basis may be hormonal changes in FSH and LH, estrogen and progesterone. The imbalance causes excessive growth of the endometrium, which sloughs off irregularly at the end of the cycle, causing bleeding even outside the normal menstrual cycle, often long and heavy.
Polycystic ovary syndrome is a disease that affects young women between the ages of 20 and 40. It is characterized by anovulation (in the absence of a normal menstrual cycle and infertility), hirsutism, acne, insulin resistance with an increased risk of developing type 2 diabetes.
By menorrhagia we mean a pathological increase in the amount and duration of menstrual flow, which, however, in this case usually occurs at the end of the cycle.
Stress and eating disorders (anorexia nervosa, bulimia, etc.) can lead to intermenstrual losses and abnormal cycles, as well as metabolic diseases (metabolic syndrome) and hormonal dysfunctions, such as thyroid disease.
By metrorrhagia we mean heavy vaginal bleeding that occurs outside of the normal menstrual cycle.
Brown intermenstrual secretion as a manifestation of a physiological norm
The mucous secretion, rejected by the woman’s body during the intermenstrual period, is designed to perform cleansing, protective and supporting functions for the vaginal microflora. Most representatives of the fair sex notice that by the middle of the menstrual cycle, approximately 12–13 days, the consistency, volume and color of this liquid changes. This phenomenon is directly related to ovulation and the preparation of the reproductive system organs for a possible pregnancy. Gynecologists claim that the appearance of bloody spotting on a woman’s underwear during the intermenstrual period does not indicate physiological processes, but despite this, cases are allowed in which this phenomenon is not considered a symptom of a disorder in the reproductive organs.
Benign organic pathologies
Uterine fibroids and endometrial polyps are among the most common causes of vaginal bleeding during the fertile phase. The former are nothing more than abnormal growths of muscle tissue, and the latter - the endometrial mucosa. They can increase in size and often, in combination with hormonal changes, cause bleeding in the form of menorrhagia and metrorrhagia. In this category, it is also important for us to consider ovarian cysts.
Endometriosis means the abnormal presence of endometrium in organs other than the uterus, such as the ovary, fallopian tube, peritoneum, vagina, intestines, lungs. These ectopic lesions may also bleed during the normal menstrual cycle.
Occasional light-colored spotting, possibly worsening with sexual intercourse, may be caused by the presence of an ectropion (an "ulcer" on the cervix).
Genital infections can cause various types of vaginal discharge, but only rarely do they cause bleeding. The most common are those that are sexually transmitted - chlamydia and gonorrhea.
Endometritis
Brown discharge may be a sign of chronic endometritis - inflammation of the endometrium, the mucous membrane of the uterine cavity. Brown discharge with endometritis appears before and after menstruation and often has an unpleasant odor. Sometimes brown mucus appears in the middle of the cycle and is combined with aching pain in the lower abdomen. Chronic endometritis is dangerous during pregnancy; it can lead to miscarriages at different stages. This pathology is due to the fact that the process of attachment of the fertilized egg in the uterine cavity and its further development are disrupted.
Chronic endometritis can result from:
- acute postpartum or post-abortion endometritis that has not been completely cured;
- intrauterine interventions;
- imbalance between the body's hormonal and immune systems;
- hidden infections.
Malignant organic pathologies
They most often occur in the perimenopausal period and consist of malignant tumors of the genital organs. Most common:
- cervical cancer (the most important risk factor is human papillomavirus infection);
- endometrial cancer;
- ovarian cancer;
- cancer of the vagina and vulva.
Ovarian cancer
These are pathologies with a very poor prognosis if they are not recognized in time and treated.
Common systemic causes
These are systemic pathologies that can affect several systems, which among the symptoms can also produce vaginal bleeding.
For example:
- bleeding disorders such as hemophilia A and B, von Willebrand disease, platelet function disorders;
- leukemia and lymphomas;
- liver failure;
- renal failure;
- severe dysthyroidism.
An important and fundamental classification for tracking the various causes of vaginal bleeding is the classification by age group.
Causes of vaginal bleeding by age group
In girls, bleeding before menarche (the first menstrual cycle) should always be carefully investigated). Possible causes of the pathology:
- vulvovaginitis;
- vaginal neoplasms;
- accidental injury;
- foreign bodies;
- violence;
- premature puberty;
- hormonal tumors;
- accidental use of certain drugs.
Causes of intermenstrual bleeding in adolescence and subsequent years:
- inability to ovulate;
- polycystic ovary syndrome;
- changes in coagulation;
- pregnancy (even unrecognized);
- sexually transmitted diseases;
- violence.
Causes of intermenstrual bleeding during the reproductive period:
The predominant cause is menorrhagia (heavy and prolonged menstrual flow), associated with benign organic pathologies - fibroids, polyps. In this category, bleeding due to problems during pregnancy is also likely.
Causes of intermenstrual bleeding in perimenopause: in this age group there is a very high risk of developing an organic malignant disease (genital cancer).
Causes of intermenstrual bleeding during menopause: during the postmenopausal period, benign causes predominate, such as endometrial and vaginal atrophy, endometrial polyps and, much less frequently, malignant tumors.
Types of intermenstrual bleeding
Intermenstrual bleeding often occurs 10-16 days after the end of the last menstrual period. They are not very abundant and last from 12 to 72 hours. But if the bleeding lasts longer or gets worse, consult your gynecologist.
Spotting in the middle of the cycle is more common than intermenstrual bleeding. A woman's vagina comes out with a little blood that can barely be seen on the toilet paper. This is usually mucus that has a pinkish color. Such discharge appears approximately 14 days before the onset of menstruation and is not a pathology. Intermenstrual bleeding indicates that the egg is ready for fertilization.
Frequent periods can also occur with proyomenorrhea (short monthly cycle). Periodically appearing and usually not intense bleeding lasts 2-3 days. Such spotting is caused by premature rejection of the uterine mucosa due to a decrease in estrogen production in the middle of the menstrual cycle.
Symptoms
Along with vaginal bleeding, other symptoms sometimes occur due to the underlying pathology. The most common:
- abdominal or pelvic pain (due to anovulation and other causes);
- vaginal discharge (with genital infection);
- asthenia and general malaise;
- nausea and vomiting;
- feeling tired;
- pallor and tachycardia associated with anemia secondary to bleeding that reduces hemoglobin levels.
Diagnostics
The diagnosis is made based on observation of symptoms and the general clinical picture associated with the use of instrumental studies.
Gynecologist assesses bleeding characteristics:
- duration;
- intensity;
- associated symptoms;
- main pathologies.
If the bleeding is quite cyclical and regular, it is likely due to benign organic lesions or anovulation. If bleeding is irregular, the possibility of malignancy should also be considered.
Blood tests are performed to assess whether the patient has anemia, which in severe cases requires supportive care, including blood transfusion.
Blood tests
From an instrumental point of view, the gold standard for diagnosing vaginal bleeding is transvaginal ultrasound, which can identify both benign and malignant organic lesions, evaluate the characteristics of the endometrial mucosa and any changes in the ovaries.
The ultrasound results may then require other methods such as
- CT scan of the abdomen and pelvis;
- Nuclear magnetic resonance;
- In case of organic lesions - hysteroscopy and endometrial biopsy.
But first of all, the possibility of pregnancy is always excluded using an hCG test.
Doctors' opinion
According to experts, spotting cannot be ignored. After all, they can cause hormonal imbalance, pathologies, and diseases. And in this case, timely treatment will provide effective results.
According to doctors, urine with blood in women without pain is not always a pathology, but still requires diagnosis. In this case, a number of examinations are carried out:
- General urine and blood tests that reveal inflammation and suggest what actions the doctor needs to take in the future.
- Biochemical tests, thanks to which it is possible to determine the content of components such as proteins.
- A three-glass urine test, with which you can clearly determine the cause of the appearance of blood.
- The Nechiporenko urine collection method, which reveals a more detailed picture of the disease.
- Bacterial urine analysis, thanks to which you can determine the type of infectious agents (if any).
- Ultrasound of the genitourinary system - shows the condition of the woman’s organs.
- X-ray of the kidneys and reproductive system is necessary if the ultrasound did not give a complete picture.
- Cystoscopy, urethroscopy - in this case, a smear is taken for biochemistry to exclude the presence of dangerous diseases.
- CT and MRI are indicated only for those women in whom doctors suspect the presence of tumors.
Each of these studies is very important, but a urine test should be ordered first. With its help, the doctor determines the basic picture of the disease and draws up a plan for further action.
Doctors also insist that you should not self-medicate. Only after a complete examination is complex therapy or surgery prescribed, and the patient must constantly notify the gynecologist about his condition. In this case, we can talk about a quick solution to the problem and the return of health to the woman.
Treatment and reasons for choosing a therapy method
Treatment depends only on the underlying cause of the bleeding. Once identified, drug therapy (dysfunctional causes) or surgical intervention (malignant formations) may be required.
A woman should always choose the most appropriate treatment, including taking into account her age or her desire to have children. This allows you to increase patient adherence to therapy, as well as achieve maximum success.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.