General information
Hyperkeratosis is a pathological process in the epidermis, which is based on accelerated growth and disruption of the desquamation process of the epidermis, manifested by hypertrophy (thickening) of the stratum corneum. Hyperkeratosis is not an independent disease. Disruption of the keratinization process and thickening of the stratum corneum can occur both in healthy people (on the feet, elbows, knees) and in various diseases ( erythroderma , lichen , ichthyosis , etc.). The process of keratinization, depending on the reasons, can occur in different parts of the body; the thickness of the keratinized layer can vary significantly (from a millimeter to 1-2 centimeters).
What is the stratum corneum of the epidermis?
At the base of the stratum corneum of the skin are horny plates containing the protein keratin. In thin skin, the stratum corneum includes 15–20 layers of horny scales, and in thick skin it can contain up to 100 or more layers. The stratum corneum is the final product of the differentiation process of epidermal keratinocytes, which has a specific structure, defined as “brick and cement,” in which horny cells act as “bricks” and intercellular lipids act as “cement.” The leading mechanism of epidermal renewal is the process of desquamation of horny scales and their replacement with new cells. The renewal process begins in the basal layer, producing keratinocytes, which, as they grow older, gradually move (pushed out) to the upper layers, losing the nucleus and organelles, turning into flat scales (corneocytes), forming the stratum corneum (Fig. below).
Thus, the mechanism of cellular renewal is based on the separation (exfoliation) of the upper horn cells, which provokes the activation of dermal cells and the formation of new mother cells of the basal layer. The renewal cycle of epidermal cells averages 21-28 days, but as the body ages, it slows down, amounting to 35-45 days in people over 40 years of age and 56-72 days after 50 years of age. The state and duration of the cellular metabolism cycle also depends on other factors: nutrition/lifestyle, hormonal levels, negative environmental factors.
The renewal process is characteristic not only of the skin epithelium, but also of the mucous membranes of the oral cavity, uterus, and vulva. However, due to differences in the structure of the mucosal epithelium (for the most part, the horny, granular and lucid layers are absent), during the renewal process, incomplete keratinization (parakeratosis) occurs, which is characterized by the appearance of the surface layer of squamous keratin epithelium in the protoplasm of the cells, but nuclei are still present . Parakeratosis is a physiological property of the mucosal epithelium, and is qualified as a pathological process when the morphology of the keratinizing squamous epithelium is disrupted. At the same time, parakeratosis is often combined with hyperkeratosis and acanthosis (increased proliferation of the spinous/basal layers).
Hyperkeratosis is an urgent problem both among men, which is faced by almost 20% of people after 20 years of age, and among women, among whom more than 40% after 20 years of age note this phenomenon on those other areas of the skin that significantly worsen the appearance of the skin (color, structure ). follicular hyperkeratosis occurs predominantly . More often in a child 1-3 years old, the face and hands are affected. In adults, the most common hyperkeratosis of the feet and, in particular, hyperkeratosis of the toenails, subungual hyperkeratosis of the hands, hyperkeratosis of the facial skin and hyperkeratosis of the scalp.
Despite the fact that hyperkeratosis, regardless of its type, is not a potentially life-threatening condition, it requires mandatory treatment, since cosmetic defects/deterioration of the aesthetics of the skin can cause a decrease in self-esteem and contribute to the development of psychological trauma and social maladjustment, especially among women .
How does follicular hyperkeratosis develop?
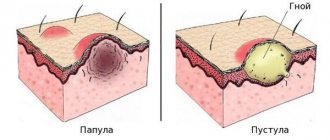
It is considered normal that when the lumen of the follicular canal contains a thin layer of corneocytes, its rejection occurs quite easily. But if microcomedones form - blockage of the follicles - this process slows down. Impaired desquamation can lead to retention hyperkeratosis, the formation of dense plugs of keratin, sebum and bacteria in the orifices.41
The structure of the follicle suggests the presence of an acroinfundibulum (its upper part) and an infrainfundibulum. With hyperkeratosis of the first, open comedones are formed, when increased keratinization concerns the second - closed comedones. 41
In closed comedones, the level of oxygenation is very low, and the drainage of metabolites of propionibacteria and sebum is blocked. The dark color of open comedones is associated with the accumulation of melanin. 41
Classification
The classification of hyperkeratoses is based on a number of factors, according to which the following are distinguished:
- By origin: hereditary and acquired hyperkeratosis .
- By area of damage: local (calluses/warts) and diffuse, occupying large areas of the skin.
According to clinical forms:
- Follicular hyperkeratosis - in which exfoliating scales of the stratum corneum clog the ducts of the follicles, which is manifested by the appearance of numerous small tubercles on the skin.
- Seborrheic hyperkeratosis is localized mainly on the scalp, less often on the facial skin. It manifests itself in the formation of areas of peeling in the form of an easily detachable greasy crust, after which reddish spots remain.
- Warty hyperkeratosis . It is characterized by the appearance on the skin of formations that outwardly resemble warts, but without the etiological factor of true warts - papillomavirus .
- Hyperkeratosis of the feet . It manifests itself as thickening of the skin of the feet with the appearance of corns and calluses.
- Disseminated hyperkeratosis . It appears as polymorphic elements on the skin of the trunk and limbs, reminiscent of thick/short hair, located separately and not merging with each other.
- Lenticular hyperkeratosis . It is characterized by the appearance of horny papules on the hair follicles of the lower extremities, and after removal, small indentations remain on the skin.
- Senile hyperkeratosis . The appearance of dark keratinized spots on the skin of older people is typical.
Stages of development
The following stages of disease development are distinguished:
- First . In some areas, the skin turns pale and becomes dry. No thickening of the stratum corneum has yet been observed.
- Second. When touching the skin, particles falling off are noticeable. Slight thickening is possible.
- Third . The skin peels off greatly and loses its smoothness, becoming rough and rough to the touch.
- Fourth. At this stage, multiple complications arise that lead to serious changes in the appearance of the epidermis. The thickening of the stratum corneum is visible to the naked eye.
Causes
The etiological factors for the development of hyperkeratosis are quite numerous. There are causes of exogenous and endogenous origin.
Exogenous causes include: mechanical factor (physical pressure on the skin - shoes, clothing, foot deformity, increased body weight, etc.); failure to comply with personal hygiene rules; occupational hazards; injuries; unfavorable environmental factors (solar insolation, frost, wind); bacterial infections.
Endogenous causes include systemic diseases and skin diseases: diabetes mellitus ; fungal infections ; psoriasis ; various forms of lichen ; ichthyosis of the skin ; hypovitaminosis ; frequent/prolonged stress; gastrointestinal diseases; erythroderma ; hormonal imbalances.
Hereditary diseases are a relatively rare cause. Nepotism may also be present in generations: if keratosis is present in the parents, then, with a high probability, hyperkeratosis in the child will also develop sooner or later.
What links in pathogenesis are affected by Clindovit®?
Clindovit® is a topical antibiotic that is active against most strains of propionibacteria6. When applied to the skin, it reduces free fatty acid levels from approximately 14 to 2%6. The main active ingredient of the drug is clindamycin6. The base also contains auxiliary components: emollient and allantoin6.
Since Clindovit® is an antibiotic, it is recommended to combine it with other drugs, for example, benzoyl peroxide or azelaic acid (Azelik®)12. In particular, azelaic acid normalizes keratinization processes and helps eliminate follicular hyperkeratosis40.
Symptoms
The symptoms of hyperkeratosis are determined by its form. Let's look at just a few of them.
Follicular hyperkeratosis
Typical manifestations of the disease are the “goose bumps” rash, which is dense, small, spiky-shaped, reddish pimples at the base of the hair follicle, appearing against a background of rough/rough skin. The predominant localization is on the lateral/back surfaces of the thighs, on the arms, and buttocks - on the lateral and anterior surfaces of the arms and thighs. Follicular hyperkeratosis of the facial skin is much less common . Generalized forms may also occur, which are characterized by extensive damage to the skin of the trunk, buttocks and extensor surfaces of the extremities. The disease does not cause any deterioration in well-being, except for a feeling of slight discomfort due to dry skin. Patients are less likely to experience mild itching (Figure below).
There are two types of the disease:
- Follicular hyperkeratosis type I (develops due to vitamin A deficiency in the body). At the same time, the neck of the hair follicle is surrounded by spiny-type nodules and plaques. The skin in the area becomes rough, dry and defatted, resembling sandpaper when touched.
- Follicular hyperkeratosis type II . The nature of the rash is hemorrhagic. Its development is based on a lack of vitamin C and K in the body. With this type, the ducts of the hair follicles are clogged with blood/pigment and have a red or brown color. The extensor surfaces of the thighs and the abdominal area are most often affected (Fig. below).
Nodules of follicular hyperkeratosis can become infected when trying to squeeze them out independently or during involuntary trauma, which manifests itself as secondary pyoderma . It occurs more often in childhood/adolescence when the body is allergic.
Hyperkeratosis of the feet (plantar hyperkeratosis)
Characterized by dryness/coarsening of the skin of the sole or locally in the heel area, the appearance of calluses and bleeding cracks, which is accompanied by severe pain and even dysfunction of the lower limb. The growth of the stratum corneum can reach 0.5-1.5 cm (Fig. below).
Among plantar hyperkeratoses, the following are distinguished (podological classification):
Dry callus is a local focus of uniform thickness with clear boundaries of thickening of the stratum corneum of the epidermis of a yellowish color, found in areas on the plantar/lateral surfaces of the feet, mainly subject to heavy or frequent load (Fig. below).
A callus is a sharply limited dense area of hyperkeratosis of the epidermis, round in shape, small in size with smooth edges. Predominant localization: zone of pressure of bone processes/protrusions on the underlying soft tissue in the area of the lateral surface of the toes/dorsal surface of the finger joints. In a core callus, in addition to a focus of hyperkeratosis, in the center of the callus there is a translucent hard core, upon pressure on which sharp pain occurs (Fig. below)
Soft callus - occurs mainly against the background of increased humidity between the toes. At the same time, there is a risk of infection of the affected area with bacterial infections.
Subungual hyperkeratosis - occurs quite often, especially against the background of traumatic onychia / onychomycosis . Characteristic is gradual growth from the distal edge/enlargement of the nail plate. In this case, an accumulation of yellow-gray horny mass occurs between the hyponychium and the free edge of the nail (Fig. below).
Hyperkeratosis of the scalp
In most cases, this is seborrheic hyperkeratosis , which is pigmented verrucous formations on the scalp.
At an early stage, the disease manifests itself as yellow-brown, round-oval spots, which gradually turn into dull-colored plaques. The lesions have a clearly defined shape, often multiple, the diameter of which can vary from 1-2 millimeters to 3-5 centimeters.
Treatment
Treatment includes drug therapy and surgical removal. Drug therapy involves the local use of cytostatics or other antitumor drugs selected according to an individual regimen. Treatment may require hospital stay.
Surgical methods for removing keratomas are varied:
- Traditional excision within healthy tissue using a scalpel. Used in cases of suspected cancer.
- Curettage of the hair follicle - the keratoma is scraped out with special instruments with sharp edges.
- Laser removal - using laser radiation, the tumor is evaporated layer by layer. In its place, a crust remains, which disappears after healing, and “young” skin remains in its place.
- Electrocoagulation - the tumor is excised under the influence of high-frequency electric current. It leads to local heating of tissues and their evaporation. At this point, they separate and form a cut. After removal, a wound with a crust remains in place, healing occurs, as after exposure to a laser.
- Radio wave surgery is a non-contact method of removal using radio waves. A modern, effective method with minimal risk of the formation of rough scars.
- Cryodestruction is the effect of liquid nitrogen on the keratoma, which leads to its immediate freezing and necrosis. After a few days it disappears on its own.
Surgical removal is performed on an outpatient basis using local anesthesia. After the procedure, the patient can leave the clinic almost immediately.
Our clinic has all the necessary equipment for keratoma removal, and experienced specialists will offer treatment based on specific clinical features.
Book a consultation around the clock +7+7+78
Prevention
General preventive measures include:
- Compliance with sun exposure and solarium use.
- Strengthening the immune system.
- A rational diet that corresponds to energy costs.
- Prevention of trauma to the skin (wear comfortable, appropriately sized shoes, clothing made from natural fabrics).
- Maintain personal hygiene, correct (according to type) skin care.
- Regular use of medicinal/cosmetic products to moisturize and soften the skin and prevent peeling of keratinized plates.
- Avoid injury to the skin.
- Don't freeze.
- When working with any chemical reagents, avoid contact with skin (use special protective equipment).
- If you are prone to hyperkeratosis, regularly carry out hardware treatment methods and visit a podiatrist.
List of sources
- Bauman L. Cosmetic dermatology. Principles and practice. Per. from English Potekaeva N. N. M.: MEDpress-inform. 2012. 688 p.
- Afanasyev E.N. Mechanically induced hyperkeratoses of the foot // Plastic surgery and cosmetology. 2012. No. 4. pp. 644–661.
- Kholodilova N.A., Monakhov K.N. The use of basic care products in patients with impaired skin barrier // Russian Journal of Skin and Venereal Diseases. 2009. No. 6. pp. 68–69.
- Lomakina E. A. The role of the barrier function of the skin in the pathogenesis of some dermatoses // Modern problems of dermatovenereology, immunology and medical cosmetology. 2009, no. 2. pp. 87–90.
- Rodionov A. N. Dry skin. Dermatocosmetology. Lesions of the facial skin and mucous membranes. Diagnosis, treatment and prevention. SPb: Science and Technology. 2011. 911 p. pp. 63–69.