Russian Ophthalmological Journal, 2017; 1:74-79
E.L. Efimova1, V.V. Brzhesky1, I.E. Panova2, A.S. Aleksandrova1, M.A. Zertsalova1, Ya.M. Poroger3 1 Federal State Budgetary Educational Institution of Higher Education "St. Petersburg State Pediatric Medical University" of the Ministry of Health of Russia 2 St. Petersburg branch of the Federal State Institution MNTK "Eye Microsurgery" named after. Academician S.N. Fedorova Ministry of Health of Russia 3 Medical, Chelyabinsk
Purpose of the work: to evaluate the nature of the effect of the drugs Irifrin 2.5% and Irifrin-BC 2.5% on the main parameters of accommodation, as well as on tear production, stability of the tear film and the epithelium of the ocular surface in patients with computer visual syndrome (CVS) against the background of low myopia and medium degree. Material and methods. We examined 52 people aged from 17 to 34 years (average 22.30 ± 2.72 years) with CLC, divided into two groups. For 4 weeks, patients in group 1 received Irifrin 2.5% daily at night; patients in group 2 received preservative-free Irifrin-BC 2.5%. Before and after the course of therapy, the nature of the effect of these drugs on the main parameters of accommodation, as well as on tear production, the stability of the tear film and the epithelium of the ocular surface was assessed. Results. The effectiveness of the studied drugs 2.5% Irifrin was established against both pathogenetic links of CCD: both accommodation disorders and associated accommodative asthenopia, and secondary dry eye syndrome. All examined patients showed a decrease in the frequency and severity of manifestations of asthenopia, an increase in uncorrected visual acuity, the volume of absolute accommodation, as well as the values of the positive and negative parts of the volume of relative accommodation, which can be associated with the effect of phenylephrine hydrochloride. In addition, there is a decrease in subjective discomfort, the severity of staining of the corneal epithelium with a solution of sodium fluorescein and the conjunctiva with a solution of rose bengal, as well as an increase in the stability of the precorneal tear film, apparently due to the presence of hydroxypropyl methylcellulose in both preparations and the absence of a preservative in the preparation Irifrin-BK 2.5%.
Key words: computer visual syndrome, dry eye syndrome, accommodation, Irifrin, Irifrin-BK.
In recent years, a steady trend has emerged towards a change in the nature of visual work, mainly among schoolchildren and students. This trend is due to the active introduction of modern information technologies and the increasing computerization of the educational process and workplaces. Of course, increasing the intensity of such visual load concerns primarily young people - students and schoolchildren, as well as people whose professional activities involve intense visual work at close range [1–3].
The peculiarities of visual work at a computer naturally cause an excessive load on the accommodative apparatus of the eye, contribute to the development of habitually excessive tension and even spasm of accommodation, visual fatigue and, finally, myopization of the eye. At the same time, the already mentioned groups of people (students, etc.) are most susceptible to these processes.
Another “result” of long-term work at a computer is the development of secondary dry eye syndrome (DES), associated mainly with a decrease in the frequency of blinks during intense visual work at the monitor [1, 4].
The circumstances considered were the reason for identifying the so-called computer visual syndrome (CVS) as an independent nosological form. Currently, this term is widely used in domestic and foreign literature. The main “components” of this syndrome are accommodative (or accommodative-refractive) asthenopia and dry eye syndrome, which together cause a fairly intense symptom complex that reduces the performance and quality of life of people working at a computer [3, 5, 6].
Accordingly, increasing attention has naturally been paid to the study of physiological mechanisms of accommodation and the possibilities of correcting their disturbances in patients with CHD in recent years [1, 5, 7].
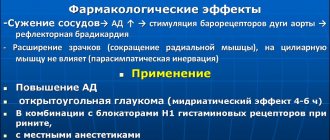
The basis of therapeutic measures for such patients is, on the one hand, the normalization of the ciliary muscle, and on the other, increasing the stability of the precorneal tear film. Of course, the main pathogenetically oriented direction of drug treatment of the pathology in question is the impact on the autonomic innervation of the main portions of the ciliary muscle using instillations of M-anticholinergics (atropine sulfate, cyclopentolate hydrochloride, tropicamide, etc.) and/or α-adrenergic agonists (phenylephrine hydrochloride) [5, 8, 9].
Considering the excessive cycloplegic effect of M-anticholinergics, accompanied by accommodation paresis, which impairs visual work at close range, as well as prolonged mydriasis, preference today is given to instillations of α-adrenergic agonists [8, 9]. Their effect is associated with a direct stimulating effect on the Ivanov radial fibers of the ciliary muscle and, according to the laws of “feedback,” weakening the function of the muscles that are antagonists of the ciliary body (circular and meridional). Among the medicines of the pharmacological group under consideration, the Register of Medicines of Russia includes phenylephrine hydrochloride preparations as eye drops: Irifrin 2.5%, Irifrin-BK 2.5%, Neosinephrine-POS, Vizofrin. Phenylephrine-induced mydriasis is usually short-lived. The clinical effectiveness of Irifrin 2.5% has already been proven in the treatment of children with habitually excessive stress of accommodation, as well as adults with accommodative asthenopia [5, 6, 7, 9].
At the same time, systematic instillation of drugs containing preservatives is naturally accompanied by a violation of the stability of the tear film and, ultimately, the development of secondary dry eye syndrome [10]. Of course, the use of such drugs in the treatment of patients with CCD is fraught with aggravation of the existing xerosis in such patients, which requires modification of phenylephrine hydrochloride preparations, for example, the introduction of polymer bases of tear substitutes into their composition and/or the exclusion of a preservative. These modified eye drops were: Irifrin 2.5% (contains hyproxypropyl methylcellulose as a phenylephrine prolongator) and Irifrin-BC 2.5% (contains the same polymer and also lacks a preservative). However, their effectiveness in the treatment of patients with CVD remains unstudied.
OBJECTIVE OF THE STUDY: To evaluate the nature of the effect of the drugs Irifrin 2.5% and Irifrin-BC 2.5% on the main parameters of accommodation, as well as on tear production, tear film stability and the ocular surface epithelium in patients with CCD.
How to use drops correctly?
The active substance of the drops is phenylephrine. With its vasoconstrictive properties, it is used not only to treat the eyes, but is also found in allergy and cold medications. This is an effective remedy for nasopharyngeal congestion.
Phenylephrine is used by injection for low pressure in the arteries and weak tone of the vascular wall. In ophthalmology it is used as “Irifrin” in two cases - in diagnosis and therapy.
In diagnostic practice, these drops are prescribed to dilate the pupil before surgery and examine the fundus, as well as determine the depth of the bulbus oculi injection and test for angle-closure glaucoma.
The drug "Irifrin" at a concentration of 2.5% and 10% is used as follows.
- To check the fundus oculi, the doctor prescribes a drop of medicine in each eye. Then, after 15-30 minutes, the pupil should dilate enough to conduct an examination. If the procedure lasts more than an hour, the instillation is repeated. If the pupil is not dilated enough, you need to use a stronger 10% composition.
- The test for angle-closure glaucoma will require 2.5% phenylephrine. First, the doctor measures the eye pressure, after which he instills the drug. He then compares the measurement results - before and after the procedure. With a difference of 3-5 mm Hg, pathology occurs.
- The depth of injection of the eyeball is determined using Irifrin 2.5%. After instillation, wait five minutes and check the result. The disappearance of redness indicates its superficial nature. If hyperemia persists, it spreads to deeper layers. Then a differential diagnosis of the identified pathology is carried out.
- Only 10% phenylephrine is suitable for preparation for surgery. It is administered drop by drop into both eyes 30-60 minutes before surgical procedures.
In what cases will Irifrin be effective? These drops are prescribed for the treatment of glaucomocyclic crisis (10% composition), red eye syndrome (2.5%), false myopia and iridocyclitis. Let's consider these pathologies in more detail.
- Glaucomocyclic crisis is manifested by fluctuations in intraocular pressure and signs of cyclitis (hyperemia, blurred vision, night pain, increased lacrimation).
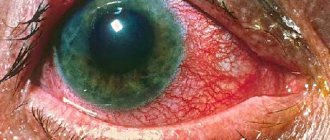
- Red eye syndrome is caused by vasodilation or hemorrhage in the visual organs. It is characteristic of a number of pathologies caused by allergies, viruses and bacteria. Taking into account the symptoms that appear, the specialist diagnoses the disease.
- The spasm of accommodation is accompanied by a prolonged contraction of the focusing muscle. Otherwise, this condition is called false myopia, which is manifested by chronic tension of the musculus ciliaris. This disease, typical of schoolchildren, is considered curable, but over the years it often develops into true myopia.
- Iridocyclitis is an inflammation of the iris or middle choroid. Its symptoms are redness, swelling, changes in the shape of the pupil, eye pain and blurred vision.
For glaucomocyclic crises, Irifrin 10% is usually used, instilled 2-3 times a day. In the case of iridocyclitis, the drug removes fluid formed due to inflammation. In this case, drops of 2.5% and 10% are prescribed in a similar dose with the same frequency. The concentration of the active substance in the solution is determined by an ophthalmologist.
To get rid of false myopia, phenylephrine 2.5% is perfect. It is used daily, a drop in both eyes. The duration of the course is one month. If the problem is not resolved and the spasm is not relieved, increase the dose to 10% and take the drops for two weeks.
Irifrin®
When performing ophthalmoscopy, single instillations of a 2.5% Irifrin® solution are used. As a rule, to create mydriasis, it is enough to introduce 1 drop of 2.5% Irifrin® into the conjunctival sac.
Maximum mydriasis is achieved after 15-30 minutes and persists for 1-3 hours.
If it is necessary to maintain mydriasis for a long time, Irifrin® can be re-instilled after 1 hour.
In adults and children over 12 years of age with insufficient pupil dilation, as well as in patients with a rigid iris (pronounced pigmentation), 10% Irifrin in the same dose can be used for diagnostic pupil dilation.
To relieve spasm of accommodation, a 2.5% solution of Irifrin® in children over 6 years of age and adults is prescribed 1 drop in each eye at night every day for 4 weeks.
In case of persistent spasm of accommodation, it is possible to use a 10% solution of Irifrin® in children over 12 years of age and adults, 1 drop in each eye daily at night for 2 weeks.
For diagnostic procedures, a single instillation of a 2.5% Irifrin® solution is used:
- as a provocative test in patients with a narrow anterior chamber angle profile and suspected angle-closure glaucoma. If the difference between the values of intraocular pressure before instillation of Irifrin® and after dilation of the pupil is from 3 to 5 mm Hg, then the provocative test is considered positive;
- for differential diagnosis of the type of injection of the eyeball: if 5 minutes after instillation there is a narrowing of the vessels of the eyeball, then the injection is classified as superficial; if redness of the eye persists, it is necessary to carefully examine the patient for the presence of iridocyclitis or scleritis, as this indicates an expansion of deeper vessels .
For iridocyclitis, a 2.5% or 10.0% solution of Irifrin® is used to prevent the development and rupture of already formed posterior synechiae; to reduce exudation into the anterior chamber of the eye. For this purpose, 1 drop of the drug is instilled into the conjunctival sac of the affected eye(s) 2-3 times a day.
In glaucomo-cyclic crises, the vasoconstrictor effect of phenylephrine helps to reduce intraocular pressure, which is most pronounced when using a 10% solution of the drug.
To relieve glaucomatous-cyclic crises, 10% Irifrin® is instilled 2-3 times a day.
When preparing patients for surgical interventions, a single instillation of a 10% Irifrin® solution is performed 30-60 minutes before surgery to achieve mydriasis. After opening the membranes of the eyeball, repeated instillation of the drug is not allowed. The 10% solution is not used for irrigation, soaking tampons during surgery and for subconjunctival administration.
"Irifrin" in childhood
For children under 12 years of age, the drug is prescribed for visual impairment if a diagnosis of farsightedness or myopia is made. When a child comes to school, lessons and electives are added to his usual workload. The eyes are under stress and often in the first grades children complain of fatigue and blurred vision.
To avoid this, you need to teach your child to take short breaks when doing homework and watching TV. And at school you can do an exercise to train your eyes, turning your gaze to distant and close objects. This will benefit the baby.
Against the background of increased loads, Irifrin is used as a monthly course, drops at night in both eyes. You can prescribe two drops every other day. After a course of treatment, lacrimation and pain go away, and fatigue decreases.
Usually, the use of the drug prevents vision loss. To avoid switching to contact lenses or glasses, you need to teach children to take care of their eyes and listen to their feelings. As soon as fatigue appears, you need to take a break, do eye exercises or do a neutral activity. These techniques will help you avoid heavy loads.
MATERIAL AND METHODS
The study involved 52 people aged from 17 to 34 years (on average, 22.30 ± 2.72 years) with a verified diagnosis of KZS against the background of mild and moderate myopia (Table 1). All patients received 1–2 drops of Irifrin 2.5% daily (once at night) in both eyes for 4 weeks. At the same time, 24 patients of the 1st group received Irifrin-BC 2.5% (without preservative), and 28 patients of the 2nd group received Irifrin 2.5% (with the preservative benzalkonium chloride).
All patients were examined before the start of therapy and after 4 weeks of treatment using diagnostic methods aimed at studying both accommodative asthenopia and the xerotic component of KZS. The first included visometry, autorefractometry (before and after cycloplegia with three-time instillations of 1% cyclopentolate hydrochloride), proxy and remotometry, determination of the volume of absolute accommodation, positive (reserve) and negative parts of relative accommodation, as well as assessment of the severity of asthenopic complaints. The methods for performing these studies complied with the recommendations of the Expert Council on Accommodation and Refraction (ECAR) [8].
All subjects were also assessed for the severity of subjective discomfort according to the ocular surface disease index (OSDI), the tear meniscus index, the stability of the precorneal tear film (according to M. Norn), the severity of staining of the corneal epithelium with sodium fluorescein solution (according to the Oxford scale), as well as the conjunctiva - 1% rose bengal according to the van Bijsterveld scale [11–16].
As a result of instillations of the studied drugs for 4 weeks, all patients with CVD showed a steady tendency to increase uncorrected visual acuity against the background of a decrease in manifest refraction and the usual accommodation tone (Table 2). However, this trend was not accompanied by statistically significant differences (p > 0.05). However, when comparing the effect of the studied drugs, the dynamics of the decrease in manifest refraction (by 0.19 ± 0.03), as well as the usual accommodation tone (by 0.18 ± 0.04), turned out to be significantly more pronounced against the background of instillations of preservative-free irifrin-BC 2.5 % than instillation of irifrin 2.5% (by 0.06 ± 0.02 D; p < 0.05 and 0.01 ± 0.04 D; p < 0.05, respectively).
Against the background of systematic instillations of the study drugs, there was a tendency for the points of clear vision that are closest to the eye and further away from it, as a result, in all patients with KZS there is a slight, statistically insignificant (p > 0.05) increase in the volume of absolute accommodation (Table 3 ).
At the same time, the values of the positive and negative parts of the volume of relative accommodation also increased. At the same time, the dynamics of the increase in the positive part of the relative accommodation turned out to be significantly more pronounced after instillation of the preservative-free drug Irifrin-BK 2.5% (the difference relative to the effect of the comparison drug is statistically significant, p < 0.05).
In addition, against the background of instillation of the study drugs in patients with CCD, a statistically significant decrease in the severity of asthenopic complaints was revealed (Table 4), moreover, to a greater extent after instillation of the drug Irifrin 2.5%, containing the preservative benzalkonium chloride.
Thus, instillations of both compared drugs of phenylephrine hydrochloride effectively relieve the symptoms of accommodative asthenopia (to a greater extent - Irifrin 2.5%). A decrease in the tone of accommodation, an increase in the volume of absolute accommodation and reserves of relative accommodation are more pronounced when using Irifrin-BC 2.5%.
When analyzing the effects of drugs on the xerotic component of the GLC, the following results were obtained.
Based on the results of assessing the subjective discomfort of patients with CGD, it was found that after treatment, the number of patients with high OSDI values decreased noticeably, and to a significantly greater extent after instillation of Irifrin-BC 2.5% (Table 5 and Fig.).
The severity of staining of the cornea (according to the Oxford scale) and conjunctiva (according to the van Bijsterveld scale) had a positive trend against the background of instillations of both compared drugs (Table 6). Moreover, after instillation of irifrin-BC 2.5%, the decrease in the severity of staining of the corneal epithelium was more significant, and after completion of the course of instillation of irifrin 2.5% - in the nasal and temporal parts of the bulbar conjunctiva.
An increase in the stability of the tear film was also noted in patients of both groups during treatment, but on average this indicator did not reach the age norm [4]. The tear meniscus index, both before and after treatment, turned out to be significantly lower than normal, and while in patients of group 1 there was a tendency for it to slightly increase, in patients of group 2 it even decreased slightly (the changes are statistically insignificant; p > 0.05).
The positive dynamics of the considered parameters of the xerotic process in patients with CCZ against the background of instillations of the compared drugs 2.5% Irifrin may be associated with the presence of hydroxypropyl methylcellulose in their composition, which helps to stabilize the tear film and improve wetting of the ocular surface, on the one hand, and the absence of a preservative in the drug Irifrin-BK 2.5% - on the other.
How does Irifrin work?
When instilling the drug, a slight burning sensation is felt, which disappears after 4-5 seconds. After this, you need to refrain from visual stress for two to three hours. You cannot write, read, work on a computer, watch TV, sew, knit, etc. 15-20 minutes after the procedure, eye accommodation deteriorates, objects become blurred, and bright light causes discomfort. This condition may last for several hours. Doctors recommend instilling Irifrin at night to minimize discomfort.
After using the drops, some patients suffering from hypertension note an increase in blood pressure. This side effect passes quickly and is not a cause for concern. Fans of contact lenses should refrain from wearing them during therapy and use glasses. After a few days you can return to them again. You need to prepare yourself for the fact that after a course of treatment with phenylephrine, your vision will be blurred for another three days. Then everything will get better, and your eyes will see even better.
By constantly using the drug, people note the disappearance of pain and a decrease in eye fatigue. If vision loss is not far from the norm, thanks to Irifrin drops, you can even remove your glasses in the future.
In addition, useful habits - control over eye hygiene, walks in the air and relaxing exercises, alternation of work and rest - will provide the visual organs with normal blood circulation in order to consolidate the therapeutic effect.
References
1. Efimova EL, Brzheskij VV, Aleksandrova AS Characteristics of visual disorders using electronic textbooks and their possible correction. Russian ophthalmological journal. 2015; 2: 27–33 (in Russian). 2. Zemlyanoj DA, L'vov SN Regional characteristic of the state of health of schoolchildren. Pediatr. 2013; 4 (4): 65–9 (in Russian). 3. Blehm C., Vishnu S., Khattak A., Mitra S., Yee RW Computer vision syndrome: a review. Surv Ophthalmol. 2006; 50: 253–62. 4. Brzheskij VV, Egorova GB, Egorov EA The syndrome of “dry eye” and ocular surface disease: clinical picture, diagnosis, treatment. Moscow: GEOTAR-Media; 2016 (in Russian). 5. Markova E.Yu., Matveev AV, Ul'shina LV, Venediktova LV Multipurpose approach to the treatment of accommodation disorders in children. Review. Oftal'mologiya. 2012; 9 (4): 27–30 (in Russian). 6. Proskurina OV, Tarutta EP, Iomdina EN, Strakhov VV, Brzheskj VV A modern classification of asthenopias: clinical forms and stages. Russian ophthalmological journal. 2016; 9 (4): 69–73 (in Russian). 7. Zharov VV, Egorova AV, Kon'kova LV Comprehensive treatment of accommodation disturbances in acquired myopia. Izhevsk: Nauchnaya book, 2008 (in Russian). 8. Proskurina O.V., Golubev S.U., Markova E.Yu. Subjective accommodation methods. In: Katargina LA, ed. Accommodation: gui-dance for practitioners. Moscow: April; 2012: 40–50 (in Russian). 9. Vorontsova TN, Brzheskiy VV, Efimova EL, et al. Effectiveness of pharmacotherapy of chronic overtension of accommodation in children. Rossiyskaya pediatricheskaya oftal'mologiya. 2010; 2: 17–9 (in Russian). 10. Baudouin C., Labbé A., Liang H., et al. Preservatives in eye drops: the good, the bad and the ugly. Prog. Retin. EyeRes. 2010; 29 (4): 312–34. 11. Bron AJ, Evans VE, Smith JA Grading of corneal and conjunctival staining in the context of other dry eye tests. Cornea. 2003; 22 (7): 640–9. 12. Eliason JA, Maurice DM Staining of the conjunctiva and conjunctival tear film. Brit. J. Ophthalmol. 1990; 74 (9): 519–22. 13. Feenstra RP, Tseng SCG Comparison of fluorescein and rose Bengal staining. Ophthalmology. 1992; 99 (4): 605–17. 14. Norn MS Dessication of the precorneal film. I. Corneal wetting time. Acta Ophthalmol. (Copenh.). 1969; 47:865–80. 15. Schiffman RM, Christianson MD, Jacobsen G, Hirsch JD, Reis BL Reliability and validity of the Ocular Surface Disease Index. Arch Ophthalmol. 2000; 118:615–21. 16. Van Bijsterfeld OP Diagnostic tests in sicca syndrome. Arch. Ophthalmol. 1969; 82:10–4.
Address for correspondence: 194100 St. Petersburg, st. Litovskaya, 2, Federal State Budgetary Educational Institution of Higher Education "St. Petersburg State Pediatric Medical University" of the Ministry of Health of Russia [email protected]
How is the drug released?
Irifrin drops are sold in 5 mm bottles. Once opened, they are suitable for use for another three months. The drug is used as prescribed by a doctor and strictly according to the instructions. You need to tilt your head back, open your lower eyelid and from a short distance squeeze a drop of the composition into each eye. In this case, it is not advisable to touch the mucous membrane with the bottle. If the solution gets on this area, adjust the inner edge of the eye so that it does not soak into where it is not needed. And remember about a gentle regime, avoiding visual stress after phenylephrine.
Release form of the drug Irifrin
Irifrin - drops that are available in 5 ml bottles. Once opened, they can be used within a month.
Drops should be instilled based on these recommendations:
- raise your head up;
- pull down the lower eyelid;
- holding the bottle at a distance of 2 cm, squeeze a drop of solution into each eye;
- during instillation, make sure that the tip of the bottle does not touch the mucous membrane;
- when the drop hits the mucous membrane, hold the inner corner of the eye with your hands so that the reflex does not work and the drug has time to be absorbed;
- do not forget about the need to eliminate visual stress after using Irifrin.
Precautionary measures
When a high dose of phenylephrine is administered, it quickly enters the bloodstream and causes unpleasant effects. The risk increases during the post-traumatic period of eye recovery, as well as with a lack of tear fluid.
In addition, doctors recommend careful use of the drug for patients with diabetes and the elderly. Diabetics have a high risk of hypertensive crisis, and in people over 65, the pupil may behave inappropriately and quickly shrink instead of the desired expansion.
Summarize. The active component phenylephrine compresses blood vessels and improves the removal of intraocular fluid. Due to the narrowing, the symptom of red eyes is relieved, and the rapid outflow of fluid brings relief from glaucoma. In addition, phenylephrine has been successfully used for diagnosis and preparation for operations, being an effective pupil dilator.