In recent years, the incidence of human papillomavirus infection has been increasing. According to WHO, every year around the world, about 250,000 women with HPV infection die from cervical cancer. Against this background, the search for effective treatments for this infection becomes extremely important. The problem of its diagnosis and treatment attracts the attention of doctors of various specialties: dermatologists, gynecologists, urologists, oncologists, immunologists, virologists, pathomorphologists. At the moment, most scientists have come to a consensus - the manifestations of the human papillomavirus can be combated using immunomodulators with antiviral activity.
- What are immunomodulators
- List of drugs
- Antiviral for HPV
- Is it possible to use VIFERON Suppositories vaginally?
- Treatment of mucous membranes in men
- Alternative Treatments
What is papillomavirus
The Human Papillomavirus (HPV) is a group of small viruses that contain DNA. These viruses cause pathologies of epithelial tissue. The main method of transmission of infection is unprotected sexual contact. Scientists have discovered more than 200 strains of HPV, of which 29 strains are oncogenic. Dangerous strains cause malignant degeneration of epithelial cells.
The relationship between HPV infection and the development of malignant tumors has been scientifically proven. The papillomavirus is integrated into the human genome, which leads to a failure of the program embedded in the DNA. When epithelial cells divide, the affected gene is transferred to new cells. This is how the virus penetrates into the deep layers of tissue.
The infection is asymptomatic until cells with an altered genome begin to reproduce cancer cells. HPV causes cancer:
- cervix;
- vulva and vagina;
- penis;
- anal canal;
- throat and larynx;
- neck and scalp;
- stomach and esophagus.
The growth of benign tumors is also possible: papillomas, condylomas, anogenital warts. Complications include recurrent respiratory papillomatosis (in adults and children). This disease leads to difficulty breathing and obstruction of the airways.
HPV symptoms
The papilloma virus infects the skin and mucous membranes, causing the proliferation of the epidermis and the appearance of pathological neoplasms:
- papillomas;
- warts;
- condylomas.
They look like small skin growths ranging in size from 1 to 5–8 mm, sometimes there are growths reaching 1–2 cm. Basically, such formations imitate healthy skin in color, but there are elements of dark brown and white shades.
The main places of distribution of papillomas:
- face and neck;
- external genitalia and groin area;
- the inner surface of the elbow and knee bends;
- soles of feet;
- fingers and skin around nails.
On the mucous membranes, elements can appear in the larynx, nasal passages; in girls, sometimes there are formations localized on the cervix.
Types of formations
There are several types of papillomas.
- Vulgar (common) warts. They are the most common type of neoplasm. They have a “leg”, rise noticeably above the surface of healthy skin, reaching a diameter of up to 1–2 cm. Sometimes hair grows from the central part of the wart. Such formations do not bother the child with pain or itching and appear on the arms, back or legs.
- Flat or juvenile papillomas. They look like small pigmented plaques of a fuzzy round shape, do not extend beyond the skin and form in groups. Such elements are characterized by a smooth surface and selectivity: they appear on the face, neck, legs, sometimes hands, but never in the armpits, genitals or skin folds. Occurs in children older than 5–6 years.
- Condylomas or genital papillomas. These elements resemble small papillae. They are pink in color and form in areas with thin skin: in the genital area, on the mucous membranes.
- Plantar warts. They affect the feet, occur under the big toes and visually resemble small round calluses.
Another variant of formations is filamentous warts or acrochords. They are similar to regular ones, but differ in elasticity and more compact sizes up to 5–6 mm. They prefer to appear under the mammary glands, in the groin, armpits, and are found on the neck and face.
The dangers of human papillomavirus
Some of the representatives of these microorganisms are harmless to humans, while others can provoke the growth of cancer cells. HPV is classified into two main types:
- Strains with high oncogenic risk. Such variants of the virus provoke the development of condylomas on the mucous membranes and in the genital area. Under unfavorable circumstances, they can cause an oncogenic mutation.
- Strains with low oncogenic risk. Viruses of this type cause warts, plantar lesions and juvenile papillomas. The risk of cell degeneration is minimal.
The greatest danger lies in girls: studies conducted in the USA have proven that 98% of cases of cervical cancer are associated with this virus. There is also a risk of developing cancer of the vagina, ovaries, anal canal, larynx, pharynx, and in boys, the genitals. Papillomas located in the anus and genital area require special attention.
Classification of viral strains
All HPV strains are divided into cutaneous and mucosotropic. Skin viruses lead to the formation of benign tumors on the skin. Mucosotropic provoke the appearance of neoplasms on the mucous membranes.
Skin strains provoke the development of different types of papillomas:
- Flat. Round nodules with a diameter of up to 10 mm. They do not turn into cancer.
- Pointed. Shaped like a cockscomb. These are pink formations covered with horny cells.
- Thread-like. Round papillomas on a thin stalk. Diameter up to 7 mm.
Mucosotropic strains cause the following diseases:
- Bowenoid papulosis. The appearance of spots and plaques on the genitals.
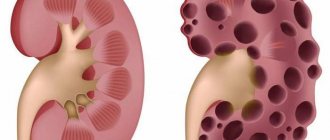
- Dysplasia. Pathological degeneration of cervical tissue.
- Inguinal condylomas. Ball-shaped tumors on a stalk.
If benign tumors appear, you should consult a doctor. A dermatovenerologist will determine the type of papillomavirus and the degree of its danger, and prescribe a treatment regimen for the infection.
Establishing diagnosis
Before treating human papillomavirus in men, the pathology must be confirmed by laboratory tests. After the examination, the doctor may prescribe the following tests:
- urethroscopy;
- urethral smear;
- PCR;
- biopsy of growths.
Since condylomas have an oncological risk, you should not delay your visit to the doctor. Timely treatment allows you to stop the disease and minimize its consequences.
Stages of HPV development
After infection, the latent stage of the disease begins. The virus is already present in the body and is localized in epithelial cells. But so far there are no symptoms that would suggest a human papillomavirus infection. When the virus is dormant, laboratory tests may show a negative result. The latent stage lasts from a couple of weeks to tens of years.
Papillomavirus multiplies in epithelial cells. The number of affected cells increases, and the disease enters the subclinical stage. The first small tissue pathologies appear, not yet visible to the naked eye. The presence of papillomavirus can be determined in a laboratory. The affected epithelium becomes more sensitive to bacterial and chemical influences.
At the clinical stage, formations appear on the skin. To stop the spread of infection and prevent complications, you should consult a doctor in time.
Degrees of oncogenicity of strains
- Non-oncogenic. Provoke the development of benign tumors. The DNA of these viruses is not prone to mutations that cause cancer.
- Low degree of oncogenicity. They can lead to the formation of a cancerous tumor in combination with other risk factors (heredity, weak immunity, bad habits).
- High degree of oncogenicity. Directly provoke the growth of malignant tumors.
Antiviral drugs against HPV
After infecting a cell, the virus can remain free or penetrate the cell’s genome. In either case, the virus alters normal cellular processes. And instead of producing everything necessary for its life, the cell provides mechanisms for the synthesis of viral DNA molecules, which will later be used to create new viral particles. But viruses are not always capable of causing disease. With an adequate immune response, the body gets rid of the virus on its own. If the body's immune response is ineffective, long-term carriage of the virus is possible, which can lead to benign or malignant, depending on the type of virus, manifestations of the disease.
In order to break the chain of endless reproduction of the virus and subsequent development of the disease, the need to treat HPV infection with immunomodulators with antiviral activity has been recognized, because To date, not a single antiviral drug against HPV has been developed that specifically targets the human papillomavirus.
VIFERON for HPV
Are there drugs that fight viruses and at the same time help restore the immune system? Of course, such drugs exist. One of these drugs that helps restore the immune system and has a wide spectrum of antiviral activity is the drug VIFERON.
Recombinant interferon alpha-2b, which is part of this drug, prevents the synthesis of viral DNA and blocks the reproduction of the virus, helps restore the immune system, and also has antiproliferative properties. It is identical to human interferon alpha-2b, but is produced using modern technology without the use of donor blood.
The drug, which is available in the form of suppositories, gel and ointment, was developed as a result of fundamental research in the field of immunology, which has proven that in the presence of antioxidants (vitamins C, E), the antiviral effect of interferon is enhanced.
Method of use and dosage of VIFERON suppositories for HPV
VIFERON Suppositories are produced in the form of bullet-shaped rectal suppositories of white-yellow or yellow color. During the treatment process, the drug suppresses the activity of viruses and increases the effectiveness of the body's own immune response to pathogenic microorganisms.
The drug in the form of suppositories can be used during pregnancy (from the 14th week), as well as during breastfeeding and when treating children.
The recommended dose for adults is VIFERON 500,000 IU, 1 suppository 2 times a day after 12 hours every day for 5-10 days. According to clinical indications, therapy can be continued.
Pregnant women from the second trimester of pregnancy (starting from the 14th week of gestation) are prescribed VIFERON 500,000 IU, 1 suppository 2 times a day every 12 hours daily for 10 days, then for 9 days 3 times with an interval of 3 days (on the fourth day) 1 suppository 2 times a day after 12 hours. Then every 4 weeks until delivery - the drug in a dosage of 150,000 IU, 1 suppository 2 times a day every 12 hours every day for 5 days. If necessary, the drug is prescribed before delivery (from the 38th week of gestation) at a dosage of 500,000 IU, 1 suppository 2 times a day after 12 hours every day for 10 days.
Symptoms of virus infection
At the clinical stage, visible signs of infection appear. The symptom complex depends on the strain of the virus and the location of the affected area. Possible symptoms include:
- the appearance of warts and papillomas on various parts of the body;
- in women: a feeling of discomfort in the vagina, painful sexual intercourse, bleeding from the cervix outside the menstrual cycle;
- copious discharge with an uncharacteristic odor;
- the formation of benign tumors on the genitals, in the anus, in the urethra;
- associated diseases: inflammation of the cervix (cervicitis), bacterial vaginosis, dysplasia of the cervical epithelium.
Indirect symptoms of the disease are chronic fatigue, problems with concentration, physical weakness, and enlarged lymph nodes.
Causes of HPV infection and development of the disease
Infection with papillomavirus can occur at the stage of birth of a child, while he is passing through the birth canal. The virus can be transmitted through contact and household contact in the first years of life. In adults, most cases of infection occur through sexual contact.
Risk factors include:
- Illness of one of the parents or family members.
- Frequent change of sexual partners, unprotected contacts.
- Gynecological manipulations: installation of a spiral, abortion.
- Long-term use of hormonal contraceptive pills.
- Hormonal imbalance caused by other reasons.
- Pregnancy and the postpartum period in women.
- Various diseases of the reproductive system.
- Hypothermia of the pelvic organs.
- Smoking, drinking alcohol and drugs.
- Chronic stress, diseases of the nervous system.
Infection with a virus does not always lead to the development of disease. Human papillomavirus infection can be suppressed by a strong human immune system. Therefore, the HPV treatment regimen sometimes includes taking immunomodulator pills.
Diagnosis of infection at the Private Practice clinic
Several tests are required to make a diagnosis of HPV. Analyzes in our modern laboratory are done quickly using highly accurate methods. You will find out the result on the day of the smear test.
Polymerase chain reaction
PCR determines the presence or absence of viral DNA in a biomaterial. For analysis, a smear is taken from the mucous membranes and directly from the neoplasms themselves, papillomas, condylomas and erosions. The location of the smear depends on the location of the skin tumors. PCR identifies the types of viral strains in the body. The cost of analysis starts from 300 rubles.
Cytological analysis. PAP diagnostics
Papanicolaou test - examination of a smear under a microscope. A smear is taken from the affected area and applied in a thin layer to laboratory glass. The preparation is stained to improve the visibility of cells.
Examining the drug under a microscope, the diagnostician pays attention to the size and shape of the cells. Cytological examination reveals the presence of atypical cells, dysplasia, and malignant mutations. The detected virus is assigned a Pap class.
Colposcopy in women
Examination and examination of the cervix. The procedure is performed in a gynecological chair. For diagnosis, the cervix is stained with safe Lugol's solution. If it is affected by a virus, the area with infected cells is different in color. After a positive colposcopy, a biopsy is performed. It is necessary to clarify the degree of oncogenicity of the virus. A survey colposcopy in our clinic is included in the cost of an appointment with a gynecologist.
Biopsy
A biopsy is used to accurately determine the cellular composition of tissue. This is a reliable method for diagnosing cancer. A biopsy is prescribed when the doctor suspects that malignant degeneration of epithelial tissue has already begun. The cost of diagnostics starts from 1500 rubles.
HPV: can it be treated or not?
It happens that papillomavirus is cleared from the body within two years after infection. But this is typical mainly for children and young people. However, since the prevalence of the virus is high, there is a risk of re-infection (relapse). Immunity after an illness is not formed for life, but for 1–3 years. It is this fact that underlies the statement that HPV cannot be cured.
In most cases, in adults, the papillomavirus does not leave the body on its own, but is integrated into the genome, provoking the development of tumors, including cancer. We advise you not to rely on luck, but to start treatment at the first symptoms of the disease. Human papillomavirus infection is successfully treated with modern medicine. New growths on the skin are removed using destructive methods.
Effective treatment is possible only according to the regimen proposed by the attending physician. When prescribing therapy, the dermatovenerologist takes into account the HPV strain, the degree of oncogenicity, and the patient’s immune system. Self-selection of medications will most likely not give the desired result. After therapy, you need to get tested for HPV every 2 years to avoid relapse of the disease.
Immunomodulators for HPV: list of drugs
Drugs that are synthetic complex purine derivatives
This group of immunomodulators, used in the treatment of manifestations of the human papillomavirus, have immunostimulating activity and a nonspecific antiviral effect. They restore the activity of lymphocytes, which are the main cells of the immune system. It has been clinically proven that low lymphocyte activity is a predisposing factor to the pronounced development of clinical manifestations of HPV. Also, this type of drug increases the functioning of natural killer cells and the so-called T-helpers - T-lymphocytes, the main function of which is to coordinate the immune response.
Some of the drugs in this group have an extensive list of side effects, including problems with the gastrointestinal tract, liver and biliary tract. Adverse reactions such as headache, drowsiness, insomnia, itching and joint pain are also possible. Contraindications include children under 3 years of age, pregnancy, kidney disease and hypersensitivity to the components of the drug.
Preparations with the active ingredient glucosaminylmuramyl dipeptide (GMDP)
GMDP is a fragment of the shell of pathogenic bacteria that cause infectious and inflammatory diseases of various organs and systems. When this fragment enters the body, the immune system perceives it as a foreign pathogenic agent and immediately begins producing antibodies. Thanks to this, there is a general activation of the entire immune system, which promotes recovery or reduces the frequency of relapses of viral infections, including HPV.
Side effects include an increase in body temperature to subfebrile and febrile levels, and diarrhea is also possible. Drugs in this group are contraindicated for metabolic disorders and for women during pregnancy and breastfeeding.
Preparations containing natural plant materials as active ingredients
This group of drugs was created based on the discovery of Nobel Prize laureate N.N. Semenov about the powerful immunostimulating properties of biologically active substances contained in plant cells. Plant extracts and auxiliary components strengthen the nonspecific part of the immune system, which increases the human body’s resistance to various viral and some bacterial infections. The immunomodulatory effect activates leukocytes, which is especially important in the fight against chronic and protracted inflammatory processes.
Allergic reactions are possible when using these drugs. Contraindications for use include diseases of the excretory system, pregnancy, lactation and children under 18 years of age.
Drug treatment of HPV at the Private Practice clinic
To treat human papillomavirus infection, doctors at our Private Practice clinic prescribe complex therapy. Medications reduce the concentration of the virus in tissues and strengthen the body’s immunity. Medicines eliminate the symptoms of the disease and improve a person’s well-being.
Attention! Self-medication can be dangerous to your health. Drugs for the treatment of HPV in women and men should be selected by a dermatovenerologist.
Antiviral tablets
Lavomax has a combined effect. This medicine suppresses the virus, stops its reproduction and stimulates the immune system. Take one tablet containing 125 grams of active ingredient, once a day, every other day. Do not reduce the interval between taking the medicine so as not to harm your health. The treatment course includes twenty tablets.
Isoprinosine is a universal drug. Prescribed to combat tumors on the skin, larynx, and genitals. This medicine suppresses the activity of the virus and stimulates the development of immunity. The dosage regimen is prescribed individually. The treatment regimen may include taking six to eight tablets per day. The course lasts from five days to several months.
Lykopid strengthens the body's defense against infections. Activates hereditary immunity, helps form an acquired immune response. Take one tablet (10 mg) once a day (half an hour before meals). The treatment course lasts from ten days.
Gepon is an immunomodulator. The drug activates the body's immune responses. Has anti-inflammatory and antiviral effect. Take one tablet (10 mg) per day. The duration of treatment depends on the individual response to the drug.
Unfortunately, all of the listed tablet drugs have very low effectiveness for the treatment of HPV. We have observed in many cases where patients undergoing treatment for human papillomavirus infection only with tablets experienced an increase in papillomas and condylomas while taking these medications.
Vaginal suppositories
Suppositories (candles) are prescribed by gynecologists at our clinic for the treatment of the vagina and cervix. Medicines for the treatment of human papillomavirus infection in women:
- Genferon. Double action drug. It contains interferon, which suppresses the development of the virus. Candles eliminate the unpleasant symptoms of the disease: pain and burning. For treatment, administer two suppositories per day: morning and evening. The treatment course lasts ten days;
- Viferon. Combined candles. Inhibits the reproduction of the virus, eliminates the symptoms of the disease, stimulates the immune system. Use suppositories twice a day, morning and evening, for five days.
Intramuscular injections
To treat papillomavirus, a dermatovenerologist may prescribe intramuscular injections. A popular injection drug is Ferrovir. 5 milliliters of medication should be administered twice a day. Duration of treatment course: two weeks.
Cycloferon is used for both intramuscular and intravenous administration using a special technique. Enhances the production of interferon in virus-affected and immune cells, which prevents its active reproduction.
Intravenous injections
The most effective drugs are administered intravenously in drip courses. Typically, polyoxidonium, panavir, and cycloferon are used, which suppress viral replication by activating the appropriate antiviral defense mechanisms.
The courses of treatment are long and combine well with general intravenous ozone therapy.
Cytostatic drugs
To combat skin defects, cytostatics and coagulants are used. These are topical medications. They do not suppress the development of the virus, but eliminate the external symptoms of infection. They are prescribed as an element of complex therapy. Medicinal substances are contained in a solution that is applied to the skin.
Podophyllin. It removes genital warts well. Burns through the cells of skin formations, causing necrosis. The solution is applied to the condyloma twice a day, with an interval of 12 hours. The duration of the treatment course is three days. The drug should not come into contact with healthy skin.
Solcoderm. Used to remove benign tumors. This is a powerful drug. We do not recommend using it without medical supervision. To remove papilloma, warts or condyloma, it is enough to apply it once. The skin lesion will become necrotic and darken, and then fall off.
Antibiotics
HPV is not treated with antibiotics. They act on bacteria, not viruses. Antibiotics are prescribed if diagnostic results reveal concomitant diseases (for example, bacterial vaginosis).
Local antiviral herbal remedies
Ammonium glycyrrhizinate
The active component of the drug, activated glycyrrhizic acid, is obtained from licorice root. It has a complex immunostimulating, antiviral, anti-inflammatory, antipruritic effect. Glycyrrhizic acid interrupts the replication of a number of DNA and RNA viruses, including herpes simplex virus, human papillomavirus, and cytomegalovirus [5].
Indicated as a drug for the treatment of human papillomavirus infection and herpes simplex virus, including infection with oncogenic viruses. Available in the form of a spray, which is sprayed onto the mucous membranes and affected areas of the skin.
Vacation: without prescription.
+
It has a wide range of indications, including the prevention and treatment of vulvovaginal candidiasis, discomfort in the genital area. Can be used during pregnancy and breastfeeding; well tolerated.
Podophyllotoxin
The active component of podophyllin, a derivative of plant extracts isolated from the rhizomes with roots of Podophyllum thyroid - a plant of the barberry family. It has pronounced antitumor and antiviral properties and has a cytotoxic effect. When used externally, it cauterizes and mummifies condylomas. It is used as a drug for local treatment of human papillomavirus. Available in the form of a solution for the treatment of genital warts [8].
Release: by prescription.
+
Proven effect. According to research, a 0.5% solution of podophyllotoxin reduces the number of anogenital warts from 6.3 to 1.1, destroying about 70% of formations [8].
!
Care must be taken when using - contact with healthy skin can lead to ulceration. Local reactions during use, allergic reactions. The physician, when dispensing this antiviral drug for papillomas and condylomas, must draw the client’s attention to this feature and remind him that the drug should be stored out of the reach of children.
Tetrahydroxyglucopyranosylxanthene
Russian drug. The active component is isolated from the Alpine kopek plant or the yellow kopek plant.
According to the instructions, it has antiviral activity against HSV-1 and HSV-2, as well as cytomegalovirus and some other DNA-containing viruses. In addition, the drug presumably activates cellular and humoral immunity, inhibits the growth of a number of bacteria and pathogenic protozoa, including Trichomonas, and also has a moderate anti-inflammatory effect. Used in the form of an ointment as part of the combined treatment of acute and recurrent forms of herpes, including genital herpes [5].
Vacation: without prescription.
+
Favorable safety profile, the ability to be used as part of complex treatment.
Polysaccharides of Solanum tuberosum shoots
A Russian prescription drug, the active component is obtained from the shoots of tuberous nightshade. According to the instructions, it exhibits an antiviral effect against HSV-1 and HSV-2, promotes the induction of interferons and increases the immune response [5]. It should be noted that the pharmacokinetic properties of the drug have not been studied. Vaginal suppositories are used in complex therapy of genital herpes.
Vacation: without prescription.
+
High safety profile. Side effects are rare.
Desmodium canada herb extract
An antiviral drug for herpes of plant origin, created from a dry extract of the herb Desmodium canadensis. According to the instructions, it exhibits antiviral activity against herpes viruses and stimulates the production of interferon [5]. The ointment is indicated for use in acute and recurrent forms of herpes, including urogenital.
Vacation: without prescription.
+
High safety profile - no side effects identified.
Hyporamine extract
Russian development based on sea buckthorn leaf extract. According to the instructions, it is active against herpes simplex viruses, cytomegaloviruses and some others [5]. An ointment containing hyporamin extract is indicated for the treatment and prevention of episodes of herpes, including genital herpes.
Vacation: without prescription.
+
High safety profile; Possibility of use during pregnancy and lactation (after consultation with a doctor).
Destructive and surgical treatment methods
To quickly eliminate warts, condylomas, and papillomas, destructive techniques are used. Unlike conservative treatment, they do not allow you to wait until the tumor necrotizes and falls off on its own. In the office of a dermatovenerologist, skin defects can be eliminated in one visit. Removal of pathologies in hard-to-reach places is carried out only by surgical methods.
Electrocoagulation
During electrocoagulation, defects are removed with an electric knife. It generates electrical waves that cut off skin growths and destroy pathological tissues. Electric waves cauterize small vessels, there is no bleeding after surgery. Removing one defect takes from a few seconds to five minutes. Removal of small papillomas on the skin with an amount of more than 20 pcs. costs 200 rubles. for 1 unit. Large tumors are removed under local anesthesia at a cost of 1000–1500 rubles.
Cryodestruction
Liquid nitrogen is used for cryodestruction. The temperature of the substance is -190 degrees. When liquid nitrogen gets into the defects, necrosis occurs. Extremely low temperatures cause cell destruction, blockage of oxygen, and blockage of blood vessels. A thermal burn is formed and the tissues die. The operation is carried out under the supervision of an experienced doctor, who ensures that the substance does not come into contact with healthy skin. The effect of the procedure does not occur immediately, but after 5–10 days, when the necrotic papilloma tissue is completely rejected. The cost of cryodestruction usually ranges from 500 to 1500 rubles. per element.
Radio wave surgery
The operation uses a device that emits radio waves at high frequencies. Radio waves destroy skin defects using thermal energy. The device is operated by an experienced doctor. It directs radio waves, focusing the flow on the growth, avoiding touching healthy skin. This is the most effective and cost effective method for removing papillomavirus tumors on the skin and mucous membranes. The cost of the procedure is from 300 rubles. for the destruction of multiple small papillomas, up to 1500 -2000 rubles, for the removal of large tumors.
Laser defect removal
A directed beam of laser beams removes skin defects. Under the influence of the laser, the cells evaporate. A protective crust is formed at the site of the removed growth. Destruction of the defect takes from 5 seconds to two minutes. Healthy skin forms under the horny crust. About a week after the intervention, the crust disappears. The cost of laser removal of large papillomas is from 1000 rubles.
Removal of affected tissue
Invasive intervention techniques are used for deep tissue damage, when the process of malignant degeneration has already begun. Knife conization is used to remove pathological areas of the epithelium. When HPV is advanced and oncology begins to develop, they resort to removing the cervix with a scalpel.
Our doctors use an integrated approach to the treatment of HPV, which provides close to 100% effect from the therapy. It includes a combination of injectable, tableted immune, antiviral and topical medications. Removal of tumors is carried out using the chosen method against the background of drug treatment, which allows you to completely get rid of papillomas and condylomas and other manifestations of HPV, and prevent recurrence of the infection.
Briefly about the main thing:
If you decide to get rid of papillomas, there are 2 ways: The first is to remove papillomas in the clinic, preferably from an oncologist. The advantages of this method are obvious - maximum efficiency and safety. The second method is removal at home using drugs that can be bought in pharmacies. The advantage of this method is its low cost, however, for safe removal, I recommend first consulting with an oncologist. If treatment of papillomas with none of the above methods is effective, it is worth checking your immunity. To do this, it is better to consult an immunologist.
Have you decided to part with your papillomas? This can be done at addresses in St. Petersburg (Asafieva 7/1)
Treatment of HPV with folk remedies
Is it possible to cure HPV only with folk remedies? From the point of view of official medicine, it is impossible. Traditional recipes help strengthen the immune system and eliminate external symptoms of the disease. But they do not suppress the development of the virus, like medications.
Recipes for clear skin
Do not apply active ingredients with bare hands. Use gloves and cotton swabs to treat the affected area.
- Lubricate the wart, papilloma, condyloma with 70% vinegar essence. Repeat the treatment two to three times a day. The tumor will become covered with a white crust and then fall off. Often there are complications in the form of deep non-healing ulcers.
- Treat skin defects with iodine solution. Apply iodine twice daily for two weeks. During this time, the defect should dry out and fall off.
- Grind the celandine and mix it with medical alcohol in a 2:1 ratio or buy a ready-made tincture at the pharmacy. Treat the defect three times a day. Celandine does not act immediately. The course of treatment can last up to three weeks.
- Essential oils of sea buckthorn, thuja, and tea tree help cleanse the skin. They soften tumor cells, which promotes its death. Mix one of the listed oils with castor oil 1:1. Treat defects twice a day. The duration of the course is not limited.
Using folk remedies only on the recommendation and under the supervision of a doctor, wait until the defect is completely necrotic. Do not tear off the tumor until it falls off on its own, otherwise you may provoke bleeding or introduce an infection into the wound. The active substance should burn the wart, papilloma, condyloma to the roots. Otherwise, the tumor may grow again in the same place.
Recipes to boost your immune system
Prepare or buy herbs: horsetail, nettle, plantain and lemon balm. If you harvest your own herbs, dry them and grind them into powder. For the recipe you will need a tablespoon of each herb. Mix the herbs in a saucepan and pour 200 ml of boiling water (about three glasses) over them. The decoction should be infused for three hours. Take the decoction for a week, 50 ml per day.
For the second recipe you will need two tablespoons of spruce or pine needles. Add 100 ml of water (about a glass and a quarter). Bring the mixture to a boil. When the water boils, reduce the heat. Keep the broth on low heat for half an hour. It needs to be insisted for the same amount of time. Drink two tablespoons of decoction three times a day. You should drink it for one to two weeks.
Attention! We do not recommend treatment with traditional methods without first consulting a doctor in order to avoid possible undesirable consequences.
Therapy
When figuring out how to cure the papilloma virus in men, it is worth understanding that it will not be possible to completely get rid of the pathogen. Modern means can only stop the development of the process and remove the consequences of the pathogen’s activity.
There are general and local therapy. General assumes the following appointments:
- antiviral drugs;
- immunomodulators.
Local treatment of human papillomavirus in men involves removing growths. This can be done using the following methods:
- cryodestruction;
- electrocoagulation;
- cauterization with chemicals;
- thermal exposure by laser;
- electrosurgical method.
The procedure to remove growths is either painless or performed under local anesthesia. Timely therapy can significantly reduce the severity of symptoms and prevent HPV damage to large areas.
HPV prevention methods
For the development of the disease, it is enough for several small viruses to enter the body. Prevention methods will help prevent infection or recurrence of the disease:
- Use barrier contraception during sexual intercourse.
- Avoid public swimming pools, baths, saunas.
- Strengthen the body's immune system.
- Avoid stress and nervous overload.
- Dress warmly and avoid hypothermia.
We advise women to undergo a gynecological examination and tests for infections at least once a year. This will help maintain the health of the reproductive system.
Possible complications
Human papillomavirus infection can cause severe or mild complications. The most severe possible complication is the development of malignant tumors. Oncogenic strains of the virus cause cellular mutations that contribute to the transformation of benign tumors into malignant ones.
Cervical dysplasia precedes the development of cancer. Papillomas on the larynx grow and cause attacks of suffocation. HPV increases the likelihood of cancer of the stomach, intestines, and respiratory system.
Benign formations on the skin seem less dangerous than cancer. But we do not recommend delaying their treatment. Condylomas, papillomas and warts can accidentally come off. In their place, a bleeding wound forms, into which pathogenic microorganisms easily penetrate. Large defects can leave unsightly scars if the removal is not carried out in the office of a dermatovenerologist.
Intraurethral condylomas may be accompanied by inflammation and bleeding from the urethra.
When to see a doctor
There is no universal way to get rid of the papilloma virus in the body. The treatment regimen is prescribed by a dermatovenerologist after reviewing the test results and the patient’s medical history. When should you visit a dermatovenerologist:
- Since childhood, your skin has had many warts, papillomas, and condylomas;
- skin defects have begun to appear en masse recently;
- you notice strange discharge from the genitals;
- you began to feel itching and burning in the perineum;
- unpleasant sensations appeared during sexual intercourse;
- you started self-treatment for HPV, but did not get results;
- you are planning to have a child (then both partners should be checked);
- you have not been tested for sexually transmitted infections for more than a year.
We recommend getting tested regularly for HPV, even if you have no symptoms and are not planning a pregnancy. Sometimes the latent stage of the disease can last for years. The virus may be present in the body, but not manifest itself in any way. Early diagnosis will help avoid the development of complications.
Is it possible to use VIFERON Suppositories for HPV vaginally?
Antiviral suppositories VIFERON are produced only for rectal use. Vaginal use is not provided for in the instructions for the medicine. The use of the drug in complex therapy is aimed at increasing the level of immune defense of the body as a whole. Therefore, inserting suppositories directly into the site of infection is not required.
There are many blood vessels in the rectum that absorb the medicine directly injected into the rectal cavity. Blood from the rectum, bypassing the liver, directly enters the systemic circulation. This ensures the systemic effect of the drug. Moreover, the liver does not undergo additional stress, which is an undeniable advantage of drugs with rectal administration.
Advantages of the Private Practice Clinic
- Certification in all areas of work.
- The consultation is conducted by experienced dermatovenerologists and gynecologists.
- The latest methods of treating diseases.
- Possibility of removing papillomas and condylomas using all currently known modern methods without pain and serious scars.
- Results of express tests on the day of treatment.
- Individual approach to each patient.
- Polite and friendly staff.
- You can undergo diagnosis and treatment anonymously.
- Convenient location of the clinic in the center of Moscow and Southern Administrative District.
- Parking for visitors to the medical center.