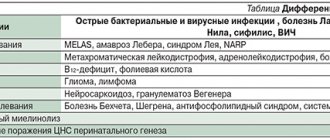
Multiple sclerosis is a disease that affects the spinal cord and brain, causing problems with muscle control, vision problems, body balance problems, and sensory problems (numbness). In multiple sclerosis, the nervous system is damaged by the body's own immune system. That is, in fact, multiple sclerosis is considered an autoimmune disease. Autoimmune diseases involve aggression of the immune system against its own organs and tissues (examples of autoimmune diseases are systemic lupus erythematosus and rheumatoid arthritis).
The central nervous system consists of nerves that act as the body's information system. Each nerve is covered with a fatty substance called myelin, which insulates the nerves and helps in transmitting electrical impulses along the nerves, carrying information from the brain to the organs. These nerve impulses control muscle movements such as walking and talking.
Multiple sclerosis gets its name from the increase in scar tissue in the brain or spinal cord. Scar tissue, or plaques, form when the protective and insulating myelin that covers nerves is broken down, a process called demyelination. Without myelin, electrical signals transmitted throughout the spinal cord and brain are interrupted or not transmitted. The brain then becomes unable to send and receive information. It is this breakdown in communication that causes MS symptoms.
Although nerves can reproduce myelin, the process is slow and does not keep pace with the damage caused by demyelination. Symptoms and their severity depend on the location of the scar tissue and the degree of demyelination.
In the United States, multiple sclerosis is one of the most common causes of neurological disability in middle-aged people.
MS is two to three times more common in women than in men and is extremely rare before puberty. Most often, multiple sclerosis occurs between the ages of 20 and 40; as a rule, it does not occur at older ages.
Causes
The causes of multiple sclerosis are still unclear, but evidence has emerged that genetics, environment and even viruses may play a role.
Epidemiological data have revealed several interesting trends in the disease of multiple sclerosis: different prevalence and certain ethnic dependence of the disease of multiple sclerosis have been noted. The disease is more common in northern countries and in people of the white race.
Research shows that MS is more common in certain parts of the world, but if you move from an area with a higher risk to an area with a lower risk, the risks are reduced if the move is before puberty.
In addition, MS is a disease of temperate climates. In both hemispheres, its prevalence increases with distance from the equator.
There have also been “epidemics” of MS in history, for example, a group of people living off the coast of Denmark fell ill with multiple sclerosis after World War II, perhaps due to some environmental problems.
Multiple sclerosis researchers believe that there is a specific genetic basis for the disease multiple sclerosis.
Researchers believe there is more than one gene that predisposes people to the risk of developing multiple sclerosis. In addition, scientists believe that a person is born with a genetic readiness to develop this disease under certain environmental triggers. With the development of gene analysis, it may be possible to obtain more information about the role of genes.
Certain studies do not exclude the role of viruses, especially Epstein-Bar, herpes zoster, even hepatitis vaccines. But obvious evidence of the involvement of viruses in the development of multiple sclerosis has not yet been obtained. Provoking factors for the development of multiple sclerosis also include sex hormones (estrogen and testosterone), which, when released in excess, can suppress the immune system, especially for estrogen (women get sick 2-3 times more often than men). But their role is also not obvious. Currently, scientists have concluded that the disease occurs due to a number of factors.
Symptoms and signs of multiple sclerosis
The most common signs of multiple sclerosis are impaired coordination of movements, muscle weakness, problems with urination, sensory disturbances, fatigue, dizziness, vision problems, decreased intellectual abilities, tingling and numbness of the limbs, impaired speech function, sexual dysfunction, problems with swallowing.
- Let's look at the manifestation of these symptoms in more detail.
Impaired coordination of movements
The most common coordination disorders in multiple sclerosis are:
- disturbances in the coordination of movements in different muscles - ataxia,
- trembling of limbs,
- loss of balance,
- gait disturbances: it becomes unsteady and clumsy, and instability appears when walking.
Coordination disorders can be a response to sensitive genesis (in this case, the cause is impaired muscle-joint sensitivity), direct vestibular disorders, or malfunctions at the cerebellar level.
Muscle weakness
First of all, muscle weakness manifests itself through reduced motor activity.
- Tendon reflexes in the knees and calves are disrupted.
- The strength of one half of the body decreases (hemiparesis).
- Muscle tone decreases. Natural muscle tension begins to be insufficient to ensure movement.
- Painful spasms appear when straightening the legs. As the disease progresses, they are painful even when the person is in a lying position.
Often, impaired motor activity leads/is adjacent to osteoporosis. – a skeletal disease that is associated with metabolic disorders.
Sensitivity disorders
Another characteristic symptom at an early stage is paresthesia - sensitivity disorder.
- Most often, the toes and cheeks begin to go numb, and the sensitivity of the legs decreases - from the ankles to the ribs.
- I am worried about “crawling goosebumps” and tingling sensations in the body.
- There may be false sensations of electric shock in the back and arms. This happens especially often when bending the head or making sharp turns.
- A number of patients develop pronounced unilateral sensory disturbances in the facial area.
It is with a sensitivity disorder of 30-50% that multiple sclerosis begins in people at a young age.
Vision problems
Vision problems in multiple sclerosis are associated with damage to the optic nerve.
Retrobulbar or optic neuritis occurs in 60% of people suffering from multiple sclerosis. Its characteristic symptoms are:
- Decreased visual acuity. In this case, the problem may appear in one or both eyes.
- Painful sensations when moving the eyeballs.
- The perception and distinction of colors becomes difficult; especially many difficulties arise in the perception of green and red colors.
- Narrowing field of view. A person is forced to choose a convenient angle for himself.
In some patients, blindness progresses. Visual disturbances are also accompanied by headaches.
Urinary disorders
The nature of the disorders depends on the damage to the area of the brain.
- With lesions in the area above the pons of the brain, urinary control decreases and urinary incontinence occurs:
- If the lesions affect the thoracic and cervical parts of the spinal cord, the ability to relax is lost, an intermittent sluggish stream becomes characteristic of urination, and some people experience a feeling of incomplete emptying.
- If the sacral region is affected, problems with the urge to urinate and chronic urinary retention begin. In this case, infection often develops quickly. Problems associated with leukocyturia and microflora come to the fore.
The early stages of multiple sclerosis are more characterized by delay, frequency, urgency (uncontrollable leakage), and the later stages are more characterized by incontinence and loss of urinary control.
Sexual disorders
- Characteristic of most patients with urinary disorders.
- The problem is aggravated by several factors: both damage to a number of parts of the central nervous system and fatigue characteristic of the disease.
- In men, sexual dysfunction is associated with problems with ejaculation and erection. Many men experience decreased libido.
- In women, problems manifest themselves in both pain during sexual intercourse and the inability to achieve orgasm.
Rare symptoms of multiple sclerosis
There is also a group of symptoms that occurs only in some patients suffering from multiple sclerosis. But these symptoms are also very serious:
- Short-term semi-fainting - paroxysmal state (for a few seconds). Consciousness is not completely lost, but attacks can be repeated several times (sometimes dozens) per day. The problem, to a lesser or greater extent, is relevant for 5-10% of patients with multiple sclerosis.
- Epileptic seizures. Occurs in approximately 2% of patients.
- Acute psychoses (more often in women).
- Sudden onset of back pain with a feeling of being compressed by a tight belt (transverse myelitis).
- Respiratory disorders. Characteristic of patients with damaged brain stem.
- Sweating disorder.
- Hypothermia – a decrease in basal temperature (below 35 ° C).
Symptoms
Almost any neurological syndrome manifests itself in MS. It all depends on which area is affected by the antibodies.
Most often observed:
- decreased visual acuity, blurred vision, double vision;
- weakness in the arms and/or legs;
- increased muscle tone (spasticity) in the arms and/or legs;
- numbness of the skin of the face/arms/legs;
- unsteadiness and instability when walking;
- trembling of hands and feet;
- urinary disturbance.
Multiple sclerosis has nothing to do with memory loss; cognitive impairment is not typical for it (the term describes pathomorphological changes).
Causes
Multiple sclerosis is a multifactorial disease. The causes and prerequisites are a combination of unfavorable external and internal factors.
- Frequent infections - bacterial and viral in nature.
- Increased radioactive background.
- Suffered injuries. Often the disease is discovered after an accident.
- Stressful situations.
- Genetic predisposition (genes that are responsible for controlling the immune response are especially important).
Also, many doctors point to the autoimmune nature of multiple sclerosis. The immune system begins to recognize nerve cells as foreign.
Routes of infection
Although the disease can be triggered by a viral or bacterial infection, it is impossible to directly become infected with multiple sclerosis from person to person.
An infection can only push the immune system to aggressively produce antibodies, and the body to replace organ parenchyma with dense connective tissue, forming pathological foci in the brain and spinal cord.
But since viruses and bacteria are “provocateurs”, people predisposed to the disease (for example, close relatives suffer from multiple sclerosis) are recommended to pay special attention to the prevention of colds and get vaccinated against infectious diseases in a timely manner.
Prevention
Since at the moment science has difficulty determining the exact causes of MS, there are no specific preventive measures. But one thing is for sure - maintaining a healthy lifestyle is an excellent preventive measure for most diseases. Namely:
- play sports (it’s enough to run in the morning or do exercises);
- avoid stress;
- give up bad habits;
- normalize nutrition and weight;
- sleep at least 8 hours a day;
- Be periodically examined by a neurologist.
Such simple rules are suitable for both healthy people and those already suffering from multiple sclerosis: it is important for them not to aggravate the course of the disease.
Risk factors
Pay attention to the statistics:
- Women suffer from multiple sclerosis more often than men.
- The majority of patients diagnosed with the disease are people aged 18 to 50 years. But you can get multiple sclerosis in early childhood (up to 10% of diagnosed cases occur in childhood) and in adulthood.
- Those who have problems with the endocrine system are at high risk of developing multiple sclerosis. The presence of diabetes mellitus and thyroid pathology is especially dangerous.
- Chronic inflammatory diseases significantly increase the risk.
Excess body weight is also a risk factor. Especially if an overweight person has problems with lipids: in particular, when the content of low-density cholesterol in the blood is increased.
There is a relationship between the disease and a person’s geographic residence:
- Most people with multiple sclerosis live in temperate climates. Here, 1 case is recorded per 300-1000 people.
- In the tropics, one person with multiple sclerosis occurs in a population of 5,000–20,000 people
- Among people who were born and live near the equator, there is the smallest number of cases
Smoking also significantly increases the likelihood of developing multiple sclerosis. This fact has been proven by Norwegian and American scientists. The fact is that smoking saturates the body with neurotoxins.
Caring for sick women
Patients with MS need constant care, so if the patient has no relatives, he is often transferred to inpatient treatment. A patient with MS needs the following help:
- ensuring physical mobility to prevent muscle atrophy;
- walking assistance;
- control of the frequency of trips to the toilet;
- creating a positive emotional mood;
- light massage of the limbs (as recommended by a doctor), etc.
Make an appointment
What do the patient's relatives need to know?
It is worth remembering that MS is a disease that currently cannot be completely cured. But, at the same time, you should not treat a patient with multiple sclerosis as a disabled person. For a long time, people with this diagnosis are able to take care of themselves and even work, so do not interfere with this. Create an atmosphere of care and love around you: exercise with the patient, prepare food for him that corresponds to the diet prescribed by the doctor, and simply be there to help in moments of exacerbation of the disease.
Currently, patients with MS can live a full life up to 72-75 years, but only if treated and followed the doctor’s recommendations. How you can support the patient:
- Never say that recovery is possible; there is no need for false promises. Only stabilization and reduction of symptoms is possible.
- Encourage interest in treatment and rehabilitation. The Yusupov Hospital has a rehabilitation center for patients with MS. With the help of modern equipment and the use of new techniques, patients begin to feel more confident.
- Offer feasible tasks. This way the patient will feel needed and important.
- Do not scold the patient for clumsiness or inattention. These are symptoms of the disease. Man cannot control them in any way.
- Encourage the person to be physically active if possible.
- Control your diet. You should not eat food high in animal proteins and fats. Find the person an adequate replacement for his favorite products.
- Help me find friends. A person needs communication not only in his usual circle. If the patient cannot leave the house, you can find friends on social networks, for example, in multiple sclerosis groups. This way she will feel that she is not alone in her illness.
Diagnostics
Many diseases, especially at the first stage, are very similar in symptoms and clinical manifestations to multiple sclerosis. Therefore, in order to make an accurate diagnosis, a complex of studies is important. Classical computed tomography, CT agnography, laboratory diagnostics, cerebrospinal fluid puncture, Holter ECG, electroencephalography are of great help in making a diagnosis.
Tomography
The basic diagnostic procedure for detecting multiple sclerosis is tomography.
CT and CT agnography are available at the 5th hospital
CT helps detect large foci of demyelination and a number of other signs that occur in patients with multiple sclerosis.
Huge advantages in using CT agnography:
• The diagnostic method helps to organize the search for narrowings, dilations in the vessels or a complete cessation of blood movement through them. Allows you to create a complete picture of the condition of blood vessels.
• It is a radiological contrast study.
• Good alternative if MRI is contraindicated.
If it is necessary to determine the number and localization of areas of destruction of the myelin sheath of nerve fibers, the world of diagnostics also uses a type of tomography such as MRI.
Laboratory diagnostics
The examination is comprehensive. The following indicators are taken into account:
- Leukocyte formula.
- Glucose.
- Protein.
- Total number of cells.
- Albumen.
- Myelin protein (protein component of myelin).
- Opening pressure
- Oligoclonal IgG groups.
SSEP Study
Somatosensory evoked potentials are tested in some patients. They show how nerve impulses are transmitted to the brain from receptors in the lower and upper extremities. The method aims to look for delays in electrical responses to sensory stimulation.
SSEP is extremely important for diagnosing patients whose lesions are only in the spinal cord, and the brain is not affected by the disease.
Ultrasound of the brachiocephalic arteries (BCA)
A quick opportunity to take full control of the vessels of the neck, which are directly involved in the blood supply to the brain, to assess the degree of atherosclerotic lesions and metallogeny of the course of blood vessels in this area.
An ultrasound scan of the brachiocephalic arteries is very important if multiple sclerosis is accompanied by spinal osteochondrosis and there is a risk of stroke.
The vessels are viewed from different angles. The results of ultrasound diagnostics are a “picture” with the diameter and lumen of the vessels.
Holter ECG
In patients with suspected multiple sclerosis or its development, it is important to study in detail the state of the cardiovascular system as a whole. And you can’t just limit yourself to ECG here. The ideal option is a Holter ECG.
Monitoring is a recording of heart rhythm over a fairly large amount of time: a day or more.
At the same time, the heart rate is recorded in different phases: at rest, during movement, when eating food and, accordingly, chewing and swallowing it.
A solid picture of the rhythm (gastric extrasystoles, pauses), heart rate, and ischemic changes is visible.
Electroencephalography
- Electroencephalography allows you to graphically record the electrical activity of brain cells.
- The procedure is painless and harmless.
- The study is based on recording ultrasonic waves.
- Electroencephalography is effective for analyzing and monitoring brain structures and their displacements. Thanks to these results, the doctor can most accurately determine the degree of development of disorders.
Ophthalmological examination
70% of patients suffering from multiple sclerosis for more than 5 years have optic nerve disorders. Such patients require diagnostics of the structure of the eye disc, computer
computer perimetry to detect the affected area.
The changes in the retina and optic nerve head discovered during the examination are directly related to the level of degenerative lesions in the brain's white matter.
Diagnosis is based on anamnestic and clinical data. At the same time, in order to prescribe the correct treatment, it is important to determine the type of multiple sclerosis:
· Primary progressive. With the progression of the disease, but there are periods with periods of stabilization of the condition.
· Remitting. Two or more exacerbations, between which there is no increase in the severity of the disease. During periods of remission, complete restoration of impaired functions is possible;
· Secondary progressive. The severity of the neurological deficit is constantly and steadily increasing.
It is important to correctly determine the clinical form of the pathology. It can be cerebrospinal, spinal, optical, brainstem, or cerebellar.
Timely diagnosis is the key to choosing the right treatment regimen. But since the picture is often very blurred, it often takes 5 years from the onset of the disease to the diagnosis. This is due to the fact that many diseases are clinically similar. But the more comprehensive the examination, the higher the chance that the diagnosis will initially be made correctly, the patient will be prescribed adequate treatment in a timely manner, and no serious complications will arise.
Not frequent dizziness
Let's consider situations and diseases in which such symptoms may occur. Dizziness may not be systematic. but only a rare effect. However, this may be a signal of serious illnesses or developing pathologies.
Presyncope
In this state, which lasts no more than a few seconds or minutes, it seems to a person that surrounding objects are moving, he feels hot, sweats profusely, feels nauseous, his eyes become cloudy, vision may even disappear, and the person becomes pale. Presyncope usually occurs when the patient is sitting or standing, but not lying down. The cause may be orthostatic hypotension (a decrease in pressure after moving from a horizontal to a vertical position), arrhythmia and vasovagal crisis (excessive activity of the vagus nerve, leading to a decrease in heart rate).
Mental disorders
Depression, anxiety or panic disorder, alcohol addiction or personality disorder can lead to non-systemic dizziness. For example, if a person, in addition to this symptom, also has shortness of breath, rapid heartbeat and sweating, then most likely we are talking about a panic attack. A psychiatrist works with all these conditions.
Damage due to medication
Some aminoglycosides (for example, gentamicin) can be toxic to the vestibular system: they damage the hair cells of the inner ear, provoke imbalance and cause oscillopsia (the illusion of vibration of surrounding objects) when moving the head. This condition can become chronic.
Antiepileptic drugs, sedatives, and tranquilizers can also cause non-systemic dizziness. Sometimes blood pressure-lowering medications are too effective and blood pressure drops to abnormal levels, causing symptoms similar to dizziness.
Acoustic neuroma
When walking, a person begins to sway, surrounding objects move, his hearing may also deteriorate, and tinnitus may occur - these are the main symptoms of an acoustic neuroma (benign neoplasm). In most cases, such patients are prescribed surgery or radiation therapy.
Stranding syndrome (sea sickness on land)
After traveling on water, in very rare cases, a person may develop this syndrome: the patient feels that he is losing his balance, he is swaying, it seems to him that he is walking on uneven ground. This condition usually goes away within a couple of days. However, in more severe cases, your doctor may prescribe benzodiazepines or the antiepileptic drug clonazepam.
Non-systemic dizziness can also be caused by anemia (accompanied by fatigue, weakness and pallor), hypoglycemia (low blood sugar, which may be manifested by sweating and confusion), inflammation of the ear, heat stroke or dehydration.
Complications, prognosis
If treatment is not started in a timely manner, or treatment does not take into account the type of multiple sclerosis, the risk of complications is high:
- bursts of causeless, uncontrollable laughter and crying,
- urological infections,
- bedsores,
- tremor,
- epileptic seizures;
- paralysis in the upper and lower limbs,
- trigeminal neuralgia,
- depression,
- diplopia - double vision,
- Lhermitte's symptom is paresthesia (a sudden feeling of intense burning) with a sensation of electric current passing through the back.
Despite the fact that the disease is not simple, for some patients we can confidently voice a favorable prognosis.
If previously, when a diagnosis of “multiple sclerosis” was made, disability began to develop in most patients within 3-5 years, but now, with properly selected medications, it is possible to delay the progression of the disease by 10 and sometimes 20 years.
But much depends on the form of sclerosis. One of the most insidious is the primary progressive form. At first, the symptoms are most vague. The diagnosis is often not made immediately, and treatment, accordingly, is also delayed. But there are often cases when, 10 years after the onset of the disease, the patient simply cannot take care of himself and finds it difficult to move.
At the same time, up to 50% of patients are faced with a form of natural progression. while maintaining the ability to work and practically the usual way of life. The only thing is that they cannot visit baths or stay in the heat for a long time. The main difficulty is to learn to accept your diagnosis and live with it.
Types of PC
According to the clinical course, experts distinguish the following forms of MS:
- Relapsing-remitting form (RRMS). Secondary progressive form. It is characterized by rather pronounced manifestations. Exacerbations in this case are rare (or generally unnoticeable against the background of constant symptoms), but residual signs of multiple sclerosis are present during stabilization. 30–40% of patients are in this group.
- Primary progressive form (PPMS). The disease is constantly progressing, periods of improvement are insignificant. Exacerbations are not clearly identified. 10–15% of patients belong to this group. A striking example is when a patient’s vision begins to decline and is no longer restored (even for a short time), but only worsens.
- Secondary progressive course (SPRS). It is characterized by a slow deterioration of the condition, the occurrence of complications over a long period of time. This form of MS can be either active (with attacks) or not. Usually occurs after RRMS. Selective damage occurs to the myelin sheath that runs around the nerve fibers of the central nervous system.
- Progressive course with exacerbations. The disease is constantly progressing, with exacerbations occurring as MS develops. After each exacerbation, the patient's condition worsens. 5% of patients fall into this group.
To determine which group according to the course of the disease the patient belongs to, specialists prescribe a series of examinations.
Make an appointment
Relapsing-remitting form
As mentioned above, relapses in this form alternate with remission, during which no progression of the disease is observed.
To diagnose RRMS, a specialist needs to detect the spread of the disease in at least two areas of the central nervous system (affected areas of myelin, the substance that forms the sheath of nerve fibers). An important criterion here is the prevalence over time, that is, damage to these areas should occur at different times. If one of the criteria is not confirmed, a clinically isolated syndrome can be diagnosed with further clarification of the diagnosis.
With this form of the disease, patients usually experience the following symptoms:
- fatigue;
- numbness of the limbs;
- loss of vision;
- memory problems;
- disturbances in the functioning of the genitourinary system.
At the same time, people with progressive forms of MS are more likely to have problems related to the musculoskeletal system.
Primary progressive
This course of the disease is accompanied by sharp deterioration without early relapses and remissions. This form of MS is more difficult to diagnose. On average, PPMS occurs several years (about 8–10) after a relapsing-remitting course. Since in this course of MS the spinal cord is more often affected than the central nervous system, the patients’ problems are usually associated with walking, urinary and fecal incontinence.
Secondary progressive
This form can only be diagnosed in a patient already diagnosed with multiple sclerosis. To understand whether the transition from RRMS to SPMS has taken place, it is necessary to be constantly monitored by a neurologist and periodically do MRI. Due to the appearance of new foci in this course, exacerbations and relapses are possible, as with RRMS. The nature of the disease slowly moves from the demyelinating stage to the neurodegenerative stage, characterized by damage to nerve fibers and tissues.
Progressive with exacerbations
The rarest form in which the disease, starting with a remitting course, becomes primary progressive. In this case, symptoms increase, and neurological functions do not recover after exacerbations.
Treatment
Treatment of multiple sclerosis is aimed at solving several problems:
- stopping the active immunoinflammatory process,
- decreased activity of the immune system to nerve fiber sheaths,
- slowing down the development of the disease, stopping the appearance of new “plaques”,
- combating symptoms that significantly impair the quality of life.
To solve problems, medications and physiotherapy are used.
Complex drug therapy
During treatment, it is important to take immunomodulators and anti-inflammatory drugs. The following drugs are especially well known:
- Interferons beta. The drugs have an immunomodulatory effect on the main components of immune reactions.
- Medicines based on glatiramer acetate. Medicines in this group are capable of replacing myelin antigens and triggering the process of inhibition of T1 lymphocytes. In this case, T2 lymphocytes, on the contrary, are activated. Due to this, the drug has a neuroprotective and anti-inflammatory effect.
- Fingolimod. Modulator of sphingosine-phosphate receptors on lymphocyte membranes. Significantly reduces the number of “autoaggressive” T cells circulating in the blood.
- Natalizum. Slows down penetration through the blood-brain barrier and reduces the activity of T-lymphocytes in areas of axonal damage. The inflammatory process is significantly slowed down.
During exacerbations, when the disease is accompanied by obvious attacks, adrenocorticotropic hormone and corticosteroids (methylprednisolone) are used. Thanks to these drugs, it is possible to quickly reduce the movement of immune cells to the spinal cord and brain. But these drugs are only good as short-term therapy. They are not suitable for long-term use, as they can cause addiction.
If the disease is accompanied by signs of depression, the doctor may prescribe amitriptyline or melipramine. However, the prescription of these drugs is done extremely carefully - only after a detailed examination. Unfortunately, many patients already have urinary retention, and amitriptyline and melipramine can significantly aggravate the situation. An alternative for such patients can be all kinds of selective inhibitors without anticholinergic properties, but with an excellent ability to reuptake serotonin. These drugs include trazadone, sertraline, fluoxetine, and paroxetine.
Also, in the presence of depression, agomelatine has been widely used in recent years. This is a drug with a melatonergic mechanism of action. It normalizes circadian rhythms (oscillations).
If you have problems with urination, targeted therapy is needed to solve this problem.
If the main problem is urgency, tolterodine oxybutynin, amitriptyline, nifedipine are used.
If concerns are associated with emptying the bladder, the blocker terazosin helps. But it is important that when taking the drug there is careful monitoring to ensure that orthostatic hypotension does not develop.
Some patients may also be additionally prescribed medications aimed at reducing external sphincter tension. Among them are diazepam, tizanidine.
The above drugs are used in tablet and injection forms.
Hypobaric oxygenation
Oxygen saturation is a big help for patients with multiple sclerosis. This is possible through the hypobaric oxygenation procedure.
Hypobaric oxygenation is especially relevant for patients in whom multiple sclerosis is accompanied by cardiovascular diseases and diabetes.
Hypobaric oxygenation is carried out in a pressure chamber. Oxygen is supplied under high pressure. During the process of hypobaric oxygenation, adaptation and regeneration mechanisms are activated.
Massage
An excellent way to reduce discomfort and pain in patients with different types and stages of sclerosis is massage. Massage is especially useful for solving the following problems:
- Relaxes muscles and relieves spasticity.
- Activation of blood circulation.
- Preventing bedsores. Relevant for people who have to spend most of their time in bed.
Diet therapy for multiple sclerosis
- A common principle for all patients with multiple sclerosis is to limit sources of fast carbohydrates in the diet. The main ones are sugar and baked goods made from refined flour.
- The remaining principles of nutrition largely depend on what specific problems the patient has in each particular case.
- If chewing is difficult, it is recommended to eat pureed foods.
If you have constipation, you should use more liquid foods (if there are no problems with the urinary system at the same time) and products with bifidobacteria.
How to help loved ones cope with illness
Chronic pathology becomes more and more severe over time. Attacks occur suddenly, at least 2 times a year. Often people lose the ability to move, care for themselves, and become helpless. The boarding house “Quiet House” has created all the conditions so that patients with multiple sclerosis from Voronezh feel as comfortable as possible:
constant supervision of doctors and health workers;
- comfortable beds and anti-decubitus mattresses;
- full sleep - the patient is not distracted by the hustle and bustle of the home;
- balanced feeding and drinking regime;
- if necessary, assistance with feeding and personal care;
- caring and understanding attitude.
Conclusions:
- Multiple sclerosis is a pathology affecting the nervous system. It is based on damage to the sheaths of nerve fibers and disruption of impulse conduction.
- The disease is not hereditary, but with certain combinations of genes the risk is higher.
- Increased background radiation, intoxication, stress, and previous injuries can provoke the development of the disease.
- When the first symptoms of multiple sclerosis appear, it is important to consult a doctor promptly. It’s better to have it confirmed that it’s just overexertion and fatigue, and not to find yourself in a situation where one on one is the acute phase of the disease.
- With multiple sclerosis, the quality of life deteriorates significantly. First of all, because physical activity decreases. But, if previously multiple sclerosis was immediately a death sentence, now there are methods and drugs through which it is possible not only to relieve the symptoms of the disease, but also to slow down the development of the disease. Doctors have learned to keep the disease under control. With timely diagnosis and treatment, the pathology no longer negatively affects life expectancy.
- CT and laboratory diagnostics play an important role in diagnosis. When clarifying the diagnosis, it is essential where the problem areas are located: in the brain or spinal cord.
In the 5th hospital of the city, treatment of multiple sclerosis is one of the main profiles. The hospital base has expert-class equipment for diagnosing this disease. Consultations with experienced neurologists are available. Treatment is approached in a comprehensive manner. Drug therapy, massage, physical therapy, including cycling on special simulators, and hypobaric oxygenation sessions are organized.
Forecast
It is not yet possible to completely eliminate the symptoms of MS, but maintenance therapy will help prevent the onset of disability, which in itself is very important. It is necessary to remember the following risks for patients diagnosed with MS:
- before 15 and after 40 years, the risk of complications increases;
- mental disorders or concomitant disorders/diseases can hasten death;
- disruptions in the functioning of vital organs (kidneys, lungs, heart) can lead to instant death.
To prevent any of this from happening, you need to constantly monitor the patient’s condition and consult a specialist in time to prevent complications. As for the life expectancy of people with MS, much depends on how quickly the correct diagnosis was made. A diagnosis made at an early stage and proper treatment are the key to a long and happy life for the patient.