Transient ischemic attack of the brain is a temporary acute disorder of the central nervous system. In medical practice, such a pathology may also be called a microstroke. The only difference is the duration of symptoms. In the case of transient ischemia, the signs disappear within an hour; they do not have irreversible consequences. Most often, this type of disorder is found in older people.
Diagnosis is carried out on the basis of the totality of all information obtained through medical research: computed tomography, magnetic resonance imaging, ultrasound and PET scans of brain regions. Additionally, laboratory procedures may be prescribed. It is advisable to undergo the examination in specialized neurological centers.
Treatment of transient ischemic attack of the brain can be conservative, symptomatic and surgical. It all depends on the patient’s age, the presence of concomitant diseases and general condition. Therapy is necessary to eliminate the risk of stroke. According to statistics, a patient’s risk of stroke after 2 days after an attack is 4%, after 30 days - 8%, within 5 years - 29%.
ICD-10 code
TIA in ICD-10 (International Classification of Diseases, 10th revision) is as follows: Transient transient cerebral ischemic attacks (attacks) and related syndromes (G45). TIA is included in the group of episodic and paroxysmal disorders (G40-G47).
A transient ischemic attack occurs as a result of blockage of a vessel supplying the brain. Atherosclerotic plaques or blood clots may form in the vessel, interfering with normal blood flow. Rarely, TIA occurs as a result of hemorrhage. However, in this case, blood circulation is restored quite quickly.
Make an appointment
Physiology of the disease
TIA develops due to the inability of blood vessels to supply neurons with oxygen. The severity of the condition can vary greatly. Doctors often find it difficult to draw a clear line between a transient attack and an ischemic stroke, since they develop according to a similar scenario.
At the moment, there is only one criterion that allows you to distinguish a TIA from a stroke - TIA lasts less than 24 hours. With a stroke, circulatory disturbances persist for more than a day.
Causes
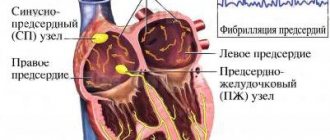
TIA is not an independent disease; its occurrence is associated with pathologies of the cardiovascular system, blood clotting problems, vascular injury and large blood loss. The causes of thromboembolism are most often associated with:
- atrial fibrillation;
- sick sinus syndrome;
- mitral stenosis;
- atrial fibrillation;
- dilated cardiomyopathy;
- infective endocarditis;
- atrial myxoma;
- acute heart attack;
- thrombosis of the left atrium.
TIA can occur in patients with:
- patent oval valve;
- artificial heart valve;
- mitral valve calcification;
- heart disease;
- heart failure;
- angiopathy;
- coagulopathy;
- abnormalities in the vertebral and carotid arteries.
Carotid artery lesions
The appearance of typical symptoms is observed after a 2-5 minute period. When the circulation of the circulatory system in the area of the carotid artery is dysfunctional, the patient feels weak, suddenly loses vision, and completely or partially stops speaking.
Motor dysfunction of the limbs on one side is often observed, and the patient also loses sensation.
The pulse drops rapidly and a noise is heard in the carotid artery. The disease may be indicated by focal symptoms of damage to the brain structures of the head: the face becomes asymmetrical, the pressure fluctuates, the retina changes.
There is a feeling of heaviness in the sternum area, the heart is working intermittently, there is not enough air to breathe, convulsions appear, and you want to cry.
Risk factors
In most cases, transient ischemic attack is caused by atherosclerotic plaques blocking small blood vessels. The risk group for developing transient ischemic attack includes persons suffering from the following diseases and conditions:
- atherosclerosis of cerebral vessels - this pathology is considered the main cause of ischemic attacks. 90% of strokes in older people are caused by atherosclerosis;
- arterial hypertension – ranks second in the incidence of strokes;
- hereditary predisposition - if any of the family members have similar conditions in the past, the likelihood of developing an ischemic stroke increases;
- age factor - after 60 years, the risk of developing the disease increases significantly.
- diabetes mellitus – hypertension and increased blood clotting in patients with diabetes lead to worsening atherosclerotic damage to blood vessels;
- systemic vascular diseases;
- obesity – excess body weight is quite often the cause of ischemic attacks;
- heart diseases;
- osteochondrosis of the cervical spine, especially spasm of the cervical artery;
- alcohol abuse and smoking.
According to statistics, transient ischemic attacks more often affect middle-aged male patients. However, symptoms can also appear in childhood and young adults with cardiovascular disease.
Diagnosis of transient ischemic attack is carried out on the basis of information obtained during medical research:
- computed tomography;
- magnetic resonance imaging;
- Doppler ultrasound;
- positron emission tomography of all parts of the brain.
To make the most accurate diagnosis, additional laboratory procedures may be prescribed.
Paroxysmal systemic dizziness
Paroxysmal systemic dizziness is the most common symptom of focal circulatory disorders, both in the brain stem and in the structures of the inner ear.
A reliable criterion for brainstem vertigo, according to Sarklinik, is the combination of dizziness with cerebral symptoms proper, for example oculomotor, visual, pyramidal, and sensory symptoms. A reliable criterion for peripheral dizziness is the combination of dizziness with cochlear disorders.
The manifestation of paroxysmal dizziness in the form of a monosyndrome in most cases indicates its peripheral origin.
In the differential diagnosis of peripheral or central dizziness, the phenomenon of accelerated growth of vestibular excitability - vestibular recruitment - is of great importance. With central vertigo it is negative, with peripheral vertigo it is positive.
Clinical manifestations
A transient ischemic attack contributes to the occurrence of temporary neurological symptoms. Therefore, at the time of consultation, the neurologist does not have all the signs; the specialist is based only on the patient’s complaints during the interview. Depending on the location of the pathology, the clinical picture will also change.
Disorders in the vertebrobasilar region (VBP) cause unsteadiness of gait, instability, dizziness, dysarthria (fuzzy speech), vision problems, and sensory abnormalities.
Changes in the carotid system lead to a sharp deterioration in vision, temporary blindness of one of the organs, impaired mobility in the limbs, and rarely convulsions. These signs are short-term.
TIA in the retinal area, when the pathology affects the artery of the visual organs, which leads to transient blindness. Patients complain of an obstacle in the form of a “curtain”.
A TIA attack lasts no more than 15–20 minutes, after which all neurological manifestations disappear. It is because of this short-term ailment that people do not pay attention to it and do not visit the clinic. This disorder can occur once in a lifetime or recur regularly (up to three times a day). There are as many manifestations of TIA as there are functions of the brain. Temporary deviations can be observed in speech, memory, and behavior.
Pathogenesis
Ischemia of brain tissue is a transient disorder of cerebral blood supply, which is also called a microstroke. In this case, neurological symptoms disappear spontaneously within an hour after the end of the attack, without causing irreversible organic damage to the structures of the brain.
Transient ischemic attacks usually develop in conditions of atherosclerotic occlusion of the main vessels bringing blood to the head. These include the carotid artery system - especially at the bifurcation sites, as well as the vertebral arteries. Most often, the pathogenesis is facilitated by compression and vasospasm caused by osteochondrosis .
Mechanism of development of TIA
Ischemia of cerebral tissue includes 4 stages:
- Autoregulation - which occurs due to compensatory dilation of cerebral vessels as a response to reduced perfusion pressure of cerebral circulation, causes an increase in the volume of blood that fills the vessels of the brain.
- Oligemia - a further increase in the fall in perfusion pressure indicators causes a decrease in cerebral blood flow, when it cannot be compensated by autoregulatory mechanisms; at this stage, the processes of oxygen metabolism are not yet disrupted.
- Reversible ischemia is the development of an “ischemic penumbra” caused by an increasing decrease in perfusion pressure and a decrease in the level of oxygen metabolism, which leads to hypoxia and disruption of neuronal function.
- Irreversible ischemia is irreversible cell death or apoplexy depolarization of neurons.
Thus, a microstroke causes disturbances in cerebral hemodynamics, sudden and short-term dyscirculatory disorders in the structures of the brain, manifested by focal and general cerebral symptoms that persist throughout the day.
General signs
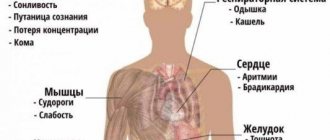
Common signs of a TIA include:
- severe tinnitus;
- flashes of light in the eyes;
- severe hiccups;
- nausea or vomiting;
- speech problems;
- pain in the back of the head;
- dizziness;
- severe headaches;
- coordination problems;
- convulsive state;
- blood pressure surges;
- transient amnesia.
Patients experience pale skin, absent-mindedness, and inability to concentrate. If the pathology is localized in the cervical region, then situational attacks cause the appearance of severe muscle weakness - the patient may fall, lose the ability to freely move the limbs, most often the victim is fully conscious. In severe cases, a person requires immediate emergency care.
Complications and consequences of ischemic attack of the brain
A transient attack is characterized by incoming symptoms as a result of impaired cerebral circulation. They should pass within 24 hours and not provoke serious consequences. Symptoms that persist after a severe microstroke include:
- slurred speech;
- amnesia;
- paralysis;
- deterioration of visual acuity.
For rehabilitation after a mini-stroke and the most successful prognosis - prevention of ischemic stroke, the help of many specialists is needed:
- neurologist – monitors the condition of cerebral vessels, the functioning of neurons and the level of metabolic processes in the brain;
- cardiologist - will select the best treatment regimen to normalize blood pressure and heart rate;
- endocrinologist - will help adjust blood sugar levels and neutralize the negative effects of diabetes ;
- speech therapist - a specialist who will help solve speech problems;
- psychologist – necessary for the correction of mental disorders.
Severity criteria
There are 3 degrees of severity of TIA. They indicate the positive or negative dynamics of the disease:
- mild degree - lasts approximately 10 minutes, focal symptoms that disappear without consequences;
- moderate degree - lasts from 10 minutes or more, the attack occurs without consequences for the patient’s health;
- severe - transient cerebral ischemic attack is prolonged, and neurological signs worsen.
According to ICD-10, transient ischemic attack has a standard classification:
- TIA in the VBB (vertebrobasilar area);
- TIA in the carotid region;
- TIAs are multiple or bilateral;
- transitional blindness syndrome;
- TGA (transient global amnesia);
- unspecified TIA.
The type and severity of local decrease in blood circulation in the head can only be determined by a qualified medical professional.
Diagnostics
If you follow the recommendations of the World Health Organization, then all patients with suspected TIA should be taken to a regional vascular center. The speed of the examination (within 24 hours) will significantly increase the chances of finding out the picture of general changes. The list of procedures includes:
- conducting MRI using diffusion-weighted images and gradient T2-weighted images;
- A CT scan is performed if it is not possible to do an MRI;
- ultrasound examination of the vessels of the head and neck if there is a suspicion of a stroke;
- clinical examination of physiological parameters with blood tests;
- conducting an ECG.
Additional procedures include:
- echocardiography;
- checking blood for clotting;
- biochemical blood tests.
The diagnostic criteria for transient ischemic attack are based on the ABCD2 scale, which is widely used in Western Europe and the USA. It can be used to predict the risk of stroke in patients who have suffered a TIA.
The assessment school looks like this:
- A - blood pressure indicators;
- B — patient’s age (over 60 years);
- C — symptoms of the disease (general list of ailments);
- D—duration of symptoms and history of diabetes.
This approach allows for an objective assessment of both mild and more severe manifestations of ischemia.
A complete examination of the patient will allow differentiation of TIA from other diseases, such as:
- Neurological disorders: migraines, focal seizures, brain tumor, subdural hematoma, hemorrhage, multiple sclerosis, myasthenia gravis, paralysis and narcolepsy.
- Somatic and mental disorders: hypoglycemia, Meniere's disease, vestibular neuritis, syncope, orthostatic hypotension, hysteria, psychosomatic abnormalities.
There is a range of significant signs with the help of which we can more likely speak about the correct differentiation of acute VBD from other diseases. These include:
- rotational dizziness;
- degree of feeling of unsteadiness or stability in an upright position;
- balance problems;
- the presence of cystic-glial changes in the head;
- the presence of atherosclerosis of the brachiocephalic arteries with stenosis exceeding 50%.
TIA is characterized by the presence of several signs, so the patient’s condition requires a qualitative analysis.
Symptoms of transient ischemic attack
Symptoms of an ischemic attack of the brain can vary significantly depending on which part of the brain is affected, but there are a number of clinical disorders that are general cerebral symptoms, these include:
- dizziness;
- headache;
- short-term loss of consciousness.
Focal symptoms of cerebral circulatory disorders manifest themselves as:
- temporary loss of speech and speech disorders - aphasia;
- loss of the ability to read and/or write;
- weakness in one half of the body - hemiparesis , causing loss of balance and impaired coordination of movements;
- strabismus or immobility of the eyeballs, loss of vision or its sharp deterioration;
- involuntary urination;
- numbness - hypoesthesia , sensitivity and tingling - paresthesia .
Treatment
The most important thing is to provide the victim with appropriate assistance in a timely manner, since it is difficult to make a diagnosis at first glance. You should know that emergency care is available. This is a series of specific actions aimed at stabilizing the patient’s condition and hospitalization:
- calling an ambulance;
- control of breathing, heart rate and blood pressure;
- relief of convulsive syndrome.
The victim should be given the opportunity to breathe freely: loosen his tie or unbutton the top buttons of his clothes, open the window. Be sure to take a horizontal or half-sitting position. If vomiting occurs, clear the airways. The patient can be given a small amount of water.
The goal of TIA therapy is to prevent subsequent attacks with the development of complications. First of all, the decrease in blood supply is stopped, followed by restoration. Doctors select treatment based on the underlying disease: diabetes mellitus, arterial hypertension, thromboembolism or other pathologies.
The duration of treatment depends on the specific case. The patient can undergo the recovery period on an outpatient basis or in a clinic. He may be prescribed:
- infusion therapy, when Reopoliglucin or Pentoxifylline is injected drip into a vein;
- antiplatelet agents: acetylsalicylic acid, Clopidogrel, which prevent the formation of blood clots;
- anticoagulants: Clexane, Fraxiparine. They require monitoring of blood counts;
- neuroprotectors: Magnesium sulfate, Ceraxon, Actovegin. With their help, nerve cells receive appropriate protection from oxygen starvation;
- nootropics: Cerebrolysin, Piracetam;
- statins: Atoris, Vaseline - help lower the concentration of cholesterol in the blood;
- antiarrhythmic drugs are prescribed for heart rhythm disturbances;
- antihypertensive agents: Lopril.
According to indications, symptomatic treatment can be carried out, which is prescribed individually. The attending physician may prescribe physiotherapeutic procedures, including:
- Oxygen barotherapy is a treatment with an air environment with a high oxygen content, which promotes cell regeneration.
- Electrosleep is therapeutic; it allows subcortical connections to be restored through exposure to a safe pulsed current.
- Electrophoresis - the effect of current pulses in combination with the administration of drugs.
- DDT (diadynamic therapy) is one of the methods of electrotherapy, when the patient’s body is exposed to Bernard currents. They have low frequency and voltage.
- SMT is the effect of sinusoidal currents on biological tissues. They have a beneficial effect on the entire body.
- Microwaves - human tissues and organs are affected by a specially created electromagnetic field, its wavelength is 12.6 cm, and its frequency is 2375 MHz.
- A circular shower is a useful hydroprocedure; its principle is the needle-like effect of streams of water on the human body over the entire surface. The water from such a shower envelops the entire body. The procedure takes place in a special box, which is equipped with a large number of tubes, from which water is supplied.
- Therapeutic baths (pine, radon, pearl).
According to indications, massage procedures aimed at improving blood circulation can be used. Surgical intervention is prescribed for atherosclerotic lesions of extracranial vessels. This procedure has 3 varieties:
- carotid endarterectomy - removal of atherosclerotic plaque located inside the vessel;
- arterial stenting - the procedure is performed on narrowed arteries;
- prosthetics - the affected area of the artery is removed and replaced with a graft.
A patient suffering from a TIA requires professional advice from appropriate specialists. Treatment after a transient ischemic attack will depend on the cause of the attack, frequency and age of the patient. If the symptoms are mild and attacks are sporadic, then recovery is quick.
Neurological rehabilitation after transient ischemic attack at the Yusupov Hospital
The rehabilitation clinic of the Yusupov Hospital is a unique medical institution, whose specialists direct all their efforts to restore patients’ body functions lost due to illness.
Our rehabilitation doctors include unique rehabilitation programs, innovative medical technologies and techniques in the scheme of rehabilitation measures.
Exercise after transient ischemic attack and stroke
Physical therapy (physical therapy) is a mandatory and very powerful tool for recovery after a transient ischemic attack. Neurologists at the Yusupov Hospital prescribe it in the first days after an attack. Exercise therapy should be performed at all stages of treatment, and ideally throughout the rest of life.
In terms of the strength of its positive effects, regular physical exercise after a transient ischemic attack and stroke can compete with even the most modern medications.
Physical exercises after transient ischemic attack and strokes have the following objectives:
- prevent complications of long-term immobilization (bedsores, congestive pneumonia, progression of congestive heart failure, thromboembolic complications, muscle atrophy);
- improve muscle tone and strength in muscles that are in a state of paresis or paralysis with reduced tone;
- pathological muscle tone in muscle groups in a state of spastic paresis or paralysis with increased muscle tone;
- improve microcirculation and metabolic processes in all tissues of the body;
- prevent muscle contractures;
- resume physical activity;
- restore the body’s speech functions;
- normalize the activity of internal organs;
- restore fine movements of the hands.
Therapeutic exercise is effective, but not the only method of rehabilitation after transient ischemic attack and stroke. The highest effectiveness is achieved if exercise therapy is combined with massage, manual therapy, occupational therapy, social and psychological adaptation.
Rehabilitation after a transient ischemic attack at the Yusupov Hospital is a full-fledged recovery program that allows you to avoid the development of severe consequences of cerebrovascular accident.
EPIDEMIOLOGY
Numerous cohort studies in different countries have demonstrated mixed incidence of TIA, which ranged from 0.37 to 1.1 per 1000 people per year. Like strokes, the risk of TIA increases significantly with age. In one British study, the incidence of TIA among people over 85 years of age reached 6.41 per 1000. According to the Cardiovascular Health Study (1993), the prevalence of TIA was 2.7% among men 65–69 years of age and 1.6% among women of the same age. age, and in persons 75–79 years old it increased to 3.6% and 4.1% in men and women, respectively. At the same time, in people who have had a stroke, a history of TIA is observed in a fairly significant number of cases - from 7 to 40%. This wide variation is believed to be explained by a number of factors, including different criteria for diagnosing TIA in different studies. Many TIAs remain undiagnosed.
ETIOLOGY AND PATHOGENESIS
Various risk factors can lead to the development of TIA as one of the variants of acute cerebrovascular accident.
The leading risk factor is atherosclerosis of the main arteries of the head with the formation of hemodynamically significant stenoses and embologenic plaques. In almost 90% of cases, the development of TIA is caused by atherothrombosis of the carotid arteries, most often at the site of their bifurcation into external and internal.
The second most common factor is the presence of blood clots in the cavities of the heart and on its valves in atrial fibrillation (AF), dilated cardiomyopathy, myocardial infarction, artificial heart valves, bacterial and non-bacterial endocarditis.
Much less often, TIAs develop as a result of:
- coagulopathies;
- angiopathy caused by arterial hypertension, diabetes mellitus or other reasons;
- developmental anomalies (kink, duplication, hypo- or aplasia) of the carotid or vertebral arteries, coarctation of the aorta;
- extravasal compression of the vertebral arteries by pathologically altered cervical vertebrae;
- dissection of the carotid or vertebral arteries.
The main mechanism for the development of TIA is the entry of microemboli from the main arteries of the head or heart into the small vessels of the head. This is accompanied by an acute, but reversible (without the formation of a heart attack) critical decrease in blood supply to a region of the brain in a certain arterial basin. The key point in the pathogenesis of TIA is precisely reversible local cerebral ischemia, which develops when cerebral perfusion decreases below 18–22 ml per 100 g/min. (at a norm of 50–60 ml per 100 g/min), which is the functional threshold for ischemia.
A transient drop in blood flow in the area distal to the site of arterial occlusion leads to the appearance of focal symptoms. When blood flow is restored as a result of autoregulation mechanisms and the opening of collaterals, regression of focal symptoms and completion of the vascular episode are observed. In the event of a further drop in perfusion below the threshold of reversible changes (8–10 ml per 100 g/min), a cerebral infarction is formed.
CLASSIFICATION
There is no generally accepted classification of TIA.
In clinical practice, a classification corresponding to the classification of ischemic stroke (TOAST classification) is often used, according to which the following types of TIA are distinguished:
- atherothrombotic - due to atherosclerosis of large arteries, leading to their stenosis or occlusion. When an atherosclerotic plaque or thrombus fragments, an arterio-arterial embolism develops, which is also included in this type of stroke;
- cardioembolic – the most common causes are atrial fibrillation, valvular heart disease, myocardial infarction, especially less than 3 months old;
- lacunar - due to occlusion of small-caliber arteries, the damage of which is associated with arterial hypertension or diabetes mellitus;
- TIA associated with other rarer causes - non-atherosclerotic vasculopathies, hypercoagulation, hematological diseases, hemodynamic mechanism of development of focal cerebral ischemia, dissection of the arterial wall;
- TIA of unknown origin, which includes strokes with an unknown cause or with two or more possible causes, when it is impossible to make a definitive diagnosis.
DIAGNOSIS
The main objectives of diagnosing TIA are:
- exclusion of cerebral infarction in the first hours from the development of TIA;
- exclusion of other diseases with a clinical picture similar to TIA;
- determination of the etiology of TIA with the aim of timely initiation of targeted prevention of cerebral infarction.
The diagnostic algorithm for TIA is the same as for ischemic stroke.
Considering the high risk of developing ischemic stroke in a patient with TIA, examination and treatment should be carried out immediately in a hospital setting.
Clinical signs and symptoms
TIA is a cerebrovascular disease with transient neurological symptoms. Symptoms of TIA are mostly the same as those of patients with ischemic stroke and include unilateral limb weakness, difficulty speaking, sensory disturbances, and difficulty walking. Since these symptoms are temporary, they are often assessed on the basis of the patient’s story; the diagnosis of TIA is made retrospectively, since at the time the patient is examined by a specialist, focal neurological symptoms are no longer present (Fig. 1).
TIAs in the carotid artery system are manifested by transient mono- or hemiparesis, sensory disturbances (mono- or hemianesthesia), and speech disorders.
TIAs in the vertebrobasilar system are characterized by short-term vestibular and cerebellar disorders (ataxia, systemic dizziness, dysarthria). Sometimes hemianopsia or transient visual impairment in both eyes occurs.
Transient blindness. Transient monocular blindness (TMB), or amaurosis fugax, is a condition of often unilateral, sudden short-term (usually within a few seconds) loss of vision due to transient ischemia in the area of the blood supply of the ophthalmic, posterior ciliary arteries or retinal arteries. Visual impairment is often described by patients as a “curtain” or “damper” that has moved from top to bottom or bottom to top. Sometimes vision loss is limited to the upper or lower half of the visual field. TMS usually occurs spontaneously, without provoking factors, but can sometimes be triggered by bright light, changes in body position, exercise, or a hot bath. Painful sensations are not typical for TMS.
Transient global amnesia (TGA) is a unique syndrome in which a patient, usually of middle age, suddenly loses short-term memory with relative preservation of memory for distant events. The patient's consciousness and orientation in his own personality are not impaired, but there is incomplete orientation in space and the environment. There is a stereotypical repetition of the same questions and confusion. The etiology of this dramatic syndrome remains unknown; they are trying to explain it by ischemia of the hippocampal-fornical system. Some authors consider this pathology an epileptic phenomenon or a variant of migraine. Episodes of TGA are often triggered by certain factors, such as emotional distress, pain, and sexual intercourse. Attacks usually last from several tens of minutes to several hours. Memory recovery after the attack is complete. As a rule, the patient fully or partially remembers the events that occurred during the amnesia episode. There is no neurological deficit. The tendency to recur is small, the frequency is rare - once every few years.
Differential diagnosis
In order to carry out a differential diagnosis of TIA and diseases that mimic it, a thorough history taking, clinical examination, palpation and auscultation of the carotid arteries are necessary (in the presence of a systolic murmur at the site of bifurcation of the common carotid artery into the external and internal - in the area of the angle of the lower jaw, contralateral neurological symptoms, it is highly likely to assume the development of a TIA), as well as appropriate imaging methods (Fig. 2).
The difficulty of diagnosing TIA is due to a wide nonspecific palette of symptoms, which determines the need for differential diagnosis. Differential diagnosis is carried out with various pathological processes that can manifest as transient neurological disorders:
- ischemic stroke with rapid regression of focal symptoms;
- hemorrhagic stroke with rapid regression of focal symptoms;
- a brain tumor;
- traumatic brain injury;
- partial epileptic seizure;
- associated migraine;
- demyelinating disease;
- hyperventilation syndrome;
- conversion disorder;
- autoimmune processes;
- hypoglycemic state and other dysmetabolic processes.
- Symptoms not typical for TIA:
- disturbance of consciousness;
- isolated non-systemic dizziness;
- general weakness;
- fainting;
- flickering (sparkling) scotoma;
- isolated tinnitus;
- urinary and/or fecal incontinence;
- gradual progression of symptoms (especially sensory ones) involving several parts of the body;
- acute behavioral disorders.
Laboratory and instrumental studies
Laboratory research
Basic methods:
- general clinical blood test with determination of hematocrit and platelet count;
- general urine analysis;
- international normalized ratio (INR), activated partial thromboplastin time (APTT), prothrombin time, fibrinogen;
- blood glucose;
- total cholesterol, high and low density lipoproteins, triglycerides;
- blood electrolytes (potassium, sodium, calcium, chlorides);
- transaminase activity, total direct bilirubin;
- urea, creatinine;
- creatine phosphokinase, C-reactive protein;
- total protein.
Additional (according to indications):
- determination of antiphospholipid antibodies;
- identification of various hypercoagulopathies;
- determination of homocysteine;
- protein fractions;
- blood test for HIV, syphilis, hepatitis B, C;
- molecular genetic tests for suspected hereditary syndromes (MELAS, CADASIL Fabry, etc.).
Instrumental studies
Basic methods
The main methods for diagnosing TIA are imaging studies (brain, blood vessels, heart), which allow:
- exclude ischemic and hemorrhagic stroke (cerebral infarction, hematoma, subarachnoid hemorrhage);
- carry out differential diagnosis with non-vascular diseases of the brain;
- determine the mechanism of development of TIA (atherothrombosis of a large vessel, cardiac source of embolism) and choose rational stroke prevention.
Computed and magnetic resonance imaging
Magnetic resonance imaging (MRI) or computed tomography (CT) of the head is indicated in all patients in whom a TIA is suspected based on the clinical picture.
The method of choice for neuroimaging for suspected TIA is MRI using diffusion-weighted images (DWI), which provides the most accurate early assessment of ischemic brain damage.
If MRI is contraindicated (patients have pacemakers, metal staples on an aneurysm, metal heart valves) or is unavailable, an X-ray CT scan is performed. This method allows for differential diagnosis with spontaneous and traumatic intracranial hemorrhages.
Urgent ultrasound examination of the vessels of the head and neck
A mandatory component of diagnosing a patient with TIA is non-invasive ultrasound visualization of the vessels of the neck and preferably intracranial vessels. This method makes it possible to identify steno-occlusive lesions of carotid vessels and determine the need for surgical restoration of cerebral blood flow.
Duplex scanning (DS) of the main (extracranial) arteries of the head (MAG) is used to diagnose stenoses, potentially embologenic atherosclerotic plaques in the MA, violation of the integrity of the vascular wall with the formation of intramural (intramural) hematoma and the presence of anatomical abnormalities. Based on the results of DS, additional information is obtained about blood flow, hemodynamic disorders and the degree of their severity.
Transcranial Dopplerography (TCDG) of cerebral arteries with microembolodetection makes it possible to assess the condition of intracranial arteries and detect the circulation of emboli in them.
Magnetic resonance angiography (MRA) or CT angiography is indicated in cases where DS does not provide a reliable result. As a rule, this occurs with the development of ischemia in the vertebrobasilar system.
Additional instrumental methods (aimed at clarifying risk factors for TIA):
EchoCG is indicated for suspected cardioembolic mechanism of TIA in cases where the history and/or physical examination indicate the possibility of cardiac pathology, when the patient’s age exceeds 45 years, and also when the results of examination of the vessels of the neck, brain and blood tests do not reveal the cause TIA. Transesophageal echocardiography is more informative than transthoracic echocardiography in determining the pathology of the interatrial septum (septal aneurysm, patent foramen ovale, etc.), atrial thrombi and valve diseases.
Carotid angiography is a standard diagnostic procedure before performing carotid endarterectomy. It is also indicated in patients with TIA if DS and MRI (CT angiography) give conflicting results or if they are not possible.
EEG is indicated for patients who need to make a differential diagnosis of TIA and epileptic seizure.
Holter 24-hour ECG monitoring according to indications.
Daily blood pressure monitoring according to indications.
Fundus examination, perimetry as indicated.
Formation of diagnosis
The clinical diagnosis of TIA reflects the vascular system or basin in which transient cerebral ischemia occurred (carotid artery syndrome or vertebrobasilar arterial system syndrome), as well as the background process that led to the acute vascular complication of TIA, similar to how it is formulated for stroke. Two types of TIA have their own codes in the international classification of diseases - transient blindness (amaurosis fugax), which occurs as a result of embolism of the ophthalmic artery, and transient global amnesia, which develops with bilateral ischemia of the mediobasal parts of the temporal lobes.
TREATMENT
According to international recommendations for the management of patients with ischemic stroke and transient ischemic attacks, if TIA is suspected, patients should be immediately hospitalized in the department for the treatment of acute cerebrovascular accidents (Fig. 3). This approach is due to their high risk of developing a stroke in the coming hours, as well as the need for differential diagnosis with other diseases and conditions resembling TIA.
Treatment and secondary prevention of stroke in patients with TIA are inseparable and begin from the moment of diagnosis.
Non-drug treatment
Surgery:
- is the leading direction in the treatment of patients who have suffered a TIA, as well as the prevention of stroke in the presence of hemodynamically significant stenosis (≥70%) or acute occlusion of the arterial artery;
- Angiosurgical restoration of blood flow is recommended within 24 hours after TIA;
- if there are individual contraindications to surgery in the acute period, the decision on surgical intervention is made as planned over the next 6 months;
- Carotid thromboendarterectomy is more often performed. Vascular stenting is carried out in special cases (difficult direct access to the vessel, high risk of perioperative complications, restenosis after carotid endarterectomy, etc.);
- Antiplatelet therapy is carried out before and after surgical treatment.
Drug treatment
Emergency pathogenetic therapy for in-hospital TIA in a neurovascular department should be carried out in the amount of AI therapy, especially on the first day of the disease, when in most cases both clinical and instrumental (CT, MRI) diagnostics do not yet provide convincing evidence in favor of one or another option .
As with AI, therapeutic measures consist of basic and specific therapy.
Basic therapy (includes control over the basic functions of the body and maintaining homeostasis):
- correction of blood pressure - it is advisable to maintain the level of mild arterial hypertension 160–180/90–100 mm Hg, and avoid a significant decrease in blood pressure, especially in patients with bilateral carotid artery stenosis;
- control of blood glucose levels, for hyperglycemia above 11 mmol/l - consultation with an endocrinologist regarding insulin therapy, for hypoglycemia below 3.3 mmol/l - administration of a glucose solution;
- control of water and electrolyte balance to avoid an increase in hematocrit and a decrease in the rheological properties of blood;
- electrocardiography - if arrhythmia is detected - daily monitoring and consultation with a cardiologist.
If it is necessary to lower blood pressure in severe arterial hypertension (>220/120 mm Hg), preference is given to the following drugs:
- the ultra-short-acting cardioselective beta-blocker esmolol is administered intravenously at a dose of 500 mcg/kg for 1 minute (loading dose), then 50 mcg/kg per minute over the next 4 minutes; maintenance dose – 25 mcg/kg per minute (or less);
- the α1-adrenergic receptor blocker urapidil is prescribed in a dose of 12.5–25 mg (1 ampoule contains 5 ml of a 0.5% solution, i.e. 25 mg). This amount of the drug is administered intravenously slowly over 5 minutes. The drug begins to act within 3–5 minutes. Duration of action is 4–6 hours. If the effect is insufficient, the administration of the same dose is repeated (with an interval of at least 15 minutes). The effective dose can vary from 25 to 100 mg. If the hypotensive effect is not persistent enough, a slow drip infusion of the drug is prescribed;
- ACE inhibitor captopril (used sublingually at a dose of 25 mg), enalapril orally at an initial dose of 5 mg, enalaprilat (administered orally intravenously slowly or drip over 5 minutes at a dose of 1.25 mg every 6 hours).
- in cases resistant to this therapy, it is possible to use an intravenous infusion of the peripheral vasodilator sodium nitrop-russide (start at a rate of 0.5 mg per 1 kg of body weight per minute under constant blood pressure monitoring).
Specific antithrombotic therapy
Antithrombotic therapy for patients with TIA begins immediately, performing both therapeutic and preventive functions, given the high risk of stroke in the first days after the development of TIA. The choice of drug is determined by the type of TIA - cardioembolic and non-cardioembolic.
For non-cardioembolic TIA, one of the platelet antiplatelet agents is prescribed:
- acetylsalicylic acid (Cardiomagnyl, Thrombo-ass, Cardio ASA, Aspirin Cardio, etc.) at a dose of 325 mg/day for 48 hours with a transition to 50–100 mg/day (at the rate of 1 mg per kg of patient weight);
- clopidogrel (Plavix, Egitromb) 75 mg;
- dipyridamole (75 mg 3 times a day);
- small doses (25 mg) of aspirin + 200 mg of slow-release dipyridamole in capsules 2 times a day (Agrenox).
For the cardioembolic mechanism of TIA development (most often as a result of AF), the treatment of choice is oral anticoagulants:
- warfarin is used with mandatory monitoring of the INR, maintaining it at a level of 2–3. The initial dose of warfarin is 2.5 mg, if necessary, the dose is increased until the target INR level is 2-3. Monitoring the INR and increasing the dose by 1.25 mg is carried out once a week. After dose titration, INR monitoring is reduced to once a month. Warfarin is used to prevent recurrent TIA or stroke in various cardiac sources of thrombi, both valvular (especially with artificial heart valves) and non-valvular;
- the so-called new oral anticoagulants are recommended for use only for non-valvular AF: dabigatran 150 or 110 mg (persons over 80 years old) 2 times a day, rivaroxaban 20 or 15 mg (for moderate renal impairment) 1 time a day, apixaban 5 or 2.5 mg (persons over 80 years of age with body weight <60 kg or serum creatinine ≥133 μmol/L) 2 times a day. In cases of severe renal impairment, all anticoagulants are contraindicated.
If there are contraindications to oral anticoagulants, ASA is prescribed at a dose of 325 mg/day for 48 hours, with a transition to 50–100 mg/day.
Evaluation of treatment effectiveness
In a patient who has suffered a TIA, the criteria for the effectiveness of treatment are:
- complete regression of neurological deficit;
- stabilization of vital functions and homeostasis;
- normalization of laboratory parameters;
- achieving target blood pressure values;
- restoration of blood flow, confirmed by the results of angiographic studies and ultrasound methods.
Complications and side effects of treatment
The most common complication of antithrombotic therapy is bleeding. When prescribing this therapy, it is necessary to find out the presence of potential sources of bleeding in the patient.
Risk factors for bleeding include:
- state of the blood coagulation system;
- age over 65 years;
- arterial hypertension;
- impaired renal and liver function;
- history of bleeding;
- history of peptic ulcer;
- alcohol or drug use;
- concomitant therapy (NSAIDs, corticosteroids);
- combined antithrombotic therapy.
But even with the risk of bleeding, in most cases the risk of developing a cerebral or myocardial infarction after a TIA is higher than the risk of bleeding.
Errors and unreasonable assignments
Gross errors are:
- refusal to hospitalize patients with TIA;
- prescribing antithrombotic therapy at the prehospital stage;
- administration of diuretics at the prehospital stage;
- lack of monitoring of vital signs and limited ability to provide adequate care to patients with TIA;
- the desire to lower blood pressure with moderate arterial hypertension.
FORECAST
With timely emergency hospitalization of a patient with TIA and adequate emergency treatment, the symptoms of TIA undergo a reverse development.
More than half of patients who have suffered a TIA remain at risk of developing cardiovascular complications, such as stroke, myocardial infarction, and vascular death.
The risk of developing a stroke within 3 months after a TIA ranges from 10 to 20%. In half of them, cerebral infarction occurs in the first 2 days after transient neurological symptoms.
To predict the risk of stroke after a TIA, the AVSD2 scale was developed (Tables 1, 2).
Almost 60% of TIA patients die within 5 years from other cardiovascular diseases.
After a TIA, ongoing therapy is recommended to prevent stroke and other cardiovascular diseases.
Management of patients who have suffered a TIA at the outpatient stage of treatment
Prevention of recurrent TIAs and strokes
Antithrombotic therapy continues almost lifelong, especially for patients who have a high risk of stroke according to the ABCD2 scale.
In patients with arterial hypertension, continuous antihypertensive therapy is indicated to prevent second TIAs and strokes. The target blood pressure level is determined individually, but it should not be lower than 130/80 mm. Hg with surgically unresolved unilateral stenosis of the carotid artery more than 70% of the vessel diameter and below 150 mm. Hg – with hemodynamically significant stenosis of the carotid arteries on both sides. The choice of antihypertensive drug is determined by the presence of concomitant and background diseases.
In case of atherothrombotic processes, especially in the presence of loose embologenic plaques in the carotid arteries, as well as against the background of lipidemia, the prescription of statins is indicated.
Lifestyle modification (giving up bad habits, dieting, rational physical activity).
To activate the processes of restoration of ischemic neurons, maintain endogenous protective mechanisms of nervous tissue, and stimulate neuroplasticity of the brain, it is advisable to prescribe neurotrophic drugs. One of the proven drugs in this group is Cerebrolysin, which contains fragments of neurotrophic factors, biologically active peptides and amino acids. The ECOMPASS study, using modern neuroimaging techniques (tractography/fMRI), demonstrated earlier and more complete disclosure of the potential of neuroplasticity in the combination therapy group (Cerebrolysin + rehabilitation measures). Several domestic randomized studies (Gusev E.I., Chukanova E.I.) have shown that the addition of Cerebrolysin to the standard treatment of patients with CCI (10 ml IV for 10 days every six months) or those who have had a stroke (20 ml IV /c for 10 days with a repeat course after six months) reduces the number of new/recurrent strokes and TIAs.
Prevention of cognitive impairment after TIA
Cognitive impairment (CI) is detected in almost 40% of patients who have suffered TIAs or “minor strokes”. CIs are more often detected in elderly and senile people, in whom the vascular process can stimulate the progression of subclinical neurodegeneration.
Currently, from the standpoint of evidence-based medicine, the role of regular physical activity in the prevention of CI in patients who have suffered a stroke or TIA is shown.
It is important to conduct cognitive training, diverse sensory stimulation, and maintain social contacts.
It is also advisable to include drug support for cognitive functions with neurometabolic drugs. It is desirable to have additional properties aimed at the pathogenetic mechanisms of cerebrovascular diseases and reducing the pathological impact of underlying diseases. From this standpoint, such drugs as deproteinized hemoderivate (Actovegin) and citicoline (Cerakson®) have proven themselves well. Both drugs provide modest but consistent improvements in memory and behavior in patients with CI.
The ARTEMIDA study showed a significant improvement in cognitive function in patients with ischemic stroke who took Actovegin for 6 months at a dose of 2000 mg intravenously for 3 weeks, followed by oral administration of 1200 mg/day for 21 weeks. The persistent therapeutic effect persisted for another 6 months after discontinuation of therapy.
Numerous clinical trials have proven the positive role of citicoline for patients in the acute period of stroke and during the rehabilitation stage. The IDEALE study noted the effectiveness and safety of oral citicoline (1 g/day) in elderly people with moderate vascular CI.
Prevention
To prevent the development of transient ischemic attacks, you should follow the recommendations of specialists:
- take prescribed medications in accordance with the prescribed prescription;
- control blood pressure levels;
- monitor blood cholesterol levels;
- give up bad habits: alcohol and nicotine addiction;
- regularly take medications that prevent the formation of blood clots;
- be regularly checked by your doctor.
To prevent a transient ischemic attack from having consequences, you should lead an active and healthy lifestyle:
- eat on time and often;
- eliminate or reduce the consumption of fatty, smoked and salty foods;
- play sports: swimming, therapeutic exercises;
- spend more time outdoors.
If you adhere to all of the above, the prognosis for full recovery will be positive.
Yusupov Hospital is located near the center of Moscow. Patients are accepted here around the clock. You can make an appointment and get advice from specialists by calling the clinic.