Sudden death
Definition
. Sudden cardiac death (SCD) is defined as: “natural death due to cardiac causes, characterized by sudden loss of consciousness within one hour of the onset of symptoms; the presence of heart disease may be known, but the timing and mechanism of death is unpredictable.” The key concepts guiding the definition of sudden death are that the cause is non-traumatic and that the onset of death is immediate and unpredictable. When considering the problem of sudden death within heart diseases, the word “cardiac” was introduced into the term.
Diet to prevent sudden death syndrome
Mom's diet while breastfeeding
- Efficacy: no data
- Timing: entire breastfeeding period
- Cost of products: 1400-1500 rubles per week
Sudden infant death often occurs in premature babies in families with low responsibility and material income, when the mother, due to circumstances, does not provide decent care for the baby, has various types of addictions and cannot find a permanent partner for life. Therefore, for the well-being of the child, it is necessary to exclude all of the above factors, take care of his sleep hygiene and establish a healthy life schedule - with walks and good nutrition for both mother and child, which can provide all nutrients, vitamins and minerals. Often, due to the mother’s lack of breast milk, it is necessary to resort to artificial feeding, the main thing is that it is of high quality and meets the needs of the child.
Causes
Epidemiology
. One of the leading causes of death in the adult population of developed countries is SCD due to coronary heart disease. In patients with sudden cardiovascular collapse, the rhythm of ventricular fibrillation is most often determined on the ECG (in 75-80% of cases), while bradyarrhythmias are the cause of SCD in a minimal number of patients. In 5-10% of cases of sudden cardiac death, patients do not have coronary heart disease or congestive heart failure. According to statistical data obtained annually in Western countries, the incidence of SCD varies from 0.6 – 1.28 per 1000 people per year. These studies only include data on those killed or resuscitated by emergency medical services; thus, official data are lower than the actual number of SCD cases in the general population.
Prevention of sudden cardiac death: general population and high-risk group. Among the adult population, the incidence of SCD is 1 in 1000 per year. Prophylactic interventions to reduce the risk of sudden cardiac death in this population appear to be neither practical nor cost-effective, since the costs include the remaining 999 per 1000 people per year who are not at risk for SCD. Thus, general principles of a healthy lifestyle are recommended in the general population.
Subgroups in which the annual risk of sudden cardiac death progressively increases are relatively few. It follows from this that promoting a healthy lifestyle among the population will naturally lead to a decrease in the number of patients with coronary heart disease, which in turn will reduce the number of cases of sudden cardiac death.
Additional examinations
The medical examination schedule for adolescents is determined by the state and provides for detailed examinations by at least six specialists of children in grades 1, 5, 7 and 9. Adolescent medical examination, especially that carried out during puberty, includes additional studies. So, a teenager must definitely visit a pediatrician, undergo basic tests, go to an ENT specialist, an ophthalmologist, an orthopedist, a dentist, a psychologist, and an endocrinologist. For the most part, pathological conditions in this area can significantly worsen the child’s health, forcing other organs and systems, incl. and cardiovascular, work literally to the limit.
Of course, as a preventative measure, you should review the child’s schedule and make it, where possible, less busy. It is also necessary to take care of the teenager’s nutrition. After all, as he grows up, he needs the right food, healthy and balanced, more than ever. It is imperative to choose vitamin therapy to compensate for the lack of useful microelements, which is quite common today. So, doctors say that many teenagers around the age of 14 experience anemia. And this is fatigue, lack of composure, and inattention, which are followed by bad grades at school, conflicts with teachers and parents. Teenagers are still children who also need attention and care.
Risk factors for sudden cardiac death in the population
| Non-modifiable risk factors | Modifiable risk factors |
| Age | Smoking |
| Male | Hypertension |
| Family history of coronary heart disease | Elevated LDL levels |
| Genetic factors | Diabetes |
| Obesity |
Prevention of SCD: recommendations of the European Society of Cardiology
The European Society of Cardiology Specialist Group on Sudden Cardiac Death presents recommendations aimed at reducing the incidence of SCD. The recommendations are presented in tables and distributed as follows:
Class I:
Reliable evidence and/or consensus among experts that a given procedure or treatment is appropriate, beneficial and effective.
Class II:
Conflicting evidence and/or differences in expert opinion about the benefit/effectiveness of a procedure or treatment.
Class IIa:
evidence and/or expert opinion for benefit/effectiveness predominates.
Class IIb
: Benefit/effectiveness is not well supported by evidence and/or expert opinion.
In these guidelines, the terms “primary” and “secondary” prevention are used primarily in the context of ventricular arrhythmia. Therapy prescribed to prevent the development of sustained ventricular arrhythmias in patients without a history of episodes of life-threatening ventricular arrhythmias, but classified as at high risk for their development, refers to “primary” prevention. The therapy recommended for patients with cardiac arrest and syncope/hypotension secondary to paroxysmal ventricular tachycardia is “secondary” prevention.
I. Myocardial infarction and heart failure
A. Risk stratification
Both non-invasive and invasive tests are used to determine the risk of SCD in patients with a history of myocardial infarction.
Risk stratification in patients who have had myocardial infarction
with/without development of HF
| Class | I | IIa | IIb |
| Demographic variability LVEF HR or BR sensitivity LV volume | ES unstable VT resting heart rate | Late potentials EPI Dynamics h. T Patency of the infarct-dependent artery |
LVEF – left ventricular ejection fraction; HR – rhythm variability
BR – baroreflex; ES – extrasystole; VT – ventricular tachycardia
HR – heart rate; h. T – T wave
B. Primary and secondary prevention of SCD in patients with a history of MI
Sudden cardiac death occurs most often among patients who have had a myocardial infarction. In this group, primary prevention includes drug treatment with beta blockers, aspirin, ACE inhibitors and cholesterol-lowering drugs. In patients with documented sustained VT or VF, the alternative is an implantable cardioverter-defibrillator (ICD) or amiodarone, and in selected cases, ablation or surgery. In patients with a history of myocardial infarction, a decrease in LVEF less than or equal to 40% (less than or equal to 5%) and clinically symptomatic paroxysms of non-sustained VT, or induced sustained or non-sustained VT by programmed electrical stimulation (EPS), the recommended treatment is CD implantation. For secondary prevention of SCD, the use of CD is recommended for those resuscitated after VF and patients with hemodynamically symptomatic VT paroxysms.
Primary prevention in patients who have had a myocardial infarction with/without the development of HF
| Class | I | IIa | IIb |
| History of MI | Beta blockers ACE inhibitors Cholesterol-lowering drugs Aspirin | Polyunsaturated fatty acids Amiodarone | |
| MI + LV dysfunction | Beta blockers ACE inhibitors Aldosterone receptor blockers | Amiodarone | |
| Hemodynamically asymptomatic VTs | Amiodarone Beta blockers | CD Ablation Surgical treatment | |
| LVEF less than or equal to 40% + paroxysms of non-sustained VT + inducible sustained VT with EPI | KD |
Secondary prevention in patients who have had a myocardial infarction with/without the development of HF
| Class | I | IIa | IIb |
| VF | KD | ||
| Hemodynamically symptomatic sustained VT | KD | Amiodarone Beta blockers |
II. Cardiomyopathies
Hypertrophic cardiomyopathy (HCM)
HCM is a relatively common cardiac disorder (incidence in adults approximately 1:500) in which sudden cardiac death is the most likely outcome at any age, but is most common in young, often asymptomatic patients. Implantation of a CD for the prevention of sudden cardiac death is strongly justified in patients who survive cardiac arrest (secondary prevention). Prophylactic use of KD is also possible in patients with two or more risk factors.
Hypertrophic cardiomyopathy
| Class | I | IIa | IIb |
| Risk stratification | Sustained VT VF | Family history of SCD Syncope LV hypertrophy (VSD greater than cm) Unsustained VT Hypotension during exercise stress test | High risk of mutations |
| Primary prevention | KD | Amiodarone | |
| Secondary prevention | KD |
VSD – thickness of the interventricular septum
Arrhythmogenic right ventricular dysplasia (ARVD)
ARVD is one of the main causes of sudden cardiac death in the “pre-coronary” age group. Although the predisposing factors for SCD have not yet been sufficiently studied in large prospective studies, sudden cardiac death occurs more often in patients with significant changes in the right ventricle, as well as in those with LV involvement. In those resuscitated after SCD (secondary prevention), in patients with sustained VT and ineffective antiarrhythmic therapy, and in high-risk patients with documented paroxysms of VT, the most adequate treatment is CD implantation.
Arrhythmogenic right ventricular dysplasia
| Class | I | IIa | IIb |
| Risk stratification | Sustained VT/VF Dilation of the RV RV dysfunction Inducible VT/VF with EPI | Family history of SCD Late potentials + LV dysfunction VT Inducible VT/VF with EPS | |
| Primary prevention | KD | Antiarrhythmic drugs | |
| Secondary prevention | KD |
RV – right ventricle; EPI – electrophysiological study
Dilated cardiomyopathy (DCM)
SCD is one of the most common mechanisms of death in DCM, especially in the early stages of the disease. Ejection fraction (EF) has been shown to be the most accurate predictor of outcome for both sudden cardiac death and death in advanced HF. The frequency of syncopal episodes is also considered one of the reliable risk factors for sudden cardiac death.
General therapeutic strategies aimed at reducing the risk of SCD in patients with DCM include the use of ACE inhibitors, beta blockers and aldosterone receptor antagonists, while amiodarone and CD implantation are used in individual cases. Several studies examining the role of antiarrhythmic drugs in patients with DCM have provided evidence (not statistically proven) that drug treatment recommended for patients who have had an MI with development of HF is equally effective in patients with DCM. The use of CDs for secondary prevention is considered acceptable; implantation of CDs is also recommended in high-risk patients for the primary prevention of sudden cardiac death.
Dilated cardiomyopathy
Class
| I | IIa | IIb | |
| Risk stratification | Sustained VT VF | Syncopations | Decreased EF Unsustained VT |
| Primary prevention | ACE inhibitors Beta blockers | KD Aldosterone receptor blockers | Amiodarone |
| Secondary prevention | KD ACE inhibitors Beta blockers | Aldosterone receptor blockers | Amiodarone |
Weak children
Modern children have a special way of life compared to past generations. On the one hand, they have more opportunities, because... they have access to global sources of information, more clubs and hobbies, but on the other hand, they go out less, communicate less often with peers, and eat poorly.
In addition, medical progress also contributes to the deterioration of children’s health. Indeed, today, young mothers often give birth at very early stages. Doctors have learned how to care for such babies: they can even grow babies born weighing 1 kg! Over time, these kids catch up with their peers, but they still remain quite fragile, and they need to be approached with special attention: they should be examined by doctors more often, and not ignore even seemingly harmless health problems. Naturally, you shouldn’t overload them. Also, various infections pose a separate danger to the fragile bodies of modern teenagers. Due to the mutation of viruses and widespread parental self-medication, even common colds can be much more difficult for children to tolerate. Doctors are especially concerned about infections when the symptoms include only fever and nothing more. All this, naturally, greatly weakens the immune forces of the child’s body.
And we shouldn’t forget about the period of hormonal changes, which has shifted today, and children begin growing up earlier. And this also becomes a serious test for a fragile organism.
Article on the topic
Evgeniy Yamburg: There are almost no healthy children left
III. Genetic pathology of ion channels
QT prolongation
Long QT syndrome is associated with a high risk of sudden cardiac death. Risk stratification is mainly based on the presence of syncope, Torsades de Pointe (VT) and a history of cardiac arrest. Primary prevention of SCD is generally based on treatment with beta blockers. CD implantation is recommended for secondary prevention, as well as in patients with VT/VF with a history of adequate treatment with beta blockers.
QT prolongation
| Class | I | IIa | IIb |
| Risk stratification | Torsade de pointes/VF/cardiac arrest Syncope Jervell–Lange-Nielsen syndrome QT prolongation | QT greater than 600 ms Development of VT/VF in childhood Prolongation of QT + AV block Macroscopically dynamic T waves Female gender Postpartum period | Family history of SCD Increased QT interval dispersion |
| Primary prevention | Avoid drugs that prolong the QT interval Beta blockers Avoid strenuous exercise | Sympathetic denervation of the LV pacemaker | |
| Secondary prevention | KD + beta blockers + avoid drugs that prolong the QT interval Avoid intense exercise |
ECS - electrical pacemaker
Brugada syndrome
Diagnosis of Brugada syndrome (BS) is based on the presence of spontaneous or inducible ST segment elevation in leads V1-V with or without right bundle branch block (RBBB). Risk stratification is still poorly defined, and the role of EPS in identifying patients with high-risk factors is debated. In survivors of cardiac arrest, CD implantation is recommended. Prophylactic use of KD in high-risk populations is strongly recommended, but this approach is limited by the lack of clearly defined risk criteria.
Brugada syndrome
| Class | I | IIa | IIb |
| Risk stratification | Sustained VT VF | Syncope Family history of SCD | Inducible VT/VF during EPI |
| Primary prevention | CD in patients with syncope/VT | KD in asymptomatic patients with VT induced by EPI | |
| Secondary prevention | KD |
Catecholaminergic polymorphic ventricular tachycardia
To date, there is no precise definition of catecholaminergic polymorphic ventricular tachycardia (CPVT), since large-scale studies are not possible. This disease is associated with a high risk of sudden cardiac death at a young age, but criteria for stratification are lacking. Prevention of sudden cardiac death is based on the use of beta blockers; KDs are recommended for secondary prevention, since the significance of KDs for primary prevention has not been determined.
Catecholaminergic polymorphic ventricular tachycardia
| Class | I | IIa | IIb |
| Risk stratification | VF | Family history of SCD Unsustained VT/syncope in childhood | Syncopations |
| Primary prevention | Beta blockers | KD | |
| Secondary prevention | KD + beta blockers | Beta blockers |
IV. Valve pathology
Aortic stenosis
Among patients whose cause of death is aortic stenosis (AS), about 20% are sudden cardiac death. In the absence of symptoms, the survival rate of patients with AS is high even without valve replacement. The prognostic value of various hemodynamic and electrophysiological studies is limited. Asymptomatic patients with hemodynamically severe aortic stenosis should be under constant observation and, if symptoms develop, undergo immediate surgery. In patients with documented sustained ventricular tachycardia, cardiac implantation should be considered.
Aortic stenosis
| Class | I | IIa | IIb |
| Risk stratification | Syncope Angina | VT, including those induced by EPS Decreased exercise tolerance | Significant stenosis |
| Primary prevention | Surgery | Amiodarone | |
| Secondary prevention | KD |
Mitral valve prolapse
Mitral valve prolapse (MVP) generally has a favorable prognosis; There are suggestions about the risk of sudden cardiac death, but there is no evidence. Most cases of SCD are described in patients who have previously suffered syncope or cardiac arrest, a family history of SCD at a young age, with severe prolapse or myxomatous changes in the mitral valve leaflets. For patients surviving cardiac arrest, CD implantation is recommended.
Mitral valve prolapse
Class
| I | IIa | IIb | |
| Risk stratification | Sustained VT VF | Family history of SCD Severe prolapse or myxomatous changes in the leaflets | QT prolongation Frequent/group ES Inducible VT/VF with EPS Mitral valve regurgitation Late potentials |
| Primary prevention | |||
| Secondary prevention | KD |
Results and discussion
It has been established that in the structure of VS, diseases of the cardiovascular system (CVS) occupy a leading place and account for an average of 74% in Omsk (Table 1).
Table 1. Indicators V.S. for 2005-2014 in Omsk
In Moscow, the average mortality rate from cardiovascular diseases also occupies a leading position and amounts to 79.19% (Table 2).
Table 2. Indicators V.S. for 2005-2014 in Moscow
From the data in table. 1 and 2 it can be seen that over the last decade, diseases of the circulatory system have taken first place among other causes of VS.
Analysis of VS cases by gender revealed a predominance of deaths among males. In the age group under 39 years of age, men accounted for 78% of all cases of VS, while in the age group over 40 years of age these figures were 57% for men and 43% for women, and by the age of 60 years and older, gender differences were almost equal to the predominance of numbers among women (Table 3).
Table 3. Sex and age characteristics of aircraft
The second place in the structure of the armed forces in Omsk is occupied by respiratory diseases - 9% and in Moscow - 6%. Mortality rates for diseases of the gastrointestinal tract are stable throughout the entire period and amount to 4% in both cities. Diseases of the central nervous system account for from 1.2 to 3% in different periods. In both cities, the indicator of BC from cancer pathology attracts attention. It is characterized by progressive growth over 10 years. In Moscow, these indicators increased 2.2 times (Table 4).
Table 4. Indicators V.S. from oncological pathology (according to the BSME of the Moscow Department of Health)
In the group of infectious diseases, one or another form of tuberculosis with complications, in some cases undiagnosed during life, was noted as the main cause of death. As a rule, this cause of VS was observed in a group of people leading an asocial lifestyle, with varying degrees of signs of alimentary cachexia and organ pathology reflecting chronic alcohol intoxication.
Thus, the structure of VS in both cities is characterized by stable mortality rates in the SCD group (74-79%) and an increase in VS from cancer in Moscow.
Of particular interest in forensic medical practice are cases of SCD in young people under the age of 35 years2, which raise controversial issues on the part of relatives, loved ones and law enforcement agencies, due to the lack of any clinical data on intravital medical observation or referral to doctors. With the usual macro- and microscopic examination of the corpses of such persons, pathological changes in the heart and large vessels are practically absent or, as a rule, insignificant.
In the group under 35 years of age, 1914 such cases were selected and studied over a 10-year period. The analysis showed that in this group, men make up 78% (Table 5), whose average age is 32-34 years, i.e., the category of working, economically promising and reproductive age.
Table 5. Indicators V.S. persons in the age group up to 35 years
The frequency of VS in young people from the entire population of deaths ranged from 15 to 15.3%.
During 2005 and 2014, the structure of causes of death in the study group also changed, which made it possible to establish certain patterns (Table 6).
Table 6. Comparative analysis of the causes of SCD among people under 35 years of age
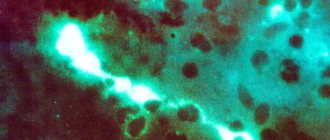
As can be seen from the data in table. 6, the rates of SCD from cardiomyopathy, the form of which is determined by a forensic expert during an autopsy based on morphological signs (dilated, hypertrophic, etc.), have increased significantly. An analysis of all cases in which a diagnosis of cardiomyopathy (CM) was made allowed us to identify a unified approach to the diagnosis of this pathology, reflecting the presence of diagnostic criteria: cardiac hypertrophy (heart weight more than 360 g), expansion of the cavities, flabbiness, dullness of the myocardium, absence of atherosclerotic vascular lesions, valvular pathology, as well as the presence of pathohistological signs: atrophy of cardiomyocytes, their uneven hypertrophy, severe myocardial lipomatosis, lipofuscinosis, myocytolysis, perivascular cardiosclerosis, endocardial fibrosis (Fig. 1). The main terminal symptom complex in cardiomyopathy is arrhythmia, since during life such individuals exhibit a prolonged RR interval, conduction disturbances, and various forms of arrhythmias (ventricular extrasystoles, paroxysmal tachycardias) [21, 22]. In the presence of a provoking factor (physical stress), acute cardiovascular failure with symptoms of pulmonary edema quickly develops. According to BUZ BSME D.Z. Moscow, mortality from cardiomyopathy has increased significantly over the past 10 years. The growth of this pathology may be due to the increased consumption in the group of adolescents (13 years old) and young men under 23 years of age of low-alcohol drinks (beer), the mechanism of damaging action of which is expressed in the disruption of energy and metabolic processes in the myocardium and in the direct toxic effect of cobalt on cardiomyocytes.
Rice. 1. Cardiomyopathy. a — myocardial lipomatosis with dilated cardiomyopathy; b — lipofuscinosis. Hematoxylin and eosin staining.
In the group of young people, 57% of the deceased, especially those under the age of 29, showed external and internal signs of systemic pathology - connective tissue dysplasia (CTD). Data obtained in recent years on the diagnosis of pathological conditions and diseases associated with CTD have made it possible to consider this pathology as one of the risk factors for VS among young people. Many works devoted to an in-depth study of the functional state of the myocardium and central hemodynamics in CTD have made it possible to formulate the statement that the pathology of the cardiovascular system in people with CTD is the main one, and cardiovascular disorders are the leading causes of shortened life of patients [23, 24].
The search for signs of DST allows one to identify the following large and small biological signs during an external examination of a corpse [25]:
1) asthenic type of constitution;
2) tall;
3) flat, narrow, long chest;
4) poor development of the subcutaneous tissue;
5) the presence of pathology of the sternum (funnel-shaped);
6) pathology of the spine (scoliosis, lordosis, combined forms);
7) skin syndrome - the presence of stretch marks, thin, pale, “marbled” skin;
 "blue sclera" syndrome;
"blue sclera" syndrome;
9) fused earlobe;
10) diastema between the first teeth, crowding, irregular tooth growth, Gothic palate;
11) curvature of the lower extremities (X- and O-shaped shins);
12) all types of flat feet (longitudinal, transverse); hallux valgus;
13) the second toe is larger than the first;
14) sandal-shaped gap (between the 1st and 2nd toes)
The presence of 1-2, 3 or more large external signs allows us to consider this pathology as a pre-existing onset of VS, since external signs indicate the presence of DST, which forms cardiovascular syndrome, dysplastic heart syndrome with metabolic disorders, as well as other syndromes: vascular, thoracodiaphragmatic, immunological .
The pathology of the cardiovascular system in persons with CTD is the main one and is diagnosed already during macroscopic examination.
1. Heart: violation of shape, size, position, changes in anatomical and topographic relationships; pathology of cavities and valve apparatus (mitral valve prolapse), endocardium, myocardium, pathology of the conduction system of the heart.
2. Coronary vessels: the presence of aneurysms, pathologically altered course of vessels, tortuosity, abnormal outlet.
3. Pathology of the aorta: hypoplasia, thinning, formation of aneurysms of the arch or ascending section.
4. Pathology of cerebral vessels: malformations, congenital aneurysms, thinning and rupture of the wall, pathological tortuosity, etc.
5. Pathology of the venous section: thrombosis, thrombophlebitis, pulmonary embolism as a cause of death.
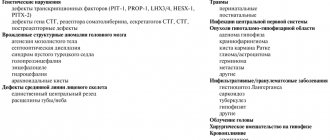
According to the literature [4, 5, 26], the immediate causes of death in persons with signs of CTD and the presence of cardiovascular syndrome were massive basal subarachnoid hemorrhages with a breakthrough into the ventricular system of the brain as a result of rupture of congenital aneurysms of the cerebral arteries; pulmonary embolism due to varicose veins; hemorrhagic shock due to rupture of a congenital aneurysm of the thoracic aorta; profuse bleeding caused by rupture of small arteries of internal organs (gastric, esophageal). The main links in the formation of vascular aneurysms in people with DST are a congenital defect of the muscular layer of the vascular wall, damage to the internal elastic membrane, changes in the collagen fibers of blood vessels and hemodynamic disorders that arise in the presence of provoking risk factors: physical activity, psycho-emotional stress, smoking, addiction to weak alcoholic drinks (Fig. 2).
Rice. 2. Rupture of an aneurysm of a vessel at the base of the brain with the development of basal subarachnoid hemorrhage.
Cases of the onset of VS during sports (during training, at competitions, during physical education classes at school or educational institution) in forensic medical practice are the most difficult, since, as a rule, boys or young men aged 16-23 die years, considered practically healthy [27-30]. According to our data, deaths were recorded in sports such as hockey, volleyball, basketball, as well as during exercise in the gym and sports halls. In such cases, sports activity as a psychophysical effort of increased intensity is a causative factor of VS. A.V. Smolensky and B.G. Lyubin [30] proposed to interpret VS in sports as follows: it is death that occurs within an hour from the moment of acute symptoms and coincides in time with sports activity (before the start, during competitions, immediately after the finish) in the absence of external causes, which themselves could have caused their own death. Consequently, the circumstances of death will always indicate the presence of a provoking factor - active physical activity of a sporting nature, and the development of terminal conditions will take place in the presence of witnesses. According to our data, the onset of VS in 42% of young people was detected before the arrival of the ambulance team, in 47% - after the arrival of medical workers and the provision of resuscitation measures, and in 11% death occurred without witnesses.
In our studies, death during physical activity (beginning of training, moment of loading, after loading) was recorded in 23 cases. The provoking factor for the onset of VS in 4 cases was physical activity of a sexual nature, in 7 cases - physical activity associated with lifting weights (lifting weights, transporting furniture, working in a summer cottage, etc.), in 12 cases - active sports (exercises physical education at a university, physical training in a military unit, death in the gym, death at sports competitions). Analysis of all these cases allowed us to consider physical activity as the main provoking factor in the onset of cardiac arrest. In all cases of VS during physical activity, the main pathological changes were identified in the heart, cardiac conduction system, as well as in the coronary vascular bed.
Pathomorphological changes in the heart, as a rule, reflected the main mechanism of SCD—arrhythmogenic. In a number of cases, emergency medical doctors who arrived before the onset of biological death recorded episodes of paroxysmal tachycardia on the ECG, the presence of groups of extrasystoles followed by atrial flutter and fibrillation, which allowed experts to identify and establish the main cause of death. The main types of fatal arrhythmias were ventricular arrhythmias (80% of cases), intraventricular or atrioventricular block. Asystole was much less common (about 20%) and reflected atrioventricular block or sinus node weakness. To date, there are no pathomorphological, biochemical and pathohistological markers that allow diagnosing the arrhythmic genesis of death, which in some cases leads to distortion and substitution of nosological verification of the cause of death in young people.
V. Pathology of the coronary arteries
Anomalous origin of the coronary arteries
SCD most often occurs in patients with an anomalous origin of the trunk of the left coronary artery from the right or non-coronary sinus of Valsalva. Therefore, special attention should be paid to young patients with chest pain similar in description to angina. Surgery is the most appropriate treatment option for patients at high risk of sudden cardiac death.
Anomalous origin of the coronary arteries
| Class | I | IIa | IIb |
| Risk stratification | VF | Young patients with angina or a positive stress test | |
| Primary prevention | Surgery | ||
| Secondary prevention | Surgery |
Myocardial bridges
The long-term prognosis for patients with the presence of myocardial bridges seems favorable, but in some cases this pathology can cause the development of tachyarrhythmias or sudden cardiac death. In symptomatic patients, quantitative coronary angiography, Doppler, and intravascular ultrasound are used to diagnose myocardial bridges. Drug treatment with beta blockers, surgery, angioplasty and coronary artery stenting are alternative treatments.
Myocardial bridges
| Class | I | IIa | IIb |
| Risk stratification | Symptomatic VT VF | Myocardial ischemia | |
| Primary prevention | Surgical treatment in patients with myocardial ischemia | Beta blockers | |
| Secondary prevention | Surgical treatment in patients with myocardial ischemia |
VI. Wolff-Parkinson-White syndrome (WPW)
According to modern research, in patients with WPW syndrome, the incidence of sudden cardiac death is 0.15% per year. The main cause of SCD is the transition of atrial fibrillation with a rapid ventricular response to ventricular fibrillation. Survivors of resuscitation for sudden cardiac death are typically characterized by the absence of symptoms, shortened RR intervals (less than 250 ms) during paroxysmal atrial fibrillation, and the presence of multiple or posteroseptal accessory pathways. Electrophysiological study with atrial excitation and determination of RR intervals between preexcited QRS complexes has high sensitivity, but specificity and significance in determining a positive predictor are limited. In patients at high risk for SCD, catheter ablation is recommended, particularly in those resuscitated from ventricular fibrillation or in patients with symptomatic episodes of atrial fibrillation with a rapid ventricular response.
Wolff-Parkinson-White syndrome
| Class | I | IIa | IIb |
| Risk stratification | less than 250 ms cycle duration in AF less than 270 ms anterograde refractory period of additional pathways Multiple additional pathways | Cessation of pre-excitation during treatment with ajmaline | |
| Primary prevention | Ablation for atrial fibrillation and the presence of rapid conduction through accessory pathways | Ablation in asymptomatic patients with – family history of SCD – athletes | Amiodarone Antiarrhythmic drugs classes Ia and Ic |
| Secondary prevention | Ablation |
Pathogenesis
Children commonly have abnormalities in serotonin , which is thought to impair the ability to regulate arousal and breathing normally, particularly in potentially life-threatening situations such as sleep and turning the baby onto his or her stomach. In addition, changes in the polymorphism of anti-inflammatory cytokines and reduced mandibular size are determinants of death. Another chain of mechanisms that causes sudden cessation of breathing is associated with the process of accumulation of high concentrations of carbon dioxide and insufficient blood oxygenation.
In general, there are several theories of the development of thanatogenesis mechanisms - respiratory, cardiac and metabolic.
VII. Bradyarrhythmias
It has been established that bradyarrhythmias are the cause of sudden cardiac death in 15-20% of cases. Risk factors for bradyarrhythmic death include high-degree AV block with intraventricular conduction disturbances, but in the presence of structural changes in the heart, these factors may predispose to the development of tachyarrhythmias. Pacing is the treatment of choice in high-risk patients with bradyarrhythmia: it relieves symptoms and may reduce mortality.
Risk stratification for cardiac conduction disorders
| Class | I | IIa | IIb |
| Profound AV block | AV block III degree AV block II degree, type II Syncope Combination of heart disease with CHF | ||
| Congenital AV block of the third degree | Syncope QT prolongation Congenital heart disease | ||
| Chronic two- or three-fascicle blockade | Combination of heart disease with CHF | Syncope Conduction from the Hiss bundle to the ventricles 100 ms (HV interval 100 ms) Intraventricular blocks Blocks induced during EPI |
Out-of-hospital resuscitation
Survival after cardiac arrest varies from 5% to 60% depending on the characteristics of the cardiac arrest (ie, cardiac etiology or not; verified or not; ventricular fibrillation or not). The outcome of cardiopulmonary resuscitation (CPR) is influenced not only by the success of its implementation, but also by the patient’s condition before the start of CPR.
It is now generally accepted that time to electrical defibrillation is the single most significant determinant of survival after cardiac arrest.
The instructions for the automatic external defibrillator allow defibrillation in cases of out-of-hospital ventricular fibrillation or ventricular tachycardia to people of non-medical professions, often many minutes before the arrival of the ambulance team. This strategy is known in the West as “first responder defibrillation,” based on the principle of mutual aid.
What to do if your baby stops breathing?
It is necessary to stimulate the respiratory center. To do this, take the child in your arms and shake him, then gently massage his arms, feet, earlobes and vigorously run your fingers along the spine. As a rule, such actions are enough for the child to wake up.
If this does not happen, start giving the baby artificial respiration, and if there is no pulse, then chest compressions. However, in order to carry out all actions correctly, it is advisable that you acquire the necessary skills for this during pregnancy or earlier, when you were planning to become a mother.
In addition, as soon as you begin to help your baby, one of your relatives should call an ambulance so that the doctors can arrive on time.