Community-acquired pneumonia is an infectious disease characterized by an inflammatory process in the lungs. The disease most often develops during influenza epidemics and acute respiratory viral infections. Patients with mild pneumonia can be treated on an outpatient basis. In cases of moderate to severe pneumonia, they are hospitalized in a therapy clinic.
The Yusupov Hospital employs professors and doctors of the highest category, who are leading experts in the field of pulmonology. To diagnose the disease, innovative examination methods are used to identify the pathogen, the localization and extent of the pathological process, and the severity of the disease. Doctors take an individual approach to the treatment of each patient, prescribing the most effective modern drugs with minimal side effects.
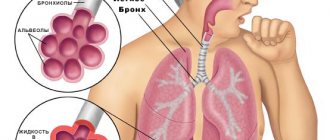
What is pneumonia
— This is a disease of the lower respiratory tract, in particular the alveoli.
This is where gas exchange occurs during breathing. Depending on the causative agent, pneumonia is divided into bacterial and viral. Initially, we only talked about bacterial pneumonia for many years. Viral ones were rare. Everything changed after 2009, when the so-called swine flu pandemic occurred. Viral pneumonia has become a fairly common complication of the disease.
Bacterial pneumonia can also be a complication of influenza or other viral illness. Viral disease is characterized by a rapid onset and a sharp onset of respiratory failure. The prognosis is poor because large areas of the lungs are affected at once.
If we are talking about viral pneumonia associated with COVID-19, then its course resembles that of swine flu.
Viral pneumonia is a manifestation of the severe course of coronavirus infection COVID-19. Sometimes microbial flora is also added, then we talk about a bacterial-viral infection.
In the Altai Territory, the number of pneumonias has always been higher than in the European part of Russia and even compared to its neighbors in the Siberian District. It is impossible to explain this by climate or standard of living.
Regional clinical hospital for emergency medical care.
Anna Zaikova.
Publications in the media
Pneumonia is a group of acute infectious (mainly bacterial) diseases, different in etiology, pathogenesis and morphological characteristics, characterized by focal damage to the respiratory parts of the lungs with the obligatory presence of intra-alveolar exudation. Bacterial pneumonia is pneumonia of bacterial etiology. Classification • According to the conditions in which the disease developed •• Community-acquired pneumonia - acquired outside a medical institution (synonyms: home, outpatient) •• Nosocomial pneumonia - acquired in a medical institution (synonyms: hospital, nosocomial) •• Aspiration pneumonia •• Pneumonia in individuals with severe immune defects (congenital immunodeficiency, HIV infection, iatrogenic immunosuppression, etc.) • Along the course •• Mild - does not require hospitalization •• Severe - hospitalization is required.
Incidence • 236.2 cases per 100,000 adolescents 15–17 years of age • 522.8 cases per 100,000 population under 14 years of age • Community-acquired pneumonia - 1,200 cases per 100,000 population per year • Hospital-acquired pneumonia - 800 cases per 100,000 hospitalizations per year . The predominant age is under 20 and over 60 years. Predominant gender - no significant differences were found by gender. Etiology • Streptococcus pneumoniae - most common (30-50%) • Haemophilus influenzae (10-20%) • Atypical pathogens - Chlamidophila pneumoniae, Mycoplasma pneumoniae, Legionella pneumophila (8-25%) • Typical but rare (3-5 %) include Staphylococcus aureus, Klebsiella pneumoniae (less commonly other enterobacteria) • Moraxella catarrhalis (Branhamella catarrhalis) • Most often, community-acquired pneumonia is caused by pneumococci (their sensitivity to penicillin in many countries is significantly reduced) • In very rare cases of community-acquired pneumonia - Pseudomonas aeruginosa (with cystic fibrosis, bronchiectasis), in persons with severe immunodeficiency - Pneumocystis carinii • Escherichia coli • Anaerobic microorganisms • Atypical pneumonia.
Risk factors • Recent acute respiratory viral infection • Renal failure • Cardiovascular diseases • COPD • Immunodeficiency conditions: diabetes, chronic alcoholism, AIDS, malignant neoplasms • Dysbiosis • Risk factors for hospital-acquired pneumonia •• Mechanical ventilation •• Early postoperative period •• Dysbacteriosis • Risk factors aspiration pneumonia •• Impaired consciousness •• Convulsive seizures •• Diseases of the central nervous system •• Anesthesia •• Reflux esophagitis. Pathogenesis . Main pathogenetic mechanisms • Aspiration of oropharyngeal secretions (the main route of infection) • Inhalation of an aerosol containing microorganisms • Hematogenous spread of pathogens from an extrapulmonary source of infection (for example, with endocarditis, with septic thrombophlebitis) • Direct spread of infection from neighboring affected organs (for example, with liver abscess ) or as a result of injury and infection of the chest organs. Pathomorphology . Segmental, lobar or multifocal peribronchial compaction with stages of red (intra-alveolar exudation and erythrocyte diapedesis) and then gray (fibrous organization of intra-alveolar exudate) hepatization.
Clinical picture. • Complaints •• Cough with mucopurulent (sometimes “rusty”) sputum •• Chest pain when breathing (with concomitant pleurisy) •• Shortness of breath •• Weakness, fatigue •• Night sweats. • Intoxication syndrome •• Fever •• Tachycardia •• Tachypnea •• Hyperhidrosis •• Myalgia •• Headaches •• Anorexia. • Objective examination data •• Cyanosis •• Percussion: dullness of percussion sound caused by infiltration or pleural effusion •• Auscultation ••• Moist fine rales and/or crepitus (heard on inspiration) ••• With extensive infiltration or pleural effusion, breathing is weakened • •• Pleural friction noise with dry pleurisy •• In severe cases, meningeal signs and disturbances of consciousness (for example, disorientation and anxiety) may appear •• In 20% of cases, objective signs may be mild or absent. Laboratory tests • Leukocytosis with a shift of the leukocyte formula to the left •• Leukocytosis more than 10-12109/l is characteristic of a bacterial infection •• Values more than 25109/l or leukopenia below 3109/l indicate a poor prognosis • Hyponatremia • Increased activity transaminases • Bacteriological blood test to identify the pathogen (positive result in 20–30% of patients with community-acquired pneumonia, especially before the start of antibacterial therapy) • At the height of active inflammation and intoxication, protein may appear in the urine • Bacteriological and bacterioscopic examination of sputum: microscopy of a stained smear according to Gram, and culture of sputum obtained during deep coughing • Bacteriological examination of material obtained during bronchoalveolar lavage and thoracentesis • In the presence of pleural effusion and pleural puncture - examination of pleural fluid: counting leukocytes with a leukocyte formula, determination of pH, protein content, LDH, microscopy of a Gram-stained smear, culture for aerobic, anaerobic bacteria and mycobacteria • Study of the immune status of persons with suspected immunodeficiency. Special studies • Chest X-ray is a mandatory research method for pneumonia, allowing to visualize areas of infiltration of lung tissue (take into account the shape, size and location), assess the dynamics of the process •• The prevalence of infiltration, the presence of pleural effusion and signs of destruction of lung tissue reflect the severity of the disease and significantly influence the nature of treatment • CT scan of the lungs is performed if destruction or neoplasm is suspected • Fiberoptic bronchoscopy with microbiological and cytological examination of the biopsy specimen - if tuberculosis and tumor diseases are suspected • FVD study - for differential diagnosis with respiratory distress syndrome • With extensive infiltration, massive pleural effusion, In the presence of COPD, it is advisable to evaluate arterial blood gases, which may be the basis for hospitalization and low-flow oxygenation • The study of capillary blood gases is not very informative.
Diagnostic tactics , diagnostic algorithms. The diagnosis of pneumonia is considered definite if the patient has radiologically confirmed infiltration of the lung tissue and at least two of the following signs: • acute febrile onset of the disease (body temperature more than 38 ° C); • cough with sputum; • listening to local crepitus, shortening of percussion sound; • leukocytosis more than 10109/l and/or shift of the leukocyte formula to the left more than 10%. Differential diagnosis • Pneumonia of non-bacterial etiology (viral, fungal, caused by protozoa) • Tuberculosis (examination of at least three sputum smears, Ziehl-Neelsen stained, sputum culture, PCR diagnosis) • Pulmonary infarction (PE) • Bronchiolitis obliterans • Pulmonary contusion • Pulmonary vasculitis • Acute sarcoidosis • Exogenous allergic alveolitis • Eosinophilic infiltrate • Lung tumors • Other conditions that can cause infiltration syndrome on chest x-ray.
TREATMENT Diet. A complete diet with sufficient protein and a high content of vitamins A, C, group B • Limiting carbohydrates to 200–250 g/day, table salt to 4–6 g/day and increasing the proportion of dairy products • Introducing a sufficient amount of fluid (1500–1700 ml/day) • Saturation of the diet with foods rich in vitamin P (aronia, rose hips, black currants, lemon) • Inclusion of foods rich in B vitamins (meat, fish, yeast, wheat bran decoction) prevents the suppression of intestinal microflora by antibiotics • Foods rich in nicotinic acid • Foods rich in vitamins A and -carotene (carrots, red vegetables and fruits) promote the regeneration of the epithelium of the respiratory tract. Fruit and vegetable juices are recommended • Food is given in crushed and liquid form, meals are taken 6-7 times a day • Energy value is from 1600 kcal/day, increasing as recovery progresses to 2800 kcal/day. Indications for hospitalization • Age under 16 or over 60 years • Concomitant diseases (for example, diseases of the bronchopulmonary system or cardiovascular system, circulatory failure IIa and higher, diabetes, thyrotoxicosis) • Physical signs: respiratory rate more than 30 per minute, diastolic blood pressure less than 90 mm Hg. Art., pulse more than 125 per minute, body temperature less than 35 °C or 40 °C or more, disturbances of consciousness • Laboratory data: the number of leukocytes in the peripheral blood is less than 4.0109/l or more than 30.0109/l , arterial blood oxygen saturation is less than 92% (according to pulse oximetry), paO2 is less than 60 mm Hg. and/or paCO2 more than 50 mm Hg. when breathing room air, serum creatinine content is higher than 176.7 µmol/l or urea nitrogen is higher than 7.0 mmol/l, Ht is less than 30% or Hb content is lower than 90 g/l • X-ray data: pneumonic infiltration of more than one lobe, the presence of decay cavities, pleural effusion, rapid progression of focal infiltrative changes in the lungs (increase in the size of infiltration by more than 50% within 2 days) • Extrapulmonary foci of infection (meningitis, septic arthritis, etc.) • Sepsis or multiple organ failure with metabolic acidosis (pH <7.35), coagulopathy • Impossibility of adequate care and fulfillment of all medical prescriptions at home • Lack of effect from outpatient treatment for 3 days, long-term persistence of intoxication syndrome • Preference of the patient and/or his family members.
Drug therapy. The basis of treatment is antibacterial therapy. It begins from the moment of diagnosis, but after collecting material for bacterioscopic and bacteriological examination of sputum. At home, as well as in a hospital, in the first days of the disease (before receiving the results of bacteriological studies), drugs are selected empirically. After receiving the results of a bacteriological study, treatment is carried out taking into account the sensitivity of the pathogen to drugs •• Treatment of community-acquired pneumonia in an outpatient setting ••• Persons under 60 years of age without concomitant diseases are prescribed amoxicillin (500 mg 3 times / day) or amoxicillin + clavulanic acid, or macrolides ( spiramycin, clarithromycin, azithromycin, midecamycin, etc.), or pneumotropic fluoroquinolones (levofloxacin) ••• For non-severe pneumonia in patients over 60 years of age and/or with concomitant diseases, treatment with amoxicillin/clavulanate or cefuroxime is started; levofloxacin is an alternative ••• If it is impossible to take drugs orally, parenteral administration of ceftriaxone is used ••• The effect of treatment is assessed after 48–72 hours, primarily by reducing body temperature. In this regard, NSAIDs should not be used during this period without special indications. If the temperature and intoxication syndrome do not decrease, a change in antibiotic is indicated with a re-assessment of the advisability of hospitalizing the patient •••• If amoxicillin was used, switch to macrolides; if amoxicillin + clavulanic acid or cefuroxime were used, switch to levofloxacin; if macrolides were used, switch to amoxicillin + clavulanic acid or levofloxacin ••• Antibacterial therapy is stopped with stable normalization of temperature on the 3-4th day •• Treatment in a hospital ••• For mild pneumonia, therapy begins with intravenous administration of ampicillin (or amoxicillin/clavulanate, cefuroxime, cefotaxime or ceftriaxone) with switching to oral administration of drugs of the same group (stepped therapy) ••• In severe pneumonia, treatment begins with intravenous administration of a macrolide (erythromycin, spiramycin, clarithromycin) in combination with an intravenous β-lactam drug (amoxicillin/clavulanate, cefotaxime, ceftriaxone) •• • An alternative may be the intravenous administration of a combination of third-generation cephalosporins with early fluoroquinolones (ciprofloxacin, ofloxacin) or the intravenous administration of new fluoroquinolones (levofloxacin, moxifloxacin) •• Treatment of nosocomial pneumonia in general wards: prescribe IV amoxicillin + clavulanic acid, ampicillin / sulbactam or cephalosporins of II–III generations, alternatives are new fluoroquinolones (levofloxacin, moxifloxacin), carbapenems, cefoperazone + sulbactam, cefepime; in intensive care units and wards - carbapenems, cefepime or cefoperazone + sulbactam, ticarcillin + clavulanic acid, piperacillin / tazobactam •• In the treatment of aspiration pneumonia, intravenous forms of cephalosporins of III-IV generations, levofloxacin, moxifloxacin, ticarcillin + clavulanic acid, piperacillin / taz are recommended obactam , amoxicillin+clavulanic acid, ampicillin/sulbactam. For persons with periodontal diseases or alcoholism - a combination of III-IV generation cephalosporins with metronidazole or lincomycin •• In the treatment of pneumonia in patients with AIDS, intravenous combinations of co-trimoxazole with amoxicillin and itraconazole (or fluconazole) are recommended •• For destructive pneumonia (or abscess formation) they are used IV amoxicillin + clavulanic acid, ampicillin / sulbactam, cefoperazone + sulbactam or carbapenems, ticarcillin + clavulanic acid, piperacillin + sulbactam, combination of lincomycin with an aminoglycoside; combination of benzylpenicillin + metronidazole with a transition to the combination of amoxicillin + metronidazole orally (stepped therapy). The duration of therapy is 3–4 weeks or more.
• Tactics of antibacterial therapy after obtaining the results of bacteriological studies, if the sensitivity of microorganisms to antibiotics has not been determined •• For pneumococcal damage - benzylpenicillin 1-2 million units intramuscularly every 4 hours, erythromycin 500 mg every 6 hours, roxithromycin 150 mg 2 times a day or azithromycin 500 mg 1 time / day. For resistant strains - cefotaxime, ceftriaxone, imipenem + cilastatin •• For H. influenzae infection - co-trimoxazole 2 tablets every 12 hours. Reserve drugs: cephalosporins of the II and III generations (cefuroxime 0.25-1 g IV every 12 h, cefaclor 0.5–1 g orally every 6 hours), chloramphenicol 0.5–1 g every 6 hours, amoxicillin + clavulanic acid •• For Staphylococcus aureus lesions - oxacillin 6–10 g/day, first generation cephalosporins or clindamycin 600–800 mg IV every 6–8 hours. For resistant strains - vancomycin •• For Klebsiella lesions - aminoglycosides, third generation cephalosporins (cefotaxime 2 g IV every 6 hours, ceftazidime 2 g IV every 8 hours; ceftriaxone 2 g IV every 12 hours), fluoroquinolone derivatives (ciprofloxacin 500–750 mg 2 times / day), imipenem + cilastatin 1 g 2 times / day •• For Escherichia coli lesions - aminoglycosides, cephalosporins II and III generations. Alternative drugs - fluoroquinolone derivatives, imipenem + cilastatin, chloramphenicol •• For Pseudomonas aeruginosa lesions - a combination of aminoglycoside and carbenicillin or ceftazidime, azlocillin or imipenem + cilastatin •• For Enterococci lesions - a combination of ampicillin and gentamicin •• For Moraxella catarrhalis lesions - cefa II generation losporins or amoxicillin + clavulanic acid, co-trimoxazole, clarithromycin •• If Acinetobacter is affected - imipenem + cilastatin or aminoglycosides, co-trimoxazole. • Expectorants •• Agents that stimulate expectoration ••• Direct-acting drugs, for example potassium iodide ••• Reflex-action drugs, for example, thermopsis herb infusion, licorice root preparations, etc. •• Mucolytic drugs, for example acetylcysteine, trypsin, bromhexine, ambroxol. • Oxygen therapy for patients with cyanosis, hypoxia, shortness of breath.
Surgical treatment of pneumonia is not performed. The question of surgical intervention arises when an abscess forms, especially a chronic one, or when pneumonia is complicated by pleural empyema. Monitoring the effectiveness of treatment • Clinical indicators •• Fever •• Shortness of breath •• Cough • X-ray dynamics (lags behind clinical) • Bacteriological examination of sputum - if treatment is ineffective. Complications • Pleural effusion (complicated and uncomplicated) • Destruction/abscessation of lung tissue • Acute respiratory distress syndrome • Acute respiratory failure • Infectious-septic shock • Pleural empyema. • Secondary bacteremia, sepsis, focus of hematogenous dissemination • Pericarditis, myocarditis • Nephritis. Prevention • Prevention of aspiration in bedridden patients • Rational use of antibiotics • Annual influenza vaccination for people at high risk • Polyvalent pneumococcal vaccine (currently not available in Russia) is recommended for people over 65 years of age and children over 2 years of age with the following risk factors •• Dysfunction spleen or asplenia •• Lymphogranulomatosis •• Multiple myeloma •• Liver cirrhosis •• Chronic alcoholism •• Renal failure •• Immunodeficiency. Age characteristics • Children •• Focal-confluent nature of the lesion predominates •• In the clinical picture - acute onset, severe intoxication against the background of a weak (or absence) pain syndrome, pronounced auscultation pattern •• Dynamics against the background of antibacterial treatment - rapid positive effect •• High mortality in children under 1 year of age • Elderly and old people: morbidity and mortality are increased over the age of 70 years, especially with concomitant pathology or the presence of risk factors. Features for pregnant and lactating women • During pregnancy, the use of β-lactam antibiotics, macrolides, metronidazole is permissible; fluoroquinolones, tetracyclines, aminoglycosides, lincosamides, co-trimoxazole are contraindicated • When breastfeeding, penicillins, cephalosporins, azithromycin are acceptable with caution; macrolides, fluoroquinolones, carbapenems, tetracyclines, lincosamides, co-trimoxazole are not recommended. Course and prognosis • Depend on the severity of the course, the pathogen, the patient’s age, the time of initiation of treatment, the adequacy of initial therapy, the state of the immune system, concomitant diseases • Mortality from community-acquired pneumonia: 1–3% - among young previously healthy people, 15–30% - in older age groups with concomitant diseases.
ICD-10 • J13 Pneumonia caused by Streptococcus pneumoniae • J14 Pneumonia caused by Haemophilus influenzae [Afanasyev-Pfeiffer bacillus] • J15 Bacterial pneumonia, not elsewhere classified • J17.0* Pneumonia in bacterial diseases classified elsewhere
Can pneumonia occur separately from ARVI and influenza?
- Maybe. This is an infectious disease that is transmitted from person to person. Everyone in the body has a complex and multi-stage defense mechanism that does not allow viruses and bacteria to penetrate into the deep respiratory tract: microbes settle during aerodynamic filtration, on the mucous membranes, in the larynx, in the branches of the bronchi - so to speak, “at the bends”.
The bronchi also contain ciliated epithelium, which is in constant motion towards exit into the oral cavity. Mucus is secreted there, which carries the germs back. Plus the immune system works.
Pneumonia is not only a complication of viral diseases. It was during its study that, for example, they discovered legionella, which loves to live in air conditioners. In 1976, more than 200 military veterans attending an American Legion convention in Philadelphia fell ill. Several dozen later died from this previously unknown disease. There was just air conditioning there.
The massiveness of the dose and high virulence - infectiousness, in other words, played a role. This is exactly what we are seeing now with coronavirus. It itself is highly contagious and active, so the body, especially if it is weakened, cannot protect itself from it. Although it is known that about 20% of those infected are asymptomatic.
District hospital.
Dmitry Lyamzin.
What is the difference between community-acquired and hospital-acquired pneumonia?
— Hospital-acquired pneumonia occurs in people who are hospitalized with any disease. That is, a person is initially more weakened. Such pneumonia requires different treatment.
Nosocomial pathogens of pneumonia are found in every intensive care unit, in every intensive care unit, or simply in a department. They are quite difficult to fight. Maternity hospitals have the practice of completely closing for a month to completely “wash themselves out.” In theory, this should be done in all hospitals, but it is impossible to close, for example, the intensive care unit of a regional clinical hospital.
In community-acquired pneumonia, the causative agent is more clear and defined. The flu season is coming, and we know what type it will be, so we can immunize the population in advance. Microbes that cause community-acquired pneumonia have long been known and described. In 80% of cases it is pneumococcus. In adults they cause pneumonia, in children - meningitis, otitis, and sinusitis. The next most common are intracellular pathogens: Klebsiella, Mycoplasma, Legionella.
In this regard, it is easier to decide on initial therapy. Most often, treatment begins with an antibiotic that acts on pneumococcus; if after three days it does not help, we prescribe drugs against intracellular pathogens.
Community-acquired pneumonia may be milder than hospital-acquired pneumonia. There are even at-home treatment options.
Medicine. Hospital.
unsplash.com
Forecast
The mortality rate of patients with severe community-acquired pneumonia hospitalized in the ICU is high and ranges from 22 to 54%. An unfavorable prognosis may be due to the following factors:
- performing mechanical ventilation
- patient age 70 years or older
- bacteremia
- bilateral localization of pneumonia
- need for inotropic support
- sepsis
- P. aeruginosa infection
- ineffectiveness of initial (initial) antibiotic therapy
The fatality rate is high when community-acquired pneumonia is caused by Legionella spp., S. pneumoniae, P. aeruginosa, or Klebsiella pneumoniae.
How to treat pneumonia
— This is primarily antimicrobial therapy. Plus symptomatic treatment - mucolytics, bronchodilators. This is individual for each patient. General: antibiotics.
However, you need to understand that antibiotics do not work on the virus. That’s why we always say that if you have ARVI or influenza, you can’t “prescribe” these drugs to yourself. This way you will only weaken the immune system, and if the microbial component also joins, then the body’s reserves will be exhausted, and this can lead to more serious complications.
For pneumonia during swine flu, there were several antiviral drugs with proven effectiveness. Now, with coronavirus infection, it is quite difficult to decide on therapy, since experience in using certain medications is only being gained.
It’s good that the epidemic did not start here, we have the opportunity to use the developments of our Moscow colleagues, they regularly review methods. On October 1, we already had the eighth version of the methodological recommendations.
Doctors, hospital
unsplash
How is pneumonia diagnosed?
- A CT scan will show changes in the airways. Based on the severity of these changes, the detected pneumonia is divided into four types, from the mildest (CT-1) to the most severe (CT-4).
But in fact, computed tomography is far from the first place in clinical recommendations. Pneumonia has always been diagnosed using radiography and even fluorography, which will also show lesions in the lungs.
Medicine. Hospital.
unsplash.com
What are the dangers of pneumonia?
- Respiratory failure and generalization of the process - that is, sepsis. In addition to the lungs themselves, the heart, kidneys, and brain are also affected. There may be extensive pulmonary edema, infectious-toxic shock, multiple organ failure. This can ultimately be fatal.
If a person has suffered a mild form of pneumonia, then it is recommended to avoid hypothermia for a month. In the case of covid pneumonia with a large volume of lung damage, there is a high probability that respiratory failure will remain for a long time, maybe even forever.
This is due to the fact that so-called pneumosclerosis occurs when the lung tissue is replaced by connective tissue that is not capable of breathing. Such people complain of constant shortness of breath and the inability to endure intense physical activity.
People need long-term rehabilitation, including physical therapy. A diet high in proteins, vitamins, and fiber is required.
Sometimes the help of a psychotherapist is required, as we observe cognitive impairment due to hypoxia. Plus, many survivors of severe forms of COVID-19 may have a persistent fear of death.
Introduction
Community-acquired pneumonia (CAP) is one of the pressing problems of modern medicine, due to the high morbidity and mortality associated with this pathology. Thus, the annual incidence of CAP in Russia is 390–400 cases per 100 thousand population, and mortality is 17–18 cases per 100 thousand [1]. According to WHO, pneumonia and influenza are the 3rd leading causes of death, claiming more than 3 million lives annually. It is known that in young and middle-aged patients without concomitant diseases, the mortality rate is on average 1–3%, and in elderly patients with concomitant diseases, the mortality rate reaches 15–58% [1, 2]. Important factors for an unfavorable outcome in pneumonia are late seeking medical help, incorrect assessment of the patient’s condition and prognosis of the disease, as well as inadequate initial antibiotic therapy.