Pharmacological properties of the drug Novomix 30 flexpen
NovoMix 30 FlexPen is a two-phase suspension consisting of a mixture of insulin analogues: insulin aspart (an analogue of short-acting human insulin) and protamine-insulin aspart (an analogue of medium-acting human insulin). A decrease in blood glucose levels under the influence of insulin aspart occurs after it binds to insulin receptors, which promotes the uptake of glucose into muscle and fat cells and at the same time inhibits the release of glucose from the liver. NovoMix 30 FlexPen is a two-phase suspension containing 30% soluble insulin aspart. This ensures a faster onset of action compared to soluble human insulin and allows the drug to be administered immediately before meals (from 0 to 10 minutes). The crystalline phase (70%) consists of protamine insulin aspart, which has the same activity profile as human neutral protamine Hagedorn insulin (NPH). NovoMix 30 FlexPen begins to act 10–20 minutes after subcutaneous injection. The maximum effect is achieved 1–4 hours after administration. Duration of action is up to 24 hours. The level of glycosylated hemoglobin in patients with type I and II diabetes mellitus who were administered NovoMix 30 for 3 months is the same as when administered biphasic human insulin. When administered in equal molar doses, insulin aspart matches the activity of human insulin. In a clinical study, patients with type II diabetes mellitus (341 people), divided into groups according to a randomized principle, received only NovoMix 30 FlexPen, or NovoMix 30 FlexPen in combination with metformin, or metformin in combination with a sulfonylurea. After 16 weeks of treatment, the levels of glycosylated hemoglobin HbA1c in patients receiving NovoMix 30 in combination with metformin or metformin in combination with sulfonylurea were the same. In this study, 57% of patients had HbA1c levels above 9%. In these patients, combined treatment with NovoMix 30 FlexPen and metformin caused a more pronounced decrease in HbA1c levels compared to the combination of metformin and sulfonylurea. In a study, patients with type II diabetes whose glycemic control was ineffective with oral hypoglycemic agents were treated with NovoMix 30 twice daily (117 patients) or insulin glargine once daily (116 patients). After 28 weeks of treatment with NovoMix 30, accompanied by dose adjustment, HbA1c levels decreased by 2.8% (average HbA1c values at study entry = 9.7%). When treated with NovoMix 30, 66% of patients reached HbA1c levels below 7%, and 42% of patients reached levels below 6.5%; at the same time, the fasting plasma glucose concentration decreased by approximately 7 mmol/l (from 14.0 mmol/l before treatment to 7.1 mmol/l). Pharmacokinetics . In insulin aspart, the amino acid proline at position 28 of the B-chain of the insulin molecule is replaced by aspartic acid, which reduces the formation of hexamers formed in soluble human insulin preparations. In the soluble phase of NovoMix 30 FlexPen, the share of insulin aspart is 30% of total insulin. It is absorbed into the blood from subcutaneous tissue faster than soluble biphasic human insulin. The remaining 70% comes from the crystalline form of protamine insulin aspart, whose longer absorption rate is the same as that of human NPH insulin. The maximum concentration of insulin in the blood serum after administration of NovoMix 30 FlexPen is 50% higher, and the time to achieve it is half as short compared to biphasic human insulin 30. In healthy volunteers after subcutaneous administration of the drug NovoMix 30 at the rate of 0.20 U/kg body weight body, the maximum concentration of insulin aspart in the blood serum was achieved after 60 minutes and amounted to 140±32 pmol/l. The half-life of NovoMix 30, which reflects the rate of absorption of the protamine fraction, was 8–9 hours. The level of insulin in the blood serum returned to baseline 15–18 hours after subcutaneous administration. In patients with type II diabetes mellitus, the maximum concentration was reached 95 minutes after administration and remained above the initial concentration for at least 14 hours. Children and adolescents. The pharmacokinetics of NovoMix 30 FlexPen have not been studied in children and adolescents. However, the pharmacokinetics and pharmacodynamics of soluble insulin aspart were studied in children (6-12 years old) and adolescents (13-17 years old) with type 1 diabetes. It was rapidly absorbed in patients of both groups, and the time to reach maximum concentration was the same as in adults. At the same time, Cmax values in different groups differed significantly, which indicates the importance of individual selection of doses of insulin aspart. The pharmacokinetics of NovoMix 30 has not been studied in the elderly, children and patients with impaired renal or hepatic function.
The biphasic insulin preparation aspart 30/70 (insulin NovoMix 30, Novo Nordisk, Denmark) refers to biphasic insulin preparations containing fixed proportions of short-acting (ultra-short) and long-acting insulin. They are also called premixed drugs or ready-mixed insulin. The drug NovoMix 30 (biphasic insulin aspart, DIAsp) has been used in global clinical practice for more than 10 years, incl. and in Russia [1, 2]. This two-phase mixture consists of two components: a biosynthetic analogue of human insulin aspart (30%), which has an ultra-short action, and crystals of protaminated complexes of the same insulin aspart, which has a hypoglycemic effect of medium duration (70%). The first of the components acts primarily in the postprandial (after eating) period, the second controls the basal level of glycemia. A mixture of aspart and its protamine form is stable, while insulin aspart and human insulin NPH (neutral protamine Hagedorn) degrade upon prolonged contact. In addition, when mixed with protaminated aspart, the ultra-short action of aspart is completely preserved [3]. Now we can safely say that NovoMix 30 is one of the most studied insulin drugs, which has demonstrated high efficiency and safety both in numerous randomized clinical trials and in large observational programs.
Biphasic insulin preparations were created primarily for the treatment of type 2 diabetes mellitus (T2DM), although there is experience with the use of NovoMix 30 in T1DM [4].
It is T2DM that makes up a rapidly growing cohort of patients that has forced the world community to talk about an “epidemic of non-communicable disease”, which is reflected in the UN Resolution adopted at the 61st General Assembly of this organization in 2006.
Effective treatment of diabetes lies primarily in maintaining target glycemic levels for many years, or more precisely, throughout the patient’s entire life. For most patients with T2DM, this is a serious challenge, given the concomitant pathology: arterial hypertension, dyslipidemia, manifestations of atherosclerosis, etc., which also requires monitoring and treatment and often leads to the phenomenon of polypharmacy. A serious factor complicating the management of the disease is also the age of the majority of patients with T2DM, which makes it difficult to carry out treatment and control measures due to decreased vision, motor, and sometimes cognitive impairment. It is no secret that such patients pose a big problem in the practice of an endocrinologist, therapist, and other specialists, as a result of which diabetes often remains insufficiently compensated.
Of course, the basal-bolus regimen is closest to the physiological secretion of insulin, which is a separate administration of short- and long-acting insulin, which allows you to vary the dose of each injection, taking into account all influencing factors (current glycemic indicators, carbohydrate content in food, etc.). However, due to the large number of injections and the complexity of the complex of measures to manage the therapeutic process, the use of a basal-bolus regimen is not possible for all patients with T2DM who require insulin therapy. In this regard, the use of biphasic insulin preparations has become widespread and has become a highly effective alternative to the basal-bolus regimen for patients with T2DM. The combination of two drugs with different durations of action in one provides ease of use and allows one to avoid errors during administration, which are often reported by patients: the introduction of a short-acting drug instead of a long-acting one, and vice versa. Fewer injections are also required during the day - 1-3 instead of 4 or more with a basal-bolus regimen.
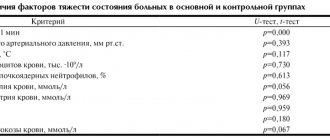
However, biphasic human insulins (BIH) have a number of pharmacokinetic and pharmacodynamic limitations that can lead to both early postprandial hyperglycemia and late postprandial hypoglycemia. They also require approximately a 30-minute pause between the injection and the start of food intake, which is not always tolerated by patients. Premixed insulin analogues were created to overcome the listed limitations in the action of DCI. A number of studies have demonstrated better postprandial glycemic indicators during therapy with the biphasic analog insulin drug NovoMix 30 compared to DCI [5], a lower risk of hypoglycemia, especially at night [6, 7] and severe [8, 9]. These advantages are due to the pharmacokinetics and pharmacodynamics of NovoMix 30, which are close to those during endogenous insulin secretion in healthy people. In a study by T. Heise et al. demonstrated the pharmacological advantages of NovoMix 30 over DCI with the same ratio of short- and long-acting fractions identified during the 24-hour euglycemic clamp procedure [10]. These advantages include a higher concentration of insulin in the blood (73.1–100.4 U/l on NovoMix 30 versus 46.7 on DCI) 1; shorter time to reach maximum concentration (2.1–2.6 hours for NovoMix 30 versus 3.2 for DHI). The pharmacokinetic profiles of insulin NovoMix 30 and DChI are presented in Fig. 1.
It is also worth noting the comparable effectiveness of NovoMix 30 insulin therapy when administered 3 times a day in comparison with basal-bolus therapy [4,12].
Since biphasic analogue insulin mixtures are also represented by drugs with a different ratio of short and extended fractions (25/75 and 50/50), their comparison is especially interesting. When NovoMix 30 was compared with biphasic insulin lispro Mix 25 in an international open-label crossover study of 137 patients with T2DM [13], both insulins resulted in comparable reductions in glycated hemoglobin (HbA1c) and glycemic levels. The frequency of hypoglycemia episodes (0.69 and 0.62 episodes per month for NovoMix 30 and Lispro Mix 25, respectively; p = 0.29) was also similar.
In a study by Hermansen et al. [14] compared postprandial blood glucose levels during the use of insulin NovoMix 30, lispro Mix 25 and DCI. NovoMix 30 demonstrated the best indicators of postprandial control, presented as an excursion of glucose levels in the interval 0-5 hours after eating. This indicator on insulin NovoMix 30 was 17% lower compared to DCI (p < 0.001) and 10% lower compared to lispro Mix 25 (p < 0.05). At the same time, the glucose level excursion was lower both in the early (0–2 hours) and late (2–5 hours) postprandial phases when compared with DHI (in both cases p < 0.01), and in the late phase when compared with lispro mix 25 (p < 0.05).
In a 16-week, open-label, randomized, multicenter study, Farcasiu et al. [15] compared two strategies for intensifying insulin therapy in patients with T2DM who had not achieved compensation with the use of biphasic insulin analogues: NovoMix 30 or Lispro Mix 25 (total number of patients – 302). One consisted of switching to a biphasic insulin preparation with a high content of the short fraction - lispro mix 50 - in a regimen of three injections per day; the other is in further titration of the doses of the initially received drugs: NovoMix 30 or Lispro Mix 25 (both twice a day). A significant and clinically significant improvement in glycemic control was observed in both groups, but the final HbA1c level did not differ between groups (7.70% in the lispro mix 50 group 3 times a day and 7.84% in the NovoMix 30 and lispro mix 25 group - 2 times a day per day) 2. The authors attribute the absence of such differences to the fact that therapy with lispro mix 50 3 times a day showed the best level of afternoon glycemia, but the worst level of fasting plasma glucose (FPG) and after breakfast, probably due to an insufficient dose of prolonged insulin fractions. Obviously, in this regard, 27% of patients in the lispro mix 50 3 times a day group switched to the previous insulin therapy regimen with drugs with a lower content of short-acting insulin and a higher content of long-acting insulin fraction before the evening meal.
Thus, preparations of ready-made mixtures of insulin analogues with different ratios of ultra-short and long-acting fractions allow for an individual approach to the treatment of diabetes in patients with different needs for insulin at different times of the day and different lifestyles, and do not replace each other.
As studies have shown, NovoMix 30 is convenient for both initiation and intensification of insulin therapy (one drug is used in one syringe pen, only the appropriate dose or number of injections is selected from one to two or three), and in addition, patients easily follow the algorithm titration recommended by your doctor. For example, in a study by Garber et al. (study “1-2-3”) [16] included 100 patients with T2DM with HbA1c levels in the range of 7.5–10.0%: 72 of them had previously received oral hypoglycemic drugs (OHLDs), the rest - OGDs in combination with basal insulin. Patients were prescribed NovoMix 30, while basal insulin was discontinued if the patient was receiving it. Treatment began with one injection per day, followed by self-titration of the dose of NovoMix 30 insulin until a target FPG level of 4.4–6.1 mmol/l was achieved. After 16 weeks of therapy, 21% of patients achieved the target level of HbA1c ≤ 6.5%, and 41% of patients achieved HbA1c ≤ 7.0%. The remaining patients were prescribed a second injection of NovoMix 30 per day. After another 16 weeks, the target level of HbA1c ≤ 6.5% was achieved by 52% of patients, HbA1c ≤ 7.0% by 70% of patients. The remainder were prescribed a third injection of DIAsp 30 for another 16 weeks.
The use of such a step-by-step titration algorithm for NovoMix 30 (a gradual transition from one to three injections when therapeutic goals were not achieved) allowed the majority of patients to achieve target glycemic control at the end of the study: HbA1c levels ≤ 6.5% were achieved by 60% of patients, ≤ 7.0% - 77 % of patients. It should be noted that the increase in the frequency of administration of DIAsp 30 throughout the study was not accompanied by an increase in the risk of severe hypoglycemia (requiring outside assistance for relief).
Moreover, no cases of severe hypoglycemia were reported throughout the study.
And the frequency of mild (self-limited by the patient) hypoglycemia did not correlate with the number of injections during the day.
Even more impressive results were obtained by Lightelm et al. [17] in an open-label, non-randomized, prospective observational study of 18 months conducted in routine clinical practice. NovoMix 30 was prescribed to patients with T2DM in whom treatment with PSSP (n = 90) or a previous insulin regimen (n = 59) was ineffective (initial mean HbA1c level was 8.4%). Within 10 weeks from the start of therapy, patients were taught methods of self-monitoring of glycemia and dose adjustment of NovoMix 30 using a simple titration algorithm: first, a dose selection algorithm was used based on the results of FPG measurement, and after the patients mastered it, they were taught a second dose selection algorithm based on the results of self-control after meal. The need to increase the number of injections was determined by the doctor. By the end of the study, all participants showed a statistically significant decrease in HbA1c levels by an average of 1.9 ± 0.1%.
HbA1c levels <7.0% were achieved in 90% of patients, ≤ 6.5% – in 52%.
Severe and nocturnal hypoglycemia were not recorded; mild ones were noted in 15% of patients. The body weight of patients who had not previously received insulin increased by an average of 2.7 kg, and in patients switched to NovoMix 30 from other insulin preparations, it decreased by an average of 0.6 kg.
Thus, the ease of use of the drug NovoMix 30, the successful mastery of the titration algorithm by patients in routine clinical practice allow the vast majority of patients (90%) to achieve target indicators of carbohydrate metabolism with a very good safety profile: a small number of only mild hypoglycemia and even a slight decrease in body weight with transfer from other insulin preparations.
Although randomized controlled trials are considered the gold standard in terms of evidence-based medicine, prospective observational programs are of great interest as a step in translating the results of these trials into clinical practice. Observational programs make it possible to cover a large number of patients, whose demographic and medical characteristics are more consistent with the realities of general clinical practice, and to identify rare side effects that do not appear in small samples.
Of particular interest to the domestic endocrinological community is the fact that Russian patients also took part in a number of observational studies (PRESENT, IMPROVE, A1chieve) using NovoMix 30 insulin 3. The results of these large-scale programs were published both in international [18–31] and in domestic scientific and medical journals [32, 33].
Below are the results of the recently completed largest international observational program A1chieve, the purpose of which was to comprehensively study the effectiveness and safety of therapy for T2DM with analog insulin drugs - NovoMix 30, detemir (Levemir) and aspart (NovoRapid), in real clinical practice. A total of 66,726 patients with T2DM from 28 countries located on 4 continents (more than 3,000 patients from Russia) took part in the study. A total of 40,917 patients with T2DM who participated in the A1chieve program used NovoMix 30 as monotherapy or in combination with PSSP (of which 27.6 thousand were “insulin-naïve” and 13.3 thousand had previously received other insulin drugs); The Russian cohort consisted of 1226 patients (730 patients who had not previously received insulin, and 496 who had previous experience of insulin treatment). The data is presented on the information portal The A1chieve Resource Center https://www.a1chieve.com
The use of NovoMix 30 led patients, both those who had not previously received insulin and those switched from other insulins, to improved glycemic control after 24 weeks (decrease in HbA1c by 2.5 and 2.0%, fasting plasma glucose - FPG - by 4.5 and 3.1 mmol/l, postprandial glycemia - PPG - by 5.2 and 3.5 mmol/l in patients who had not previously received and received insulin, respectively). About 30% of patients achieved HbA1c < 7% by the end of the study. The average daily dose of NovoMix 30 after 24 weeks was 44.0 and 51.8 units for insulin-naïve and insulin-treated patients. In individuals who had previous experience with insulin treatment, the incidence of all and nocturnal hypoglycemia after switching to DIAsp decreased by 7.0 and 2.6 cases/patient/year, respectively. It is quite natural that the initiation of insulin use in patients who had not previously received insulin was accompanied by an increase in mild hypoglycemia, but their frequency increased slightly (by 3.2 cases/patient/year). In addition, despite the presence of excess body weight in the majority of participants (the average body mass index - BMI - in the analyzed cohort at the beginning of the study was 31.2 kg/m2); NovoMix 30 therapy did not lead to an additional increase in body weight: after 24 weeks, body weight decreased by 0.2 and 1.0 kg in those who had not previously received and received insulin.
An additional, no less significant advantage of NovoMix 30 insulin therapy, in addition to a significant and safe improvement in glycemic control, was a clinically significant improvement in the health-associated quality of life of patients (assessed using the standard EQ-5D questionnaire - EuroQol-5D) [26].
A separate study carried out as part of the international prospective observational program A1chieve in Russia (n = 9,342, duration 52 weeks) also demonstrated the high efficacy and safety of NovoMix 30 therapy with respect to the risk of hypoglycemia. Initiation of insulin therapy in patients with T2DM without previous experience of treatment with insulin analogues insulin Levemir (insulin detemir), NovoMix 30 or the basal-bolus regimen of Levemir + NovoRapid in everyday clinical practice contributed to a significant improvement in glycemic control (after 12 months, a decrease in HbA1c by 2.9%) with no negative impact on the tolerability and safety of therapy [34 ].
It is noteworthy that when choosing a regimen for starting insulin therapy, about a third (29%) of doctors preferred NovoMix 30. Moreover, if the number of patients who started therapy with a basal insulin analogue decreased by the end of the study due to the need to intensify therapy by adding bolus insulin, then the number of patients receiving DIAsp therapy even increased slightly after 12 months (up to 32%).
It is also characteristic that the most optimal glycemic control in terms of improvement of all glycemic parameters (especially PPG as an independent adverse cardiovascular risk factor) was observed precisely in the subgroup of patients receiving NovoMix 30. The dynamics of HbA1c and PPG were comparable to those during treatment with basal-bolus regimen (decrease in HbA1c level during treatment with basal insulin by 2.7%, during treatment with DIAsp - by 3.0% and on basal-bolus therapy - by 3.3%; decrease in PPG by 5.1, 6.1 and 6, 8 mmol/l, respectively) (Fig. 2).
The dynamics of FPG during therapy with NovoMix 30 insulin were comparable to those when using basal insulin (a decrease of 5.0 and 4.7 mmol/l compared to the initial level, respectively).
Severe hypoglycemia during treatment with insulin NovoMix 30, as well as with other insulin therapy regimens under study, was extremely rare [34]. There was virtually no weight gain during DIAsp therapy over the course of a year (+0.1 kg after 6 months without further weight gain over the next 6 months).
An important component of the presented A1chieve study was a study of patient satisfaction with treatment, which was carried out at baseline and after 12 months using a validated Russian version of the specific DiabMedSat© questionnaire (Diabetes Medication Satisfaction Questionnaire). Against the background of all studied insulin therapy regimens using insulin analogues, a pronounced positive dynamics of this indicator was noted (an increase in the score from 33.3 points during the initial visit to 76.2 at the end of the study, i.e. +42.8 points over 12 months) [34]. At the same time, the increase in satisfaction with treatment 6 months after the initiation of insulin therapy was most pronounced when starting with NovoMix® 30, which most likely reflects a subjective high assessment of the effectiveness and safety of therapy with this insulin, as well as the convenience and ease of its use.
Thus, this observational study conducted in Russia also confirmed all the advantages of treatment with the biphasic insulin analogue NovoMix 30: high efficiency in improving all parameters of glycemic control, safety in relation to hypoglycemia and the effect on body weight, as well as favorable patient attitude towards it.
Finally, since the main population of patients receiving NovoMix 30 are older people, the recently published subanalysis of the efficacy and safety of NovoMix 30 insulin in different age groups within the framework of the 26-week international A1chieve study is of great interest [29].
Of the 40,917 patients receiving NovoMix 30, 4,347 were under 40 years of age, 29,036 were aged 40–65 years, and 6,739 were over 65 years of age. Most (65%) of them had no previous experience with insulin therapy.
It should be noted that with initially similar unsatisfactory control in all age groups (average HbA1c level - 9.4–9.6%), after 24 weeks the dynamics of HbA1c were also very similar: a decrease in HbA1c by 2.3% in patients under 40 years of age and by 2.0% in other age groups (p < 0.001 in all groups). Moreover, the dynamics of HbA1c levels were more pronounced in patients without previous experience of insulin treatment.
The decrease in FPG and PPG was pronounced in all age groups, the most pronounced positive dynamics were observed in patients under 40 years of age (reduction in FPG by 4.2 mmol/l; PPG by 6.1 mmol/l), the minimum in patients over 65 years of age (FPG – -3.4 mmol/l; PPG – -4.0 mmol/l), in all cases the difference was significant (p < 0.001) [29].
The proportion of patients who experienced at least one hypoglycemia (any episode) decreased significantly in all age groups, although there was a slight increase in this indicator in people without experience of insulin treatment over 65 years of age (from 3.8 ± 0.99 cases/patient/year initially to 6.1 ± 1.49 cases/patient/year; p < 0.001) [29]. At the same time, in the entire analyzed sample, the proportion of patients with severe hypoglycemia decreased significantly – to 0–0.1%. Even in patients without previous experience of insulin therapy aged 40–65 and over 65 years, no severe hypoglycemia was recorded throughout the entire observation period (24 weeks) (initial incidence of severe hypoglycemia in patients who had not previously used insulin, aged under 40 years, 40 –65 and over 65 years were 0.2 ± 0.03, 0.5 ± 0.08 and 0.8 ± 0.15 cases/patient/year; p < 0.001, respectively). The proportion of patients who experienced nocturnal hypoglycemia also decreased significantly in all age groups, except for older people (≥ 65 years) with no previous experience of insulin therapy, although among them this proportion was small (1.6 ± 0.33 after 24 weeks vs. 1.3 ± 0.32 cases/patient/year at baseline).
Regardless of age and previous therapy, weight gain was insignificant: 0.2–0.7 kg.
The results of the presented subanalysis confirm that, regardless of age, both when initiating insulin therapy and when transferring from other insulin preparations, NovoMix 30 provides a significant improvement in glycemic control. The increasing proportion of patients with mild hypoglycemia among patients over 65 years of age without previous experience with insulin therapy further emphasizes the need to educate such patients both at the beginning of insulin treatment and thereafter.
To summarize, we can state that ten years of experience in the use of the biphasic insulin analogue NovoMix 30 has reliably confirmed its high efficiency, safety, convenience and ease of initiation and intensification of insulin therapy for DIAsp. NovoMix 30 can also be used as an alternative to the basal-bolus regimen when intensifying therapy after basal insulin, when the ability to adhere to the regimen of multiple injections of two different types of insulin, as well as regular self-monitoring of glycemia, necessary for the success of basal-bolus therapy, is difficult or impossible.
Conflict of interest The author declares that there is no conflict (duality) of interest in connection with the preparation of this manuscript.
Use of the drug Novomix 30 flexpen
Insulin dosage is individual and determined by the doctor in accordance with the patient's needs. Since the effect of NovoMix 30 FlexPen occurs faster than biphasic human insulin, it should be administered immediately before meals. If necessary, NovoMix 30 FlexPen can be administered a short period of time after meals. On average, a patient's need for insulin is, depending on body weight, from 0.5 to 1.0 IU/kg/day. It can be fully or partially achieved by administering the drug NovoMix 30 FlexPen. The daily need for insulin may increase in patients with insulin resistance (for example, obesity) and decrease in patients with remaining residual production of endogenous insulin. NovoMix 30 FlexPen is usually injected subcutaneously into the thigh area. You can also make injections into the area of the anterior abdominal wall, buttocks or deltoid muscle of the shoulder. To avoid lipodystrophy, injection sites should be changed even within the same body area. Like other insulin medications, the duration of action may vary depending on the dose, injection site, blood flow rate, temperature and level of physical activity. The dependence of the absorption rate on the site of drug administration has not been studied. For patients with type II diabetes mellitus, NovoMix 30 FlexPen can be prescribed both as monotherapy and in combination with hypoglycemic agents (GLDs) in cases where the blood glucose level cannot be effectively regulated with GLDs alone. For patients with type II diabetes mellitus, the recommended initial dose of NovoMix 30 FlexPen in combination with metformin is 6 units before breakfast and 6 units before dinner. You can begin its administration with a dose of 12 units before dinner. After reaching a dose of 30 units, it is usually recommended to switch from a single injection to two injections per day of 15 units before breakfast and dinner. Then you can safely switch to three injections per day and administer half the morning dose before breakfast and lunch. When selecting doses, it is recommended to be guided by the data in the table below
Pre-meal blood glucose levels | Selection of the dose of the drug NovoMix 30 | |
| ≤ 4.4 mmol/l | ≤80 mg/100ml | –2 units |
| 4.4–6.1 mmol/l | 80–110 mg/100 ml | 0 |
| 6.2–- 7.8 mmol/l | 11–-140 mg/100 ml | + 2 units |
| 7.9–10 mmol/l | 141–180 mg/100 ml | + 4 units |
| 10 mmol/l | 180 mg/100 ml | + 6 units |
You should focus on the lowest glucose concentrations over the last three days. If there were episodes of hypoglycemia during this period, the insulin dose is not increased. The dose is adjusted once a week until the target HbA1c level is achieved. The adequacy of the previous dose is assessed by the glucose concentration values before meals. Impaired liver or kidney function may reduce the patient's need for insulin. NovoMix 30 FlexPen can be used in children and adolescents aged 10 years and older, when the administration of a mixture of insulin is preferable. Data from clinical studies on the use of the drug in children 6-9 years of age are limited. Studies have not been conducted in children under 6 years of age. NovoMix 30 FlexPen can be used in elderly patients; however, experience with its use in combination with PSS in individuals over 75 years of age is limited. NovoMix 30 FlexPen should never be administered intravenously. Instructions for use of the drug NovoMix 30 FlexPen for a patient The need to thoroughly mix the insulin suspension before use should be emphasized. After mixing, the suspension should be uniformly white and cloudy. NovoMix 30 FlexPen is intended for individual use only. Do not refill NovoMix 30 FlexPen. NovoMix 30 FlexPen is used with short NovoFine® needles. Before using NovoMix 30 FlexPen: you must check the label to see if the type of insulin you are using is correct. Always use a new needle for each injection. Do not use NovoMix 30 FlexPen:
- in insulin pumps;
- if the FlexPen syringe pen has been dropped, if it is damaged or deformed, since in these cases insulin leakage may occur;
- if the syringe pen was stored incorrectly or was frozen; if after stirring the suspension does not become uniformly white and cloudy; if the product has white clumps or hard white particles stuck to the bottom or walls of the cartridge, giving it the appearance of being frozen.
NovoMix 30 FlexPen is intended for subcutaneous injection. The drug should not be administered intravenously or directly into the muscle. To avoid the formation of infiltrates, injection sites should be constantly changed. The best places for injection are the anterior abdominal wall, buttocks, anterior thigh or shoulder. Insulin works faster when injected into the waist area.
Side effects of the drug Novomix 30 flexpen
Adverse reactions observed in patients using NovoMix 30 FlexPen are mainly related to the size of the administered dose of the drug and are a manifestation of the pharmacological action of insulin. The most common side effect of insulin therapy is hypoglycemia. It may appear if the dose significantly exceeds the patient's need for insulin. Severe hypoglycemia can cause loss of consciousness and/or seizures, followed by temporary or permanent impairment of brain function and even death. According to the results of clinical studies, as well as data recorded after the drug was marketed, the incidence of severe hypoglycemia varies in different patient groups and with different dosage regimens; The incidence of severe hypoglycemia in patients receiving insulin aspart is the same as in patients receiving human insulin. Below is the frequency of adverse reactions that, according to clinical studies, may be associated with the administration of NovoMix 30 FlexPen. Based on the frequency of occurrence, these reactions are divided into those observed sometimes (1/1000, ≤1/100) and rarely (1/10,000, ≤1/1000). Individual spontaneous cases are classified as very rare (≤1/10,000). From the immune system Very rare: anaphylactic reactions. Sometimes: urticaria, itching, skin rashes. Generalized hypersensitivity reactions may include skin rashes, itching, sweating, gastrointestinal disturbances, angioedema, difficulty breathing, palpitations and decreased blood pressure. These reactions are potentially life-threatening. From the nervous system. Rarely: peripheral neuropathies. Rapid improvement in blood glucose control may result in acute painful neuropathy, which is usually transient. Visual disturbances : Sometimes: refractive errors; may occur at the beginning of insulin therapy and are transient. Sometimes: diabetic retinopathy. Long-term maintenance of good glycemic control reduces the risk of progression of diabetic retinopathy. However, intensifying insulin therapy to rapidly improve glycemic control may cause a temporary exacerbation of diabetic retinopathy. From the skin and subcutaneous tissue: Sometimes: lipodystrophy; may occur at injection sites as a result of non-compliance with the recommendation to change drug injection sites within the same area; local hypersensitivity. When insulin is administered, manifestations of local hypersensitivity (redness, swelling and itching at the injection sites) may occur. These reactions are usually transient and disappear with continued treatment. Generalized disorders and reactions at injection sites Sometimes : local swelling; may develop at the beginning of insulin therapy. These symptoms are usually temporary.
Special instructions for the use of Novomix 30 Flexpen
Inadequate dosage or discontinuation of treatment (especially in type I diabetes mellitus) can lead to hyperglycemia and diabetic ketoacidosis; These conditions are potentially fatal. Patients who have significantly improved blood glucose control, for example through intensive care, may notice a change in the usual symptoms that are warning signs of hypoglycemia, about which patients should be warned in advance. NovoMix 30 FlexPen should be administered immediately before meals. The rapid onset of action of the drug should be taken into account when treating patients with concomitant diseases or taking medications that can slow down the absorption of food in the gastrointestinal tract. Concomitant diseases, especially infections and fevers, increase the patient's need for insulin. When transferring a patient to other types of insulin, early warning symptoms may change or be less pronounced than when taking the usual insulin drug. Transferring a patient to another type or type of insulin is carried out under strict medical supervision. Changes in the concentration, type (manufacturer), type, origin of insulin (animal, human or human insulin analogue) and/or production method may require dose adjustment. When switching to NovoMix 30 FlexPen injections, patients may need to change their usual insulin dose. The need to adjust the dose may arise both when a new drug is first introduced and during the first few weeks or months of its use. Skipping meals, sudden changes in diet, or unexpected intense physical activity can lead to hypoglycemia. Compared to biphasic human insulin, injection of NovoMix 30 FlexPen leads to a more pronounced hypoglycemic effect, which can last up to 6 hours. This may necessitate the selection of insulin doses and/or diet. The need to adjust the dose of the drug may arise with increased physical activity or changes in diet. Exercising immediately after eating increases the risk of hypoglycemia. Insulin suspensions should not be used in insulin pumps for continuous subcutaneous insulin administration. During pregnancy and breastfeeding. Clinical experience with the use of insulin aspart during pregnancy is limited. Animal studies have shown that insulin aspart, like human insulin, does not have embryotoxic or teratogenic effects. Enhanced monitoring is recommended when treating pregnant women with diabetes mellitus throughout the entire period of pregnancy, as well as if pregnancy is suspected. The need for insulin usually decreases in the first trimester of pregnancy and increases significantly in the second and third trimester. After childbirth, insulin requirements quickly return to baseline levels. There are also no restrictions on the treatment of diabetes mellitus with insulin during breastfeeding, since treatment of a nursing mother does not pose a risk to the child. However, it may be necessary to adjust the dose of NovoMix 30 FlexPen. Impact on the ability to drive vehicles and machinery. The patient's responsiveness and ability to concentrate may be impaired by hypoglycemia. This may become a risk factor in situations where these abilities are of particular importance (for example, when driving a car or operating machinery). Patients should be advised to take measures to prevent hypoglycemia before driving. This is especially important for those who have mild or no symptoms - warning signs of hypoglycemia or episodes of hypoglycemia occur frequently. Under such circumstances, the advisability and safety of driving should be weighed.
Use during pregnancy and breastfeeding
Clinical experience with the use of NovoMix® 30 Penfill®/FlexPen® during pregnancy is limited.
Studies on the use of NovoMix® 30 Penfill® in pregnant women have not been conducted.
However, data from two randomized controlled clinical trials (157 and 14 pregnant women, respectively, receiving basal-bolus insulin aspart) did not show any adverse effects of insulin aspart on pregnancy or fetal/newborn health compared with soluble human insulin. Additionally, a clinical randomized trial of 27 women with gestational diabetes treated with insulin aspart and soluble human insulin (insulin aspart in 14 women, human insulin in 13) demonstrated similar safety profiles for both types of insulin.
During the period of possible pregnancy and throughout its entire duration, it is necessary to carefully monitor the condition of patients with diabetes mellitus and monitor the concentration of glucose in the blood. The need for insulin, as a rule, decreases in the first trimester and gradually increases in the second and third trimesters of pregnancy. Shortly after birth, insulin requirements quickly return to pre-pregnancy levels.
During breastfeeding, NovoMix® 30 Penfill®/FlexPen® can be used without restrictions. Administration of insulin to a nursing mother does not pose a threat to the baby. However, it may be necessary to adjust the dose of NovoMix® 30 Penfill®/FlexPen®.
Interactions of the drug Novomix 30 flexpen
A number of drugs affect glucose metabolism, which should be taken into account when determining the dose of insulin. Drugs that reduce the need for insulin: oral hypoglycemic agents, octreotide, MAO inhibitors, non-selective beta-blockers, ACE inhibitors, salicylates, alcohol, anabolic steroids and sulfonamides. Drugs that increase the need for insulin: oral contraceptives, thiazides, corticosteroids, thyroid hormones, sympathomimetics and danazol. β-adrenergic receptor blockers can mask the symptoms of hypoglycemia, while alcohol can enhance and prolong the hypoglycemic effect of insulin. Incompatibility. Adding some drugs to insulin can cause it to break down, such as drugs containing thiols or sulfites. NovoMix 30 FlexPen cannot be added to infusion solutions.
Interaction
There are a number of drugs that affect the need for insulin. The hypoglycemic effect of insulin is enhanced by oral hypoglycemic drugs, MAO inhibitors, ACE inhibitors, carbonic anhydrase inhibitors, non-selective beta-blockers, bromocriptine, sulfonamides, anabolic steroids, tetracyclines, clofibrate, ketoconazole, mebendazole, pyridoxine, theophylline, cyclophosphamide, fenfluramine, lithium preparations, salicine ilats.
The hypoglycemic effect of insulin is weakened by oral contraceptives, corticosteroids, thyroid hormones, thiazide diuretics, heparin, tricyclic antidepressants, sympathomimetics, somatropin, danazol, clonidine, CCB, diazoxide, morphine, phenytoin, nicotine.
Beta blockers may mask the symptoms of hypoglycemia.
Octreotide/lanreotide can either increase or decrease the body's need for insulin.
Alcohol can increase or decrease the hypoglycemic effect of insulin.
Incompatibility. Since compatibility studies have not been conducted, NovoMix® 30 Penfill®/FlexPen® should not be mixed with other drugs.
Overdose of the drug Novomix 30 flexpen, symptoms and treatment
Although there is no specific definition of insulin overdose, hypoglycemia may occur when administered in excess. Mild hypoglycemia can be treated by ingesting glucose or sweet foods. Therefore, patients with diabetes are recommended to always have a few pieces of sugar, candy, cookies or sweet fruit juice with them. In case of severe hypoglycemia, when the patient is unconscious, it is necessary to administer intramuscular or subcutaneous injections of glucagon (0.5 to 1 mg) by a person who has received appropriate instructions. A healthcare worker can also administer intravenous glucose to the patient if the patient does not respond to glucagon administration within 10–15 minutes. After the patient regains consciousness, he should take carbohydrates orally to prevent relapse of hypoglycemia.
Compound
NovoMix® 30 Penfill®
| Suspension for subcutaneous administration | 1 ml |
| active substance: | |
| insulin aspart - soluble insulin aspart (30%) and insulin aspart protamine crystals (70%) | 100 units (3.5 mg) |
| excipients: glycerol - 16 mg; phenol - 1.5 mg; metacresol - 1.72 mg; zinc (in the form of zinc chloride) - 19.6 mcg; sodium chloride - 0.877 mg; sodium hydrogen phosphate dihydrate - 1.25 mg; protamine sulfate - about 0.32 mg; sodium hydroxide - about 2.2 mg; hydrochloric acid - about 1.7 mg; water for injection - up to 1 ml | |
| 1 cartridge (3 ml) contains 300 units |
NovoMix® 30 FlexPen®
| Suspension for subcutaneous administration | 1 ml |
| active substance: | |
| insulin aspart - soluble insulin aspart (30%) and insulin aspart protamine crystals (70%) | 100 units (3.5 mg) |
| excipients: glycerol - 16 mg; phenol - 1.5 mg; metacresol - 1.72 mg; zinc (in the form of zinc chloride) - 19.6 mcg; sodium chloride - 0.877 mg; sodium hydrogen phosphate dihydrate - 1.25 mg; protamine sulfate - about 0.32 mg; sodium hydroxide - about 2.2 mg; hydrochloric acid - about 1.7 mg; water for injection - up to 1 ml | |
| 1 pre-filled pen (3 ml) contains 300 units |
Storage conditions for the drug Novomix 30 flexpen
Shelf life - 2 years. The used syringe pen with NovoMix 30 FlexPen should not be stored in the refrigerator. A syringe pen that is used or carried in reserve should be stored for no more than 4 weeks (at a temperature not exceeding 30 ° C). An unused syringe pen with NovoMix 30 FlexPen should be stored in the refrigerator at a temperature of 2–8 ° C (not too close to the freezer). Do not freeze. To protect from light, store the syringe pen with the cap on.
List of pharmacies where you can buy Novomix 30 Flexpen:
- Moscow
- Saint Petersburg