To the reference book Sensorineural hearing loss is a lesion of one or more parts of the auditory analyzer.
Symptoms: hearing loss, tinnitus, dizziness and imbalance. Author:
- Sokolova Alla Vasilievna
otorhinolaryngologist, otosurgeon, doctor of the highest category
3.71 (Votes: 7)
Sensorineural hearing loss is a hearing loss that affects any of the sound-perceiving structures of the auditory analyzer. The conversion of sound wave energy in the organ of Corti of the cochlea (in some sources defined as sensorineural hearing loss) or the conduction of nerve impulses to the cerebral cortex may be impaired. Timely correction of pathological changes allows you to slow down or prevent the progression of the disease and avoid the development of complete deafness.
What is sensorineural hearing loss?
The perception of sounds is ensured by the coordinated work of all parts of the hearing organ. The outer ear (concha and ear canal) conduct sound waves to the middle ear. The eardrum converts the wave into mechanical vibrations. The auditory ossicles transmit these vibrations to the inner ear. The movement of fluid in the cochlea irritates the hair cells, which convert mechanical impulses into nerve impulses. The auditory pathways transmit signals to the temporal lobes of the brain, where the central part of the auditory analyzer is located. After processing impulses by cerebral structures, a person understands what he heard.
Treatment
When treating acute sensorineural hearing loss and deafness, the following principles must be observed:
- Eliminate the etiological factor that led to the disease;
- If a disease is detected, begin treatment immediately;
- Apply complex etiotropic (aimed at eliminating the cause of the disease) pathogenetic (affecting the mechanism of development of the disease) therapy, which will compensate for the lack of oxygen in the inner ear and bring microcirculation in it to a normal state.
Patients with an acute form of sensorineural hearing loss require emergency care in an ENT hospital. For toxic lesions, antidotes are prescribed - unithiol, sodium thiosulfate, calcium pantothenate; anticoagulant therapy, infusion (infusion) of vasoactive substances and agents such as heparin, trental, piracetam, ATP, cocarboxylase, vitamins B, A, E, galantamine, oxazole, nicotinic acid, corticosteroids, fibrinolytic (promoting the dissolution of blood clots) agents (streptokinase ).
Make an appointment right now!
Call us by phone or use the feedback form
Sign up
During the period of stabilization of sensorineural hearing loss, the patient is under the supervision of an audiologist and undergoes maintenance treatment courses twice a year. Such courses have an impact on tissue metabolism and include: taking vitamins and their analogues, biostimulants, anticholinesterase drugs, classes with an audiologist, as well as physiotherapy: electrophoresis with iodide preparations, galantamine, proserin, nicotinic acid, phosphobion, mud applications on the mastoid area processes, balneotherapy (radon), endaural electrical stimulation.
If hearing loss exists for a long time, then this is an indication for hearing aid, including cochlear implantation of electrodes.
Types of sensorineural hearing loss
The International Classification of Diseases (ICD-10) identifies the following forms of sensorineural hearing loss:
- H90.3 - double-sided;
- H90.4 - unilateral with preserved function of the second ear;
- H90.5 - unspecified.
And also H91:
- H91.0 - ototoxic hearing loss;
- H91.1—presbycusis;
- H93.3—damage to the auditory nerve.
In clinical practice, congenital, or early, form of sensorineural hearing loss is distinguished and acquired (all other cases). Based on the duration of the disease, hearing loss can be:
- sudden (hearing decreases within 12 hours);
- acute (hearing loss occurs within 1–3 days, the disorder persists for about a month);
- subacute (hearing loss occurs over 1–3 months);
- chronic (the process drags on for 3 months or more).
Taking into account the nature of its course, hearing loss can be reversible, stable and progressive.
2. Sudden hearing loss
Acute sensorineural hearing loss can have such a rapid course that it is classified as a separate group, the so-called “sudden hearing loss.”
. In this case, significant or even complete deafness develops within several hours (up to half a day). This situation has a number of specific features. Sudden hearing loss often ends with an equally rapid recovery. If sudden sensorineural hearing loss occurs during sleep, the patient is awakened by a sensation that is described as a broken telephone wire, that is, sudden silence wakes the patient in the same way as a loud sound. Most often, sudden hearing loss is unilateral.
Visit our Therapy page
Degrees of sensorineural hearing loss
Based on hearing thresholds, there are 4 degrees of sensorineural hearing loss:
- First. The problem of sound perception is noticeable only in certain situations (noisy room, conversation with several interlocutors at once, etc.) The threshold is increased to 25–40 dB.
- Second. The perception of quiet speech and whispers is seriously difficult. The threshold is increased to 41–55 dB.
- Third. Problems arise with speaking. The hearing threshold is 56–70 dB.
- Fourth. The patient hears only loud sounds from sources located in the immediate vicinity. The threshold is increased to 71–90 dB.
Deafness is diagnosed if a person cannot hear even very loud sounds, more than 91 dB.
Treatment of sensorineural hearing loss
To make a diagnosis of sensorineural hearing loss, a specialist must conduct pure tone threshold audiometry - an objective test of the patient's hearing using an audiometer. The person puts on special headphones, and he picks up a special remote control with a button. Sounds of different frequencies and volumes are delivered to each ear of the patient in turn; if the person hears them, he reacts by pressing a button. In this way, an audiogram is formed - a graph reflecting the degree and nature of hearing impairment.
Treatment for sensorineural hearing loss can only be successful in the earliest stages. As we remember, hearing begins to decline due to the fact that the nerve cells of the auditory analyzer are poorly supplied with oxygen. The task of the patient and the specialist is to react in a timely manner before they die. Therefore, treatment will be aimed at improving blood circulation in problem areas. If a person does not receive qualified help on time, sensorineural hearing loss will become irreversible.
Like any disease, sensorineural hearing loss is easier to prevent than to treat: a healthy lifestyle, timely treatment of otitis media and viral diseases, fresh air and careful attention to protection from ambient noise will allow you to keep your hearing healthy.
If the disease has become chronic, there is no need to despair. Yes, the consequences are irreversible, yes, a person will never be able to hear on his own, but today there are technologies that allow a hearing-impaired person not only to return to live communication, but also to preserve residual hearing.
Sensorineural hearing loss, disability
Today in Russia, disability for sensorineural hearing loss is assigned at the 4th degree of reduction. This is the deepest degree, followed only by complete deafness. Children are assigned disabled status at the 3rd degree. Also, those who have chronic sensorineural hearing loss, bilateral, grade 3 or lower, can often count on disability.
Causes of sensorineural hearing loss
Sensorineural hearing loss in children can be caused by:
- abnormalities of brain development;
- developmental disorders of the cochlea;
- adverse effects on the mother’s body during pregnancy (intoxication, previous infections, etc.);
- genetic mutations;
- difficult childbirth.
Acquired hearing loss may be associated with the following factors:
- head injuries;
- acoustic injuries (the most common is listening to music on headphones at high volume);
- barotrauma;
- past intoxications;
- viral diseases;
- acute and chronic otitis;
- treatment with ototoxic drugs;
- local and systemic metabolic disorders;
- tumors;
- vascular pathologies;
- work in hazardous conditions;
- autoimmune diseases.
The causes of acute sensorineural hearing loss are often traumatic factors (traumatic brain injury, exposure to toxins, infection, etc.). If treatment begins on time, in the first 3 days, there is a chance of complete restoration of hearing.
Chronic sensorineural hearing loss is most often associated with progressive changes in the structures of the inner ear. Treatment requires the elimination of provoking factors, the use of conservative methods to slow the development of pathology and rehabilitation measures (hearing correction).
Sensorineural hearing loss - symptoms and treatment
Sensorineural hearing loss (sensorineural hearing loss, sensorineural hearing loss) is a decrease or loss of hearing as a result of damage to the sound-receiving apparatus. The pathology is quite common [1][2][3][6][7][8].
The organ of hearing is divided into sound-conducting and sound-receiving sections. The sound-conducting section is designed to transmit sound vibrations to the receptor; it includes:
- outer ear;
- middle ear.
The sound-perceiving department is responsible for the reaction of nervous tissue to sound stimulation; it includes:
- inner ear;
- auditory nerve;
- subcortical centers and pathways;
- auditory cortex of the brain.
Sensorineural hearing loss occurs when there is a violation of the sound perception department. Hearing loss associated with damage to the sound-conducting region is called conductive hearing loss . If there are disturbances in both departments, they speak of mixed hearing loss .
Sensorineural hearing loss is not an independent form of the disease, it is a collective concept that unites several different nosological forms. There can be many reasons for its occurrence, but the symptom is always the same - hearing loss. In different countries and even within the same country, but in different scientific communities, this disease is called differently: sensorineural hearing loss, sensorineural hearing loss, perceptual hearing loss, cochleoneuritis, cochlear neuropathy. All these names are relevant, since each of them reflects the concept of hearing impairment at a different level of the human auditory system. In Russia, the name “Sensorineural hearing loss” is accepted.
The International Classification of Diseases, 10th Revision (ICD-10) has the name “Sensorineural Hearing Loss”. According to the definition in the Clinical Guidelines developed by the National Medical Association of Otorhinolaryngologists of the Ministry of Health of the Russian Federation in 2016: “Sensorineural hearing loss (sensorineural hearing loss, perceptual hearing loss, cochlear neuropathy) is a form of hearing loss (up to loss) in which any of the areas of the sound-receiving section of the auditory analyzer, starting from the direct sensory apparatus of the cochlea and ending with damage to neural structures.” [8]
First of all, it must be noted that hearing loss means a decrease in the sensitivity of tonal hearing and a decrease in speech intelligibility [11]. Tonal hearing sensitivity , or auditory perception threshold, means a person’s perception of the quietest sound of a certain frequency (tone) during pure-tone audiometry.
There are two types of transmission of sound vibrations from the external environment: air conduction and bone conduction. Airborne sound conduction is the normal pathway for sound vibrations to enter the ear as sound travels through the pinna and external auditory canal to the eardrum. With bone conduction, sound vibration passes through the bones of the skull directly into the cochlea, bypassing the middle ear.
During audiometry, both types of sound conduction are tested. Hearing thresholds (the quietest sound that the test subject hears) are expressed in conventional units - decibels (dB). Normally, a person’s hearing thresholds should be from -10 dB to 15 dB over the entire frequency range, 20 dB is considered the borderline value between normal and pathological.
According to the World Health Organization, more than 5% of the world's population, or 466 million people (432 million adults and 34 million children), have hearing impairment greater than 40 dB in the better hearing ear for various reasons [20]. In the Russian Federation, the number of patients with hearing loss exceeds 13 million people, of which more than 1 million are children. Out of 1000 newborns, one child is born with total deafness. In addition, during the first 2-3 years of life, another 2-3 children lose their hearing. 14% of people aged 45 to 64 years and 30% of people over 65 years old have hearing problems [8].
Causes of the disease
In case of sensorineural hearing loss, the cause of hearing loss lies in a disorder (or disease) of the sound-receiving part of the auditory analyzer at the cochlear and retrocochlear level.
Cochlear level:
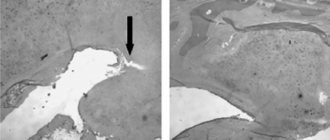
- Cochlear hair cell receptors. Sensory disorders - death or dysfunction of cochlear hair cells due to infection, intoxication, vascular or hereditary pathologies.
- Fibers of the auditory nerve before exiting the internal auditory canal. Neural disorders - damage to the auditory nerve due to trauma, neuronitis (inflammation) of the auditory nerve, disruption of the myelin sheath of the auditory nerve, etc.
Retrocochlear level:
- The pathways and nuclei of the medulla oblongata perform the function of sound conduction and primary analysis of sound (stem disorders).
- The cortical section - fields 41 and 42 (Heschl's gyrus) - performs the function of fine analysis of sound and speech intelligibility (cortical disorders).
Any pathology affecting one or more levels of the sound-perceiving auditory analyzer can lead to sensorineural hearing loss or deafness.
Factors in the development of sensorineural hearing loss
Sensorineural hearing loss (sensorineural) is a disease that develops as a result of exposure to many factors [1][2][3][4][6][7][8]: vascular, infectious, traumatic, metabolic, age-related, congenital, hereditary , metabolic, immune, as a complication after suffering otitis and other diseases of the middle ear, such as otosclerosis, tympanosclerosis and many others.
Vascular factors in the development of sensorineural hearing loss [3][4][5].
Vascular disorders are the most common cause of sensorineural hearing loss and are detected in approximately 40% of cases.
Vascular disorders in the auditory analyzer occur with hypertension, neurocirculatory dystonia, cerebrovascular accident (stroke), atherosclerosis of cerebral vessels, changes in the blood coagulation system, and cervical osteochondrosis.
The peculiarity of its blood supply predisposes to vascular disorders in the inner ear - the internal auditory artery is a terminal artery and does not have anastomoses (connections with other arteries). Therefore, the slightest changes in blood supply lead to hypoxia (lack of oxygen) of hair cells and their death.
Vascular factors also include the occurrence of sensorineural hearing loss in children during the peripartum period - this is fetal hypoxia and hypoxia that occurs during childbirth with cerebral circulatory disorders of varying severity.
Infectious factors in the development of sensorineural hearing loss [3][4][6][7][8].
In 30% of cases, sensorineural hearing loss develops under the influence of infectious factors. Especially often, damage to the auditory analyzer occurs during viral infections: most often it is influenza, mumps (characterized by predominant damage to the parotid salivary glands), measles, tick-borne encephalitis, herpes, cytomegalovirus infection, especially those transmitted in utero, meningococcal infection, syphilis and some others. Sometimes sensorineural hearing loss develops as a complication against the background of viral neuritis (inflammation of the nerves), viral ganglionitis (inflammation of the sympathetic nerve ganglion) or arachnoiditis of the posterior cranial fossa with damage to the cerebellopontine angle.
An infectious factor is often the cause of prenatally acquired sensorineural hearing loss in children whose mothers during pregnancy had or were carriers of infections such as toxoplasmosis, chicken pox, rubella, herpes infection, cytomegalovirus infection, HIV, chlamydia, hepatitis B and syphilis, listeriosis.
The risk group for the development of sensorineural hearing loss during the newborn period includes children who have suffered from generalized and localized infectious diseases: sepsis, omphalitis (bacterial inflammation of the bottom of the umbilical wound), meningoencephalitis, pneumonia.
Toxic factors in the development of sensorineural hearing loss [3][4][6].
Any toxic substances that can penetrate the blood-brain barrier can cause sensorineural hearing loss, especially with concomitant kidney disease, otitis media or decreased immunity. Most often these are ototoxic medications, as well as household and industrial poisons.
Ototoxic drugs include:
- Aminoglycoside antibiotics : streptomycin and its derivatives (kanamycin, monomycin, neomycin, amikacin, gentamicin) - this group is the most toxic, as well as tobramycin, abrekacin, dibekacin, amycin, isepamycin, frameticin, libidomycin, sisomycin, bleomycin, ristomycin. Aminoglycosides have a cumulative property, i.e. they accumulate in the nervous system of the body. If during the first course there was no damage to the spiral ganglion or vestibular system, then with the next prescription, hearing loss may occur even after the first injection of any other drug from this group. Children during intrauterine development and under the age of two years and the elderly are most sensitive to their effects. The use of aminoglycosides during pregnancy at any stage can cause deafness in the child.
- Amphomycin group : rifampicin.
- Glycopeptide antibiotic : vancomycin.
- Antibiotics of the amphenicol group : chloramphenicol, chloramphenicol.
- Antibiotics of the macrolide group : erythromycin, midecamycin, roxithromycin (“Roxyhexal”, “Rulid”) spiramycin (“Rovamycin”). An ototoxic reaction usually develops after a minimum of 36 hours and a maximum of 8 days from the start of treatment. If the drug is immediately discontinued and detoxification treatment is started, hearing may improve, and when taking macrolides, it is usually completely restored.
- Antitumor drugs : cisplastin, transplastin, vincristine, etc.
- Loop diuretics : furosemide (Lasix), ethacrynic acid, bumetanide.
- Nonsteroidal anti-inflammatory drugs : acetylsalicylic acid (“Aspirin”), sodium salicylate, naproxen, indomethacin.
- Ephedrine processing products : ephedrine, methcathinone.
- Antimalarials : quinine, delagil, mefloquin.
- Arsenic preparations : osarsol, stovarsol.
- Local preparations : ointments and drops containing ototoxic antibiotics:
- ointments erythromycin, polymyxin, tetracycline, chloramphenicol;
- ear drops: Sofradex, Anauran, candibiotic. These ointments and drops cannot be used for perforation in the eardrum.
- Many anti-tuberculosis drugs.
- Organic dyes and many industrial poisons.
Ototoxic medications should be prescribed strictly only for health reasons. They should not be prescribed to children under two years of age, pregnant women and people at risk for developing hearing loss or who already have any hearing loss. Moreover, you cannot use these drugs without a doctor’s prescription for self-medication.
Toxic factors in the development of sensorineural hearing loss include hemolytic disease of the newborn or prolonged hyperbilirubinemia with an increase in bilirubin in a child of more than 20 mmol/l.
Traumatic factors of sensorineural hearing loss.
Sensorineural hearing loss can be a consequence of head trauma, as well as acoustic trauma, barotrauma (damage to the walls of the tympanic cavity caused by changes in environmental pressure), exposure to vibration, prolonged exposure to noise (occupational sensorineural hearing loss). Traumatic factors can also include birth injuries during the use of obstetric aids.
Age factor of sensorineural hearing loss.
Presbycusis , the so-called senile hearing loss, is associated with atrophy of the auditory analyzer during natural aging.
Hereditary factors of sensorineural hearing loss.
Genetically determined sensorineural hearing loss can appear from birth or at any later age. It can be isolated (manifest only as sensorineural hearing loss) or syndromic (exist along with other genetic abnormalities). There are more than 300 different genetic diseases with manifestations of sensorineural hearing loss. Hearing loss can be a dominant trait, or, more often, recessive and appear even after 6-9 generations.
Immune factors of sensorineural hearing loss.
Sensorineural hearing loss can be a complication or even a primary symptom of some autoimmune diseases, such as multiple sclerosis. In addition, in recent decades, scientists have discovered immunoglobulins in the inner ear, which indicates the presence of an immune system in the inner ear. Therefore, acute or progressive sensorineural hearing loss can sometimes manifest itself as an independent autoimmune disease.
Sensorineural hearing loss can result from malignant or benign brain tumors.
Thus, for different causes and levels of damage to the auditory analyzer, the pathogenesis, and therefore the treatment tactics, will be different, but without treatment, ultimately all factors lead to degenerative-atrophic changes in the tissues of the auditory analyzer.
How does the disease manifest itself?
Hearing problems can manifest themselves clearly or develop unnoticed by the patient. Acute sensorineural hearing loss is characterized by a sudden loss or progressive decrease in hearing in one or both ears, as well as one or a combination of the following symptoms:
- tinnitus of various types (high-frequency ringing or squeaking, low-frequency noise, etc.);
- vestibular dysfunctions (dizziness, nausea, vomiting, coordination problems, etc.);
- autonomic dysfunctions (sweating, rapid heartbeat, changes in blood pressure, etc.).
At the beginning of the development of chronic pathology, the clinical picture may be erased. The patient should be alert to the following situations:
- during a regular or telephone conversation you constantly have to ask again;
- there are difficulties communicating in an environment with background noise (on the street, in public places, etc.);
- understanding the interlocutor requires observing his lips;
- There are regular problems with identifying the source of noise.
The attention of loved ones should be attracted by oddities in a conversation (for example, a person hears words incorrectly or does not catch the meaning of what was said), watching TV at excessive volume, lack of reaction to events accompanied by noise (outside the patient’s field of view), and others.
Symptoms
When hearing loss is suspected to be due to a condition such as sensorineural hearing loss, symptoms will help determine the correct diagnosis. In this case, typical symptoms are:
- Sudden loss of hearing on one or both sides. The person indicates that he has become worse at understanding speech and perceiving high-frequency sounds;
- The appearance of tinnitus. This is not a permanent symptom. But it may indicate the cause of decreased hearing - acute injury, acute disruption of blood flow in the artery of the labyrinth, intoxication.
Qualified doctors who work in the Nearmedic clinic network necessarily assess the presence of risk factors. To do this, they ask the patient targeted questions:
- Do you have any relatives in your family who suffer from hearing loss?
- Is the work associated with high noise production conditions?
- Have you had any dangerous infections in the near future (measles, mumps, flu, meningitis, etc.)?
- Have you taken drugs from the ototoxic group (see above)?
Only after this comes the stage of objective examination. The otolaryngologist has an otoscope at his disposal during the appointment. This is a device that allows you to precisely examine the outer parts of the ear and the eardrum. It is not possible to look into the internal sections, but based on the condition of the peripheral sections, it is possible to identify some causes of decreased hearing - inflammation, degenerative processes, etc.
At the same time, the doctor evaluates the symmetry of the face. This sign allows us to exclude the involvement of cranial nerves in the pathological process, which is especially often observed with herpes infection.
Where to go if you have symptoms of hearing loss?
The diagnosis of sensorineural hearing loss is carried out by an otolaryngologist or audiologist. The first stage includes a survey, medical history and examination of the ears using a special device.
Laboratory examination involves a general blood test; according to indications, a coagulogram, blood biochemistry, and hormone tests are prescribed. Instrumental diagnostics includes the following options for a comprehensive hearing test:
- tests with whispered and spoken speech;
- tuning fork tests;
- pure tone threshold audiometry;
- impedancemetry;
- recording of auditory evoked potentials;
- otoacoustic emissions;
- extratympanic electrocochleography.
To assess hemodynamics in the structures of the auditory analyzer, duplex scanning of the brachiocephalic vessels is prescribed. To exclude serious causes of hearing loss (complications of injury, vascular pathology, tumor, etc.), CT and/or MRI of the head and neck are performed.
Treatment of sensorineural hearing loss at the Yauza Clinical Hospital
Specialists at the Yauza Clinical Hospital provide comprehensive treatment for sensorineural hearing loss. The doctor may prescribe intravenous or intramuscular administration of medications, administration of medications directly into the tympanic cavity, and various physiotherapeutic treatment methods are indicated. In some cases, treatment by related specialists (cardiologist, neurologist, neurosurgeon) may be necessary. Sometimes hearing aids are recommended for the patient. Children with congenital hearing loss are advised to consult a geneticist.
You can see prices for services
How is sensorineural hearing loss treated?
In accordance with clinical recommendations, acute sensorineural hearing loss is treated under the close supervision of an audiologist, who dynamically evaluates the effectiveness of therapy and, if necessary, carries out its correction. Treatment options include:
- hearing-friendly mode;
- hormone therapy;
- complex therapy with drugs to improve microcirculation and rheological properties of blood, antioxidants and antihypoxants.
In chronic sensorineural hearing loss, concomitant diseases are treated first. Twice a year, the patient must undergo courses of drug treatment using drugs to improve intracerebral and labyrinthine circulation and correct metabolism. At the same time, hearing aids are provided using a hearing aid.
The unsatisfactory effectiveness of hearing aids in severe sensorineural hearing loss is the reason for cochlear implantation.
Audiologists at the Ear, Nose and Throat Clinic successfully diagnose and treat sensorineural (sensorineural) forms of hearing loss. The clinic has equipment to conduct a complete diagnosis of hearing pathologies. The treatment program is drawn up taking into account the cause and characteristics of the development of disorders. Hearing aid is provided according to indications. Doctors at our medical center provide care to both adults and young patients.
Causes
When the number of normally functioning nerve cells in the sound-receiving part of the hearing organ decreases, sensorineural hearing loss develops. The reasons that lead to this are varied. It can be:
- Infections. Particularly significant among them are:
- Influenza and parainfluenza;
- Measles infection;
- Tick-borne encephalitis;
- Bacterial meningitis;
- Diphtheria infection;
- Scarlet fever;
- Syphilitic lesion.
- Toxic substances:
- Alcohol poisoning;
- Long-term intake of industrial poisons into the body;
- The use of drugs that exhibit ototoxic properties (some types of antibiotics, diuretics).
- Cardiovascular pathologies:
- Arterial hypertension;
- Poor cerebral circulation in the vertebrobasilar zone;
- Thrombosis.
- Diseases of the cervical spine:
- Arthrosis between the joints of the cervical vertebrae (from the first to the fourth);
- Slipping of the cervical vertebrae from each other (spondylolisthesis).
- Genetically determined increased sensitivity to damaging environmental factors (for example, vibration, sounds, etc.).
Therefore, unilateral and bilateral sensorineural hearing loss occurs:
- Genetic;
- Hereditarily determined (it is realized in the presence of certain genes that cause the development of pathology only when exposed to unfavorable factors);
- Acquired.