The use of β-adrenergic blockers (BABs) in the treatment of arterial hypertension (AH) remains one of the controversial positions in modern recommendations today. The question of the place of beta blockers in the treatment of hypertension is resolved in different ways, but the European Society of Cardiology classifies them as first-line drugs. There is much concern about the adverse metabolic effects associated with some drugs in this group. When using them, it is possible to increase blood lipid levels and reduce tissue sensitivity to insulin. However, an increase in heart rate (HR) often accompanies the presence of metabolic disorders - diabetes mellitus (DM), metabolic syndrome (MS) - and serves as a reflection of the constant sympathetic stimulation characteristic of these conditions. Tachycardia can be not only a marker, but also a predictor of the onset of diabetes and MS.
Prospective studies have shown a close relationship between increased blood pressure (BP) and the development of diabetes [1]. This makes the problem of blocking the sympathetic nervous system especially relevant in people with prediabetes and metabolic disorders. The 2013 recommendations of the European Society of Cardiology and the European Society of Hypertension included beta blockers with vasodilating properties among the drugs approved for use by patients with MS. Among these are celiprolol, carvedilol and nebivolol [2]. These drugs can reduce central aortic pressure and arterial stiffness. A drug such as nebivolol, which belongs to the 3rd generation beta blocker, is practically devoid of adverse metabolic effects.
Currently, highly effective generic drugs of nebivolol are registered in Russia, one of which is the 3rd generation cardioselective β-blocker drug Nevotenz (manufactured by ACTAVIS Ltd.). For this drug, the main indications for use are the treatment of arterial hypertension (AH), the prevention of attacks of stable angina in coronary artery disease (CHD) and the treatment of chronic heart failure (CHF) (as part of combination therapy).
This review examines the main issues related to the use of nebivolol drugs in patients with hypertension.
Pharmacokinetics and pharmacodynamics of nebivolol
A special feature of nebivolol is its ability to stimulate the synthesis of nitric oxide (NO) by the endothelium. This effect of the drug is associated with its effect on type 3 β-adrenergic receptors. Probably, their stimulation causes the release of NO by the endothelium. In atrial tissue, this receptor subtype is involved in the regulation of ion channels. The functions of these receptors in adipose tissue include the regulation of lipolysis and carbohydrate metabolism. An increase in NO synthesis promotes vasodilation, and therefore creates conditions for the organoprotective effects of nebivolol and its good tolerability. The contribution of the NO synthesis-enhancing effects of nebivolol has been proven in several experimental studies. One study compared the vasodilation induced by labetalol, nebivolol, and propranolol in radial artery fragments. All beta blockers caused significant changes in vascular tone. At the same time, NG-nitro-L-arginine ester blocked only vasodilation caused by the use of nebivolol, which indicates the presence of an additional mechanism of vasodilation associated with the NO system [3]. An experiment on cell culture showed that nebivolol, unlike metoprolol, normalizes the processes of cell proliferation and mitosis, improves endothelial function and NO-dependent vasodilation [4].
Evidence of an additional mechanism of action of nebivolol on the modulation of NO release includes a study of the effectiveness of this beta blocker in patients with impaired autonomic regulation of blood pressure. The increase in blood pressure in these patients is not associated with activation of the sympathetic nervous system (SNS). In a small group of such patients, the effectiveness of nebivolol and metoprolol was compared. Sildenafil was used as a “positive” control. A decrease in blood pressure was recorded in patients receiving nebivolol and sildenafil, which suggests a common mechanism of their action caused by NO activity [5].
The advantages of nebivolol include its favorable pharmacokinetic profile. The drug has good bioavailability and is quickly absorbed when taken orally. At the same time, a fairly long half-life (12–19 hours) provides the possibility of a single dose per day and a sufficient duration of the hypotensive effect.
The use of nebivolol in the treatment of hypertension
The effectiveness of nebivolol in the treatment of hypertension has been well studied. For the treatment of hypertension, doses of 5–10 mg/day are most often used, but in clinical studies the drug was prescribed at a daily dose of up to 40 mg.
In a placebo-controlled study of nebivolol in patients with stage 1-2 hypertension, it was shown that nebivolol therapy leads to a decrease in systolic and diastolic blood pressure by an average of 12.3 mm Hg, and heart rate decreases by 12.8 beats/min. The rate of discontinuation of treatment with nebivolol due to side effects was low and comparable to the placebo group - 1.4% [6]. Discontinuation of nebovolol does not lead to a sharp increase in blood pressure and does not cause symptoms of rebound hypertension [7].
Nebivolol has a convenient dosage regimen – once a day. It is most rational to take the drug in the evening. A randomized small study in a group of 42 patients with hypertension compared two regimens of nebivolol - morning and evening. According to 24-hour blood pressure monitoring data, with both regimens of taking the drug, the average daily, average daily and average night blood pressure values decreased equally. With the evening regimen of nebivolol, it was possible to control the morning rise in blood pressure to a greater extent, and the morning values of systolic blood pressure were lower [8].
There are a number of studies in which the effectiveness of nebivolol was compared with that of other biologically active agents. When comparing the effectiveness of metoprolol and nebivolol in patients with stage 1 hypertension, it was revealed that blood pressure decreased equally at rest and during the stress test. The rate of rise in blood pressure during exercise also did not differ significantly [9].
In a group of 138 patients with stage 1 and 2 hypertension, the effectiveness of therapy with nebivolol and atenolol was compared. Nebivolol was prescribed at a dose of 5 mg/day, atenolol at a dose of 50 mg/day. If the effectiveness was insufficient, the dose of atenolol was increased to 100 mg/day. After 6 weeks of therapy, hydrochlorothiazide could be added to treatment if necessary. At the end of treatment, blood pressure (central aortic and peripheral) did not differ significantly between the two treatment groups. In the atenolol group there was a greater need for diuretic use. Nebivolol, unlike atenolol, did not worsen the augmentation index [10].
In another study of patients with hypertension, when comparing the effectiveness of nebivolol and atenolol, it turned out that while taking nebivolol, metabolic parameters did not change, but while taking atenolol, there was an increase in lipid and blood sugar levels [11].
In the group of patients with stage 1 hypertension, the effectiveness of nebivolol at a dose of 5 mg/day and carvedilol 25 mg 2 times a day was compared. The reduction in systolic and diastolic blood pressure and heart rate were similar in both groups. Heart rate at the end of treatment was lower in the nebivolol group, but the differences were not statistically significant. In both groups, an improvement in myocardial diastolic function was noted, somewhat more pronounced in the nebivolol group [12].
The randomized multicenter study NEBIS (Nebivolol, Bisoprolol Multicenter Study) compared the effectiveness of nebivolol and bisoprolol. The study included patients with hypertension whose systolic blood pressure was no higher than 180 mm Hg and diastolic blood pressure from 95 to 110 mm Hg during the 4-week washout period. 273 patients were randomized to treatment with nebivolol 5 mg/day or bisoprolol 5 mg/day. After 12 weeks of treatment, similar reductions in systolic and diastolic blood pressure were recorded (by 15.7 mmHg in the nebivolol group and -16.0 mmHg in the bisoprolol group). The proportion of patients who responded well to therapy was slightly higher in the group receiving nebivolol (92%) compared to the bisoprolol group (89.6%), although the differences were not significant. In the nebivolol group, significantly fewer side effects of therapy were recorded (in 5.8% of patients) than in the bisoprolol group (8.9%)[13].
Nebivolol can be used as a drug for combination therapy. Several studies have used it in combination with renin-angiotensin-aldosterone system (RAAS) blockers.
A randomized multicenter study examined the effectiveness of nebivolol in women with hypertension and insufficient response to lisinopril or losartan; 491 patients with initial blood pressure 163/98 mm Hg. nebivolol at a dose of 5–40 mg/day or placebo was added to therapy. Nebivolol caused a significant decrease in diastolic blood pressure compared to the placebo group and a more pronounced, but non-significant decrease in systolic blood pressure [14].
An open-label study assessed the effectiveness of a free combination of nebivolol and valsartan. The drugs were initially prescribed at a dose of 5/160 mg, and if necessary, the doses were doubled. The target reduction in blood pressure was achieved in 60.9% (489 out of 810) of patients; 8.4% of patients refused treatment due to insufficient effectiveness of the combination. The average reduction in blood pressure was 25.5 for systolic and 19 mmHg. for diastolic [15].
The drug is well tolerated by patients. The incidence of side effects of therapy is low. A meta-analysis of data from three placebo-controlled studies analyzed the effectiveness and safety of nebivolol in the treatment of hypertension. In total, the analysis included data from 1811 patients receiving nebivolol in doses from 5 to 40 mg/day. The average decrease in systolic blood pressure was 12.4 mm Hg, diastolic blood pressure – 11.1 mm Hg, heart rate – 9.2 beats/min. The most common side effects included headache (7.1%), dizziness (3.6%), nasopharyngitis (3.1%) [16]. Nebivolol was better tolerated than other beta blockers. A small randomized trial compared the effectiveness of two beta blockers, nebivolol and atenolol, in patients with hypertension. With the same hypotensive effect, drug tolerability varied significantly: in the atenolol group, side effects were recorded in 36.8% of patients, in the nebivolol group - in 12% [17].
The good efficacy and tolerability of the drug, a convenient dosage regimen help to significantly solve the problem of patient adherence to treatment. Based on the analysis of US electronic databases, an analysis of patients' adherence to therapy with various beta blockers was carried out.
Based on 173.2 thousand case histories, it was revealed that the rate of discontinuation of treatment with nebivolol is 8% less than atenolol and carvedilol, and 20% less than the entire group of other beta blockers. The frequency of replacement of antihypertensive drugs while taking the drug was 12–22% less than when using other beta blockers [18].
Another analysis compared adherence to nebivolol and therapy with a drug of another pharmacological group (the diuretic hydrochlorothiazide) in patients who were prescribed antihypertensive therapy for the first time. Among patients prescribed nebivolol, the proportion remaining on this treatment was higher after 12 months (76 vs. 70%) and the period during which patients remained on this drug was longer (273 vs. 245 days, respectively) [19].
Nebivolol is the preferred drug from a pharmacoeconomics point of view. A pharmacoeconomic study compared the costs of treating hypertension using nebivolol at doses of 2.5, 5 and 10 mg/day and metoprolol succinate at doses of 25, 50 and 100 mg/day. Cost of reducing blood pressure by 1 mmHg. was significantly lower with nebivolol therapy [20].
Another pharmacoeconomic study recruited patients treated with metoprolol for at least 6 months and then started on nebivolol for at least 6 months. A total of 2259 patients were selected for the study. Switching to nebivolol was associated with a 33% reduction in total hospitalizations (p<0.01), a 60% reduction in cardiovascular hospitalizations (p<0.01), and a 7% reduction in the number of physician visits (p<0.01). ). At the same time, drug costs increased, but overall treatment costs decreased, and more significantly [21].
Use of nebivolol in patients with hypertension and metabolic disorders
There is evidence of good efficacy and the absence of adverse metabolic effects of nebivolol in the treatment of patients with diabetes, prediabetes and MS.
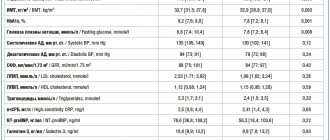
An open post-marketing study examined the effectiveness and safety of nebivolol in patients with hypertension and diabetes: 510 patients received nebivolol therapy for 4 months. A significant decrease in blood pressure and a decrease in heart rate were recorded. There was no significant change in high-density lipoprotein cholesterol or triglyceride levels. A significant decrease in the level of glucose, total cholesterol, and low-density lipoprotein cholesterol was noted [22].
In a group of 233 patients with newly diagnosed hypertension of 1-2 degrees, it was shown that the use of nebivolol, even in combination with hydrochlorothiazide, does not significantly change the state of carbohydrate and lipid metabolism [23].
A post-marketing open-label study assessed the effectiveness of nebivolol in patients with hypertension and diabetes. In total, the drug was prescribed to 2838 patients, the majority (85%) of whom received nebivolol at a dose of 5 mg/day. With the addition of nebivolol to therapy, blood pressure decreased from 156/92 to 135/81 mmHg. Heart rate decreased significantly. The decrease in blood pressure was accompanied by an improvement in metabolic parameters - lipid metabolism, glycated hemoglobin, microalbuminuria [24].
A group of 531 patients with hypertension, diabetes and MS showed that the use of nebivolol promotes better blood pressure control, especially among people under 40 years of age. At older ages, a decrease in systolic blood pressure was observed to a greater extent with an insufficient decrease in diastolic blood pressure. In addition, nebivolol therapy has been shown to promote weight loss, which may be due to the effect of nebivolol on β3-adrenergic receptors [25].
Nebivolol can be used in this group of patients in combination therapy to create additional hypotensive effect. In patients with type 2 diabetes and hypertension who received therapy with maximum doses of RAAS blockers, the effectiveness of metoprolol and nebivolol was compared. Both drugs were prescribed as 2nd line drugs. Both groups showed the same decrease in peripheral blood pressure. Central systolic blood pressure decreased only in the nebivolol group. Augmentation index and pulse wave velocity did not differ significantly between groups. In the metoprolol group, a deterioration in carbohydrate metabolism was recorded. Metabolic parameters did not change significantly in the nebivolol group [26].
We assessed the effect of nebivolol and metoprolol on the state of the endothelium in patients with diabetes. Nebivolol was prescribed at a dose of 5 mg/day, metoprolol – 100 mg/day. To achieve target blood pressure, a diuretic was added to therapy if necessary. Both groups achieved the same hypotensive effect. During treatment with nebivolol, the level of the endothelial dysfunction marker asymmetric dimethylarginine did not change significantly, but during treatment with metoprolol it increased by 36% [27].
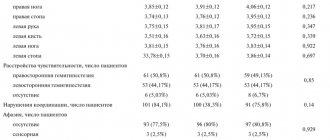
A multicenter study examined the effect of nebivolol on the state of carbohydrate metabolism in patients with hypertension and prediabetes who received basic therapy with RAAS blockers and did not achieve target blood pressure. Patients were randomized to receive nebivolol (223 patients), hydrochlorothiazide (212 patients), or placebo (102 patients). The addition of nebivolol and hydrochlorothiazide created a significant reduction in SBP compared to the placebo group. The area under the curve of the glucose tolerance test did not change in the nebivolol group and increased with hydrochlorothiazide. The proportion of patients in the hydrochlorothiazide group who stopped treatment was higher than in the nebivolol group. Thus, this drug is safer and better tolerated by patients with prediabetes [28].
The metabolic effects of metoprolol at a dose of 100 mg/day and nebivolol at a dose of 5 mg/day were compared in 46 patients with MS. The dynamics of metabolic parameters were assessed 12 weeks from the start of treatment. Nebivolol did not significantly change tissue sensitivity to insulin, levels of oxidative stress markers, and levels of plasminogen activator inhibitor. During treatment with metoprolol, a significant decrease in the index of tissue sensitivity to insulin and an increase in the level of plasminogen activator inhibitor and F2-isoprostane were noted [29].
Among patients with MS, the majority of patients have sleep apnea syndrome. In this group of patients, nebivolol at a dose of 5 mg reduced blood pressure in the same way as valsartan at a dose of 80 mg 2 times a day. Nebivolol also caused a decrease in heart rate. The sleep apnea index, according to polysomnography, did not change significantly in any of the groups [30].
The effect of nebivolol on the state of target organs in hypertension
Nebivolol has angio- and organoprotective properties associated with a vasodilating effect. It has been shown that therapy with nebivolol can help reduce left ventricular hypertrophy (LVH), aortic stiffness, and central blood pressure. In terms of the degree of organ protection, nebivolol is not inferior even to RAAS blockers. In a group of 106 patients with stage 1 and 2 hypertension and LVH, we compared the dynamics of left ventricular myocardial mass index (LVMI) during treatment with nebivolol at a dose of 5 mg/day and ramipril at a dose of 2.5 mg/day. If necessary, diuretics were added to treatment to normalize blood pressure. In the ramipril group, 97% of patients received a diuretic at the end of treatment, in the nebivolol group – 92%. LVMI 39 months after the start of treatment with nebivolol was 17 g/m2 less than with ramipril [31].
A study involving 160 patients with hypertension compared the effectiveness of nebivolol and irbesartan. Antihypertensive efficacy, as well as left atrial volume and deformation were assessed. Tissue Dopplerography was performed on the 6th and 12th months from the start of treatment. There were no significant differences in the effectiveness of nebivolol and irbesartan in lowering blood pressure, as well as in the effect on diastolic function [32].
A small study in a group of 85 patients compared the dynamics of LVH in patients with hypertension during treatment with irbesartan, carvedilol and nebivolol. During therapy with carvedilol and irbesartan, after 3 months of treatment, no significant changes in LVMI were observed; at the 6th and 12th months, the decrease in LVH was significant. During treatment with nebivolol, a decrease in LVMI was registered already by the 3rd month of therapy, and by the 12th month this dynamics was most pronounced. Thus, nebivolol is slightly more effective compared to carvedilol and irbesartan [33].
The effect of nebivolol on myocardial health was also studied in the echocardiographic substudy of the SENIORS protocol. This protocol demonstrated the effectiveness of nebivolol in patients over 70 years of age with heart failure. An echocardiographic substudy of patients with systolic myocardial dysfunction showed an increase in ejection fraction by 4.6% and a decrease in end-systolic volume of the left ventricle by 28.5 ml [34].
The cardioprotective properties of nebivolol appear to be responsible for the effectiveness of this drug in the treatment of heart failure with preserved ejection fraction, which often complicates the course of hypertension. In the SENIORS study, of the 2111 patients included, 752 had preserved (more than 35%) ejection fraction. During follow-up, 235 (31.2%) patients experienced adverse outcomes (death or cardiovascular hospitalization). As in general, in the study of patients with preserved ejection fraction, a reduction in the risk of the primary (by 19%) and secondary endpoints was recorded [35].
Of particular interest are the vascular effects of nebivolol. The use of nebivolol in patients with hypertension helps to improve the parameters of aortic stiffness. Taking nebivolol at a dose of 5 mg leads to a significant decrease in mean and pulse pressure in the aorta, pressure and augmentation index [36].
A randomized trial of a small group of 50 patients with prehypertension showed that treatment with nebivolol 5 mg significantly improved central hemodynamic parameters compared with placebo. There was a significant decrease in central pressure in the aorta - systolic, diastolic and mean. In addition, urinary excretion of nitrates and nitrites increased during nebivolol therapy [37].
In a group of 85 patients with newly diagnosed and previously untreated hypertension, the effectiveness of nebivolol and olmesartan was compared. The dynamics of blood pressure, the state of endothelial function according to the degree of increase in vasodilation of the brachial artery and the level of several markers of endothelial damage (plasminogen activator inhibitor, NO, C-reactive protein) were assessed. At the end of treatment, the decrease in blood pressure was significant and did not differ significantly in the nebivolol and olmesartan groups. Endothelial function improved, and levels of markers of endothelial damage decreased significantly. There were also no differences in the effectiveness of the drugs [38].
In a comparative randomized study, it was shown that combinations of irbesartan and a diuretic and nebivolol and a diuretic during 8 weeks of therapy equally reduced brachial artery blood pressure. There were also no significant differences in the dynamics of central pressure, pulse wave velocity, augmentation index and endothelial function [39].
Conclusion
Thus, the 3rd generation cardioselective β-blockers nebivolol, one of which is the drug Nevotenz (manufacturer: ACTAVIS Ltd.). has a number of significant advantages over other drugs in this group. They have a dual mechanism of action: peripheral vasodilation and high cardioselectivity. The convenient regimen of using the drug (once a day), high safety, good tolerability and affordable cost of treatment help solve the problem of patient adherence to therapy during long-term use. All this creates the prerequisites for the high effectiveness of the drug. The most interesting properties of nebivolol are to influence endothelial function and enhance NO synthesis, which creates conditions for organ protection. The use of this beta blocker is also possible for patients with high-risk hypertension - with concomitant diabetes mellitus and metabolic syndrome.
High effectiveness of nebivolol and improvement in the quality of life of patients
The article analyzes the results of studies on the antihypertensive effectiveness of nebivolol. It has been shown that the use of the drug reduces systolic and diastolic blood pressure, cholesterol and low-density lipoprotein levels. Nebivolol does not have a negative effect on lipid and carbohydrate metabolism, which is why it is the drug of choice in patients with arterial hypertension in combination with metabolic syndrome, obesity, and diabetes mellitus. The good hypotensive effect of nebivolol is considered on a specific example of a patient with significant damage to the coronary arteries, suffering from angina pectoris of the 2nd functional class, hypertension with blood pressure rising to 190/100 mm Hg. Art. and ventricular cardiac arrhythmias. Changing previously ineffective antihypertensive, antiarrhythmic and antianginal therapy to nebivolol made it possible to stabilize the patient's condition before stenting. The expansion of physical activity after stenting led to the need to increase the dose of nebivolol and made it possible to achieve an optimal hypotensive effect over the next five years of follow-up.
In cardiological practice, beta-blockers remain one of the most effective drugs for patients in whom sympathoadrenal activation is a pathogenetically significant mechanism.
A number of large multicenter studies, in particular LIFE and ASCOT, are devoted to studying the possibilities of antihypertensive therapy with beta-blockers. The results of these studies demonstrated that, with regard to the impact on the prognosis of arterial hypertension (AH), antihypertensive therapy with atenolol is less effective than therapy with angiotensin-converting enzyme inhibitors, calcium channel blockers and angiotensin receptor blockers [1, 2]. Based on these data, beta-blockers were excluded from the 2006 British National Guidelines for the Treatment of Hypertension as first-line antihypertensive drugs.
It is obvious that different generations of beta-blockers have different effects on the course of hypertension [3–6]. As shown by the results of the study by LH Lindholm et al. [7], in terms of reducing the risk of stroke, atenolol is significantly inferior to antihypertensive drugs of other groups. At the same time, according to a meta-analysis of 22 randomized trials conducted by S. Bangalore et al., when beta-blockers were used as antihypertensive agents, there was a decrease in the risk of all cardiovascular events in proportion to the decrease in heart rate (HR) [8].
Side effects of beta-blockers of the first generations, which include atenolol, also significantly narrow the scope of their use as antihypertensive drugs. It was the unfavorable effect on carbohydrate and lipid metabolism (increased levels of glucose and blood lipids) that limited the use of beta-blockers in the recommendations of the European Society of Cardiology for the treatment of arterial hypertension in 2007 [9]. Moreover, the recommendations specifically stipulate the irrationality of combining beta-blockers with thiazide diuretics in patients with diabetes mellitus and metabolic syndrome. However, in the version of these recommendations [10], presented at the congress of the European Society of Arterial Hypertension in June 2013, beta-blockers with vasodilating properties were highlighted: celiprolol, carvedilol and nebivolol. Based on this, since 2013, nebivolol, as a metabolically neutral, cardioselective beta-1-blocker with vasodilating properties and minimal effect on bronchial conduction, has been included in the recommendations of the European Society of Cardiology for the treatment of arterial hypertension. Thus, nebivolol retained its status as a special beta-blocker and rightfully remained one of the most commonly used antihypertensive and antianginal drugs.
High hypotensive, antianginal and, in some cases, good antiarrhythmic effects are primarily due to competitive selective blocking of beta-1 adrenergic receptors with minimal effect on alpha and beta 2 adrenergic receptors. With selective blockade, the receptors become inaccessible to catecholamines and thereby achieve negative chronotropic, inotropic, dromotropic and bathmotropic effects [5, 6].
Experience shows that a decrease in myocardial oxygen demand due to bradycardia and decreased contractility leads to a reduction in the frequency and severity of angina attacks, as well as an increase in exercise tolerance. Suppression of pathological automatism helps to achieve a good antiarrhythmic effect, which is most clearly expressed in patients with cardiac arrhythmias due to ischemic cardiopathy.
Antihypertensive effectiveness of nebivolol
One of the valuable effects of nebivolol (the drug Nebilet) is the modulation of the release of endothelial vasodilating factor (NO) by inducing the expression of NO synthase [11–16]. This hyperpolarizing factor produced by the endothelium promotes the opening of potassium channels, activation of Na+, K+-ATPase and the development of hyperpolarization of vascular smooth muscle cells. As a result of its production, the flow of calcium ions through calcium channels decreases and their flow into the sarcoplasmic reticulum increases, and the excretion of calcium from the cell increases. It is this biochemical chain that provides the vasodilation effect. Thus, modulation of NO release contributes to both the hypotensive and antianginal effects. According to experimental data obtained in animals, the drug is highly effective in preventing cardiovascular events [17].
An important property of the drug is the absence of a negative effect of nebivolol on carbohydrate and lipid metabolism. It has been proven that in patients with hypertension and impaired glucose tolerance, insulin sensitivity does not decrease [18–20], which is due to the lack of stimulation of alpha-adrenergic receptors, which cause arteriolospasm and insulin resistance. Therefore, nebivolol is the drug of choice in patients with metabolic syndrome, obesity, and diabetes mellitus.
Based on the beneficial effect of the drug on carbohydrate metabolism, data on its use in patients with diabetes mellitus are of interest. In a post-marketing study, LM van Bortel et al. 510 patients with hypertension and diabetes mellitus were treated with nebivolol for six months. It was shown that the use of the drug significantly reduced systolic and diastolic blood pressure (BP). When analyzing biochemical parameters, a significant decrease in the levels of blood glucose, total cholesterol and low-density lipoproteins (LDL) was noted. No significant dynamics in the levels of high-density lipoproteins and triglycerides was detected [21, 22]. Similar results were obtained in the AC Schmidt study, which also assessed the antihypertensive efficacy of nebivolol in 2838 patients with hypertension and diabetes mellitus. Monotherapy with nebivolol at a dose of 5 mg/day was effective in 85% of patients, which made it possible to achieve a significant reduction in systolic and diastolic blood pressure, levels of total cholesterol and LDL, microalbuminuria and glycosylated hemoglobin [23].
The results of a meta-analysis of three large placebo-controlled studies of the effectiveness of nebivolol in individuals with normal and overweight are also relevant in cardiological practice [24]. A significant reduction in diastolic blood pressure was achieved with the use of nebivolol at a dose of at least 2.5 mg/day, regardless of the patients’ body weight. At the same time, a significant decrease in systolic blood pressure was observed in individuals with normal body weight when using nebivolol at a dose of at least 5 mg/day, and in patients with excess body weight - at least 2.5 mg/day. Adverse metabolic effects of nebivolol were not reported in any of the study groups.
In a randomized study by N. Cağlar et al. compared the effects of ramipril and nebivolol on left ventricular myocardial hypertrophy in patients with hypertension. Patients were prescribed ramipril 2.5 mg/day or nebivolol 5 mg/day. Moreover, to achieve optimal blood pressure levels, most patients also received thiazide diuretics. The duration of therapy was 39 weeks, and at the end of the observation period the level of blood pressure in patients receiving ramipril and nebivolol did not differ significantly. In both groups, a decrease in left ventricular myocardial mass index was achieved, but it was higher in patients taking nebivolol [25]. Other studies [26, 27] also show similar results.
Considering the pharmacokinetic profile of nebivolol, one cannot fail to note its high bioavailability. The long (12–19 hours) half-life of the drug ensures the possibility of once daily dosing and long-term antihypertensive effectiveness.
As a rule, a dose of 5 mg/day is sufficient to achieve a hypotensive effect. The maximum daily dose is 10 mg/day. To date, many studies have been conducted to determine the optimal dose. Study results have demonstrated good tolerability of nebivolol, which is traditionally associated with its vasodilating properties [28–30].
As shown by an analysis of the results of three placebo-controlled studies involving over 1800 patients with hypertension, treatment with nebivolol led to a decrease in systolic blood pressure by 12.4 mm Hg. Art., diastolic - by 11.1 mm Hg. Art. The most common (7.3%) side effect was headache [30].
The results of a study of adherence to treatment with nebivolol are also interesting. Among 173,200 patients receiving beta-blockers, after 30 days of therapy, low adherence to treatment was about 8% and was significantly lower than in patients taking metoprolol, carvedilol and atenolol. Compliance with treatment was highest among patients receiving nebivolol. The study authors concluded that high adherence to therapy is associated with high efficacy and good tolerability of the drug [29].
Of particular interest are the results of the MP Hermans study, obtained from an analysis of the treatment of 1468 patients with hypertension who were prescribed nebivolol both as monotherapy and as a component of combination therapy. In addition to a good hypotensive effect, the use of nebivolol in all treatment options led to an improvement in the quality of life of patients, which was associated with good tolerability of the drug [28].
Clinical case
Today, any practicing cardiologist can present many clinical cases of long-term use of nebivolol. One of the most indicative clinical observations of the good effect of nebivolol is the case of patient B., 74 years old, hospitalized in the cardiology clinic of Clinical Hospital No. 1 of the First Moscow State Medical University. THEM. Sechenov with complaints of pressing pain in the heart area when walking, as well as frequent (every other day) rises in blood pressure to 190/100 mm Hg. Art. against the background of psycho-emotional stress. Increases in blood pressure in the patient have been observed over the past five years. He took antihypertensive drugs with good effect, but over the past year he frequently changed drugs and significantly increased their dosage. Pain in the heart area has occurred over the past three months.
Laboratory research methods did not reveal significant deviations from reference values.
Transthoracic echocardiography did not reveal significant valvular pathology, as well as disturbances in local and global contractility; Moderate left ventricular hypertrophy was detected.
Daily blood pressure monitoring demonstrated a clear need to replace antihypertensive therapy: average blood pressure values during the day were 145 and 93 mm Hg. Art., average heart rate – 85 per minute. The degree of reduction in systolic (9%) and diastolic (8%) blood pressure at night is insufficient. During the daytime, 47% of increased blood pressure values were detected. The maximum daytime blood pressure values were 186 and 95 mm Hg. Art., at night – 148 and 93 mm Hg. Art.
During daily recording of the electrocardiogram (ECG), a pronounced tendency towards sinus tachycardia (average heart rate - 84 per minute), frequent (more than 3000 per day) polymorphic single ventricular extrasystole with periods of bi- and trigeminy, ten ventricular couplets was revealed. Frequent notes by the patient in the diary “walking” and “stress” corresponded to periods of stable horizontal depression of the ST segment up to 1.5 mm in monitor lead II and periods of ventricular bigeminy.
During a stress treadmill test, when the heart rate reached above 100 per minute, a stable increasing horizontal depression of the ST segment in leads II, III, aVF, V4–6 up to 2 mm was recorded, accompanied by intense pressing pain in the heart area and induced ventricular bigeminy.
The patient underwent coronary angiography, which revealed 80% stenosis of the right coronary artery (RCA) and 70% stenosis of the obtuse marginal branch (BMA). The decision was made to implant stents in both stenotic arteries. However, due to the patient’s reluctance to undergo revascularization, we were able to observe the dynamics of blood pressure, anginal attacks and ventricular extrasystole while taking nebivolol 5 mg/day, Thrombo ACC 100 mg/day and rosuvastatin 20 mg/day for two months.
According to the patient, during the entire observation period, during therapy with nebivolol, pronounced positive dynamics were subjectively noted: anginal pain became less intense, occurring no more than once a week with very intense and/or long walking. During ambulatory 24-hour ECG recording in the usual active mode, the average heart rate was 58 beats per minute, the minimum was 49 beats per minute. A slight tendency to slow down atrioventricular conduction at night was recorded (PQ up to 190 ms). A total of 117 single monomorphic ventricular extrasystoles without episodes of allorhythmia were observed during therapy with nebivolol. No periods of ST segment depression were identified.
Repeated stress testing while taking nebivolol was carried out according to the previous protocol (Mod Bruce). The test result was also positive and was accompanied by pressing pain in the heart area, however, both ST segment depression in the same leads and an anginal attack occurred later and were less pronounced. Due to the recording of ischemic ECG dynamics and the development of an anginal attack during the stress test, the patient consented to stenting. Stents were implanted into the RCA and VTC. The patient was discharged from the hospital with a diagnosis of coronary heart disease: exertional angina of the 2nd functional class. Condition after implantation of Cypher stents in the RCA and VTC. Heart rhythm disturbances: single ventricular extrasystole. Hypertension stage II, 3rd degree increase, very high risk. Hypercholesterolemia. Duodenal ulcer in remission.”
Patient B.'s observation has continued over the past five years. Within a month after revascularization, we were able to reduce the dose of nebivolol to 2.5 mg/day. During control daily ECG recordings, no significant heart rhythm disturbances were detected. During control stress testing (once every six months), the ECG does not reveal ischemic dynamics, and anginal pain does not recur. According to the results of independent regular measurements and control 24-hour blood pressure monitoring, a good hypotensive effect of nebivolol has now been achieved. The patient notes rare (no more than once a month) rises in blood pressure up to 160/100 mm Hg. Art., usually associated with pronounced psycho-emotional stress.
Replacement of the drug Nebivolol
Oleg
October 22, 2021
Hello. I have been taking the drug Nebivolol for more than 3 years. Every day, in the morning, 2.5 mg. It was attributed to me for tachycardia and pressure surges. Half a year ago, I purposefully lost a lot of weight by 30 kg and against this background my blood pressure dropped significantly (from normal 125/85 to 105/65) and my pulse from my normal resting 80 to 59 at rest. I believe that in addition to everything, Nebivolol added an effect. Against this background, I periodically began to experience noise or ringing in my ear (2-3 times a day in different ears and as if stuffy). All this happened over the next 4 months. I decided to cut Nebivolol to 1.25 mg. And after a week, the incoming noise in the ear disappeared (average pressure became 115/75, and pulse 70), BUT. After another 2 weeks of this use, against the background of weight gain, the pressure began to jump: the average was 130/89. And in the evenings there were pressure surges up to 150/95 and the pulse was up to 100. Naturally, all this did not make me happy, but at that time it was very difficult to get to a specialist (due to COVID) and I had to return the dosage of 2.5 mg. every morning. The pressure surges stopped 2 weeks later and the blood pressure and pulse decreased. And so I gained weight again due to stress and my inability to cope with it. But everything would have been fine, only on top of everything else, symptoms that were unusual for me “came” to me: paresthesia. Either under the eye, then in the hand, then in the leg, and so on. Half a year of examinations (ultrasound of literally the whole body and MRI from head to toe), including ultrasound of the heart, dozens of consultations with neurologists did not yield results. Because in the vessels of the neck, arms and legs and everything else there is health. Only osteochondrosis and protrusions in the neck. But they told me that this is the case for the majority and my blood flow is not impaired and that my symptoms in this form are not specific to neurology at all. But just recently, one of the cardiologists told me that it is better not to take Nebivolol for so long (I have been taking it for more than 3 years), because many side effects may appear. And I decided to read the instructions for Nebivolol and saw there: paresthesia. I was surprised. It got me thinking. So I have a question for you: could this be from Nebivolol? How and what should I replace it with in order to keep my pressure surges under control? I don’t even know what to call it... Let’s say “labile” blood pressure. It is normal on average per day, but there are surges in the evening or during the day or in the morning - as it generally pleases