BCG: what is it?
The BCG vaccine is used to prevent severe forms of tuberculosis.
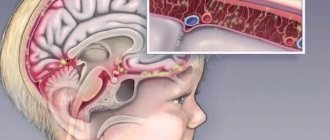
It also protects against the most dangerous complications if a person does get sick. Tuberculosis is a common infectious disease (Fig. 1). In the world, up to 10 million people fall ill with it every year, and up to 1.4 million people. dies from this disease. In Russia, the incidence of tuberculosis has been declining in recent years. In 2022 it amounted to 41.2 people. per 100,000 population, and mortality is 5.2 people. per 100,000 population. Despite this, tuberculosis infection remains dangerous, and BCG vaccination is important to protect against it.
Figure 1. General information about tuberculosis. Source:
The BCG vaccine is live. It contains live vaccine strains. They are obtained using weakened bovine tuberculosis bacilli Mycobacterium bovis.
M. bovis is a mycobacterium of the tuberculosis complex that can cause tuberculosis in humans in the same way as the main causative agent of the disease, Koch bacillus (Mycobacterium tuberculosis). Bovine tuberculosis bacillus and Koch's bacillus have a number of similarities and differences. M. bovis produces a similar immune response and can be weakened in vitro. This allows the strain to be used for the production of a live attenuated vaccine.
Back in 1908, the development of BCG began in France. The vaccine was named after the first letters of the surnames of its creators, Albert Calmette and Camille Guérin: Bacillus Calmette-Guérin or BCG. It was tested in 1921, but the tests were unsuccessful. Later it was transferred to the USSR. Since the 1950s, the mass use of BCG for vaccination began in the USSR and other countries. New vaccines are currently being developed, but for now BCG remains the only means of immunoprophylaxis against tuberculosis.
In countries where the incidence of tuberculosis is high, WHO recommends that all healthy newborns be vaccinated in the first days of life. Russia is one of such countries. In regions where the incidence of tuberculosis is decreasing or is low, vaccination against tuberculosis is carried out selectively, only for risk groups.
BCG vaccination: what it protects against, at what age it is given
The vaccine got its name from the English abbreviation – BCG (Bacillus Calmette-Guerin). It includes a live attenuated strain of bovine tuberculosis bacillus. This bacterium is not dangerous to humans, but forms immune protection against severe forms of tuberculosis (damage to the bones of the spine, meningitis, severe damage to internal organs) and the transition of latent carriage of bacilli to an active form of infection (pulmonary tuberculosis). Source: D.T. Levi, N.V. Alexandrova Vaccinal prevention of tuberculosis // BIOpreparations. Prevention, diagnosis, treatment, 2015, p. 4-8
Today, this vaccination is given in the maternity hospital, on the 4th day of life of a full-term baby, if there are no contraindications. Premature babies are also vaccinated with BCG, but they must weigh more than 2500 g and have no health problems. Subsequently, BCG revaccination is carried out at the ages of 7 and 14 years according to the results of tuberculin tests (Mantoux).
In our country, BCG vaccination is included in the compulsory vaccination schedule of the national calendar - it is recommended for all children. But not all countries support the idea of universal vaccination against tuberculosis at an early age. Some European countries and the United States have abandoned mass vaccination; they only vaccinate children at risk. This is explained by the low incidence of tuberculosis in these countries.
To whom and when do they do it?
The Russian national vaccination calendar recommends that all healthy newborn children be vaccinated against tuberculosis in the first days of life.
Further, Mantoux tests are performed annually to diagnose tuberculosis and detect infection with mycobacteria in children. This is a subcutaneous injection of tuberculin - a filtrate of killed cultures of Mycobacterium tuberculosis that have undergone special treatment. After the test, redness or a papule (solidification) may appear at the injection site. The reaction to tuberculin is assessed by its size (Fig. 2). If the test is negative (there is no severe redness or swelling at the injection site), then the child is healthy, and the doctor may recommend revaccination.
Figure 2. Assessment of response to tuberculin test. Source: MedPortal
Vaccination against tuberculosis can also be given to adults, but it is not as effective as in childhood. It is recommended to get vaccinated if a person is going to travel to a country with a high incidence of tuberculosis, or if he will have contact with patients. Vaccination is performed only if the tuberculin test gives a negative result.
Hepatitis B vaccine
Hepatitis B is a viral infection that is characterized by damage to liver cells followed by death. As well as a long course with frequent chronicity and resistance to treatment.
Hepatitis vaccination was introduced into the calendar relatively recently, approximately in the 80s of the last century. This late introduction of the vaccine into the national calendar is due to the peculiar structure of the virus and the frequent absence of a characteristic clinical picture in patients.
Why is it necessary to get vaccinated against hepatitis B?
Most adults recover on their own after contracting hepatitis. For some, the virus remains in the body and does not manifest itself in any way. Such asymptomatic carriage does not require treatment. Although the person remains infectious.
However, approximately 20% of infected adults and 80% of children develop the disease, causing inflammation and death of liver cells. After an acute process, fibrosis forms at the site of hepatocyte death. Cirrhosis of the liver may then develop with the possibility of tumor formation. The existing treatment takes a long time. The drugs have a pronounced toxic effect and are unable to completely remove the virus from the body, only to convert the disease into an inactive form.
When is the hepatitis B vaccine given?
According to the national calendar, the vaccine is given in the first 12 hours of life, then at 1 month and at 6 months. Children from risk groups are vaccinated four times. In the maternity hospital, then at 1,2 and 12 months. Children at risk include:
- born from mothers who are carriers of HBsAg (one of the components of the hepatitis B virus),
- from mothers of patients with viral hepatitis B,
- from mothers who do not have test results for hepatitis B markers,
- from mothers who use narcotic drugs or psychotropic substances,
- from families in which there is a carrier of HBsAg, or a patient with acute viral hepatitis B, as well as chronic viral hepatitis.
Previously unvaccinated children and adults not belonging to risk groups are vaccinated according to the same schedule - 0-1-6 months.
What is included in the hepatitis B vaccine?
The vaccine is a subunit vaccine. The main component is part of the virus shell. In addition, the vaccine contains an adjuvant (a substance that improves the production of immunity) - aluminum hydroxide, and a preservative thiomersal.
What happens after hepatitis B vaccination?
After completing the vaccination course (at 6 months for children not at risk), stable lifelong immunity is developed. The vaccine is almost 100% effective.
What complications can occur after hepatitis B vaccination?
This vaccine is one of the least reactogenic. Local reactions may be observed: redness, hardening at the injection site, swelling. General reactions: weakness, muscle pain, increased body temperature, high-pitched crying. All reactions resolve on their own and do not require treatment.
When should you not get vaccinated against hepatitis B?
- If a severe reaction has developed to the previous injection - an increase in body temperature above 40*C, swelling and redness at the injection site more than 8 cm in diameter.
- In children with severe immunodeficiencies due to HIV infection.
- In children with acute diseases, as well as in cases of exacerbation of chronic diseases, temporary medical diversion is indicated.
- In women during pregnancy and breastfeeding.
Carrying out BCG: according to the calendar and individually
In the absence of contraindications, healthy children are vaccinated according to the national calendar of preventive vaccinations twice:
- on days 3-7 of life before discharge from the hospital;
- at 6-7 years, if the tuberculin test is negative.
If there are contraindications, the vaccination is not given in the maternity hospital, but later, after discharge. In this case, a separate immunization schedule is drawn up for the child, planning it so that BCG is administered separately from all other vaccines. It is important to get vaccinated against tuberculosis as early as possible. If a child is weakened, underweight or has contraindications to the administration of the BCG vaccine, he is vaccinated with the BCG-M vaccine with a reduced content of live mycobacteria. This reduces the risk of complications.
BCG, tuberculosis and Mantoux test
The most dangerous forms of tuberculosis are miliary tuberculosis and tuberculous meningitis. They develop much more often when infected with Mycobacterium tuberculosis in the first years of life. BCG is effective in preventing these forms of tuberculosis in children in 75-86% of cases, and slightly lower in preventing other forms of tuberculosis.
Unvaccinated children have a much higher risk of developing tuberculosis than vaccinated children. In order to diagnose the disease in a timely manner, children are given a Mantoux or Diaskintest test.
Unvaccinated children undergo testing twice a year; for this purpose, there are orders 109 and 125n of the Ministry of Health.
If parents refuse to conduct a Mantoux test on their child, then according to the law, children may not be accepted into kindergarten, since there is no confidence that the child is completely healthy.
BCG vaccination reduces the risk of other diseases caused by mycobacteria, such as leprosy, Buruli ulcers and lymphadenitis caused by non-tuberculous mycobacteria.
By the way, Mantoux and rib are not interrelated. The child may have one of the manifestations, both at once, or neither. One does not affect the other.
Features of vaccination
It is important to carry out vaccination against tuberculosis as early as possible, in the first few days after birth. This will allow you to activate your immune system faster. If immunization is performed later, BCG vaccination cannot be combined with other vaccines. One month before and one month after vaccination against tuberculosis infection there should be no other vaccinations. An exception is vaccination against viral hepatitis B, which is performed in the maternity hospital on the first day of a child’s life.
When using the BCG vaccine, the correct technique for administering the drug is especially important. It is injected to a certain depth, strictly intradermally. Incorrect injection depth provokes local complications and reduces the effectiveness of vaccination. It is better if the vaccination is administered by medical staff in the maternity hospital. Nurses in maternity hospitals constantly carry out such vaccinations and do them correctly, and in addition, the child will remain under the constant supervision of doctors for some time after vaccination. No special preparation is needed for BCG vaccination.
What happens after the BCG vaccination?
After administration of the BCG vaccine, a number of changes occur at the injection site. About a month after vaccination, redness and thickening appear at the injection site. Then an abscess. It becomes covered with a crust, which then falls off, leaving behind a scar. This happens around six months. Sometimes the inflammation is so active that pus can be released from the wound. All these changes are normal and indicate that the baby is developing immunity. There is no need to do any manipulation with the wound during inflammation. It will live on its own when the time comes.
Contraindications for carrying out
Vaccination against tuberculosis cannot be done if the following contraindications exist:
- birth weight less than 2000 g;
- the presence of acute diseases (including intrauterine infection, severe damage to the nervous system, purulent-septic and other diseases);
- malignant neoplasms;
- primary immunodeficiency;
- use of immunosuppressants or radiation therapy (vaccination is performed 6 months or more after completion of therapy);
- generalized BCG infection in other children in the family;
- HIV infection in the child or his mother (if she did not take antiretroviral therapy).
Vaccination in these cases is carried out after removal of contraindications. The BCG-M vaccine can be used for it, for which the risk of complications is lower.
Tuberculosis vaccine BCG
FSUE NPO Microgen, Ministry of Health of the Russian Federation, Russia
Release form: 1 ampoule / 20 doses No. 5.
Vaccination schedule: once on 3-7 days after birth. Revaccination at 7 and 14 years of age.
INSTRUCTIONS FOR USE of dry tuberculosis BCG vaccine
The drug is a live mycobacteria of the BCG-1 vaccine strain, lyophilized in a 1.5% solution of monosodium glutamate. The porous mass is powdery or in the form of a white or creamy tablet. Hygroscopic. The vaccination dose contains 0.05 mg in 0.1 ml of solvent. Biological and immunological properties . Live mycobacteria of the BCG-1 strain, multiplying in the body of the vaccinated person, lead to the development of long-term immunity to tuberculosis. Purpose . Active specific prevention of tuberculosis. Directions for use and dosage . The BCG vaccine is used intradermally at a dose of 0.05 mg in a volume of 0.1 ml. Primary vaccination is carried out on healthy newborn children on days 3-7 of life. Children aged 7 and 14 years who have a negative reaction to the Mantoux test with 2 TE PPD-L are subject to revaccination. The reaction is considered negative in the complete absence of infiltration, hyperemia, or in the presence of a prick reaction (1 mm). Children infected with tuberculous mycobacteria who have a negative reaction to the Mantoux test are not subject to revaccination. The interval between the Mantoux test and revaccination should be at least 3 days and no more than 2 weeks. Vaccinations should be carried out by specially trained medical personnel of the maternity hospital (ward), department for nursing premature babies, children's clinics or feldsher-obstetric stations. Vaccination of newborns is carried out in the morning in a specially designated room after the children have been examined by a pediatrician. Vaccinations at home are prohibited. In clinics, the selection of children to be vaccinated is preliminarily carried out by a doctor (paramedic) with mandatory thermometry on the day of vaccination, taking into account medical contraindications and medical history. If necessary, consultations with medical specialists and blood and urine tests are carried out. The history of the newborn (medical record) indicates the date of vaccination, series and expiration date of the vaccine, company|manufacturer. For vaccination (re-vaccination), disposable sterile tuberculin syringes with a capacity of 1.0 ml with tightly fitting pistons and thin short needles with a short bevel are used. It is prohibited to use syringes and needles that have expired and needleless injectors. After each injection, a syringe with a needle and cotton swabs are soaked in a disinfectant solution (5% chloramine) and then centrally destroyed. It is prohibited to use instruments intended for vaccination against tuberculosis for other purposes. In the vaccination room, the vaccine is stored in the refrigerator (under lock and key) and diluted. Persons unrelated to BCG vaccination are not allowed into the vaccination room. To avoid contamination, it is unacceptable to combine tuberculosis vaccination with other parenteral procedures on the same day. Vaccine ampoules are carefully inspected before opening. The drug cannot be used: - if there is no label on the ampoule or if it is filled incorrectly; - expired; — in the presence of cracks and notches on the ampoule; - when the physical properties of the drug change (wrinkled tablet, change in color, etc.); - in the presence of foreign inclusions or flakes that do not break when shaken in the diluted preparation. The dry vaccine is diluted immediately before use with a sterile 0.9% sodium chloride solution attached to the vaccine. The solvent must be transparent, colorless and free of foreign inclusions. The neck and head of the ampoule are wiped with alcohol, the sealing area (head) is filed down and carefully broken off using tweezers. Then they file and break off the neck of the ampoule, wrapping the sawed end in a sterile gauze napkin. To obtain a dose of 0.05 mg of BCG in 0.1 ml, transfer 2 ml of 0.9% sodium chloride solution into an ampoule with a 20-dose vaccine using a sterile syringe (2.0 ml capacity with a long needle), and into an ampoule with 10- dose vaccine - 1 ml of 0.9% sodium chloride solution. The vaccine should completely dissolve within 1 minute after shaking 2-3 times. Precipitation or formation of flakes that do not break when shaken is not allowed. The diluted vaccine must be protected from sunlight and daylight (for example, a cylinder of black paper) and consumed within one hour after dilution. It is mandatory to maintain a protocol indicating the time of dilution and destruction of the vaccine ampoule. Unused vaccine is destroyed by autoclaving at 126° C for 30 minutes, immersing in a disinfectant solution (5% chloramine solution) for 60 minutes or boiling for 30 minutes. For one vaccination, 0.2 ml (2 doses) of the diluted vaccine is drawn up with a sterile syringe, then 0.1 ml of the vaccine is released through a needle into a sterile cotton swab to displace the air and bring the syringe piston to the desired graduation of -0.1 ml. Before each kit, the vaccine must be carefully mixed using a syringe 2-3 times. One syringe can only administer the vaccine to one child. The BCG vaccine is administered strictly intradermally at the border of the upper and middle third of the outer surface of the left shoulder after pre-treatment of the skin with 70° alcohol. The needle is inserted with the cut upward into the surface layer of the stretched skin. First, a small amount of the vaccine is injected to make sure that the needle enters exactly intradermally, and then the entire dose of the drug (only 0.1 ml). With the correct injection technique, a whitish papule with a diameter of 7-9 mm should form, usually disappearing after 15-20 minutes. Injecting the drug under the skin is unacceptable, as this may result in the formation of a cold abscess. It is prohibited to apply a bandage or treat the vaccine injection site with iodine or other disinfectant solutions. Reaction to introduction . At the site of intradermal injection of the BCG vaccine, a specific reaction develops in the form of a papule measuring 5-10 mm in diameter. In newborns, a normal vaccination reaction appears after 4-6 weeks. The reaction undergoes reverse development within 2-3 months, sometimes over a longer period. In those revaccinated, a local reaction develops after 1-2 weeks. The site of the reaction should be protected from mechanical irritation, especially during water procedures. In 90-95% of vaccinated people, a superficial scar up to 10.0 mm in diameter should form at the vaccination site. Complications after vaccination and revaccination are rare and are usually local in nature. Contraindications . Vaccination. 1. Prematurity - birth weight less than 2500 g. 2. Acute diseases. Vaccination is postponed until the end of acute manifestations of the disease and exacerbation of chronic diseases (intrauterine infection, purulent-septic diseases, moderate and severe hemolytic disease of newborns, severe damage to the nervous system with severe neurological symptoms, generalized skin lesions, etc.). 3. Immunodeficiency state (primary), malignant neoplasms. When prescribing immunosuppressants and radiation therapy, vaccination is carried out 6 months after the end of treatment. 4. Generalized BCG infection detected in other children in the family. 5. HIV infection in the mother. Children who were not vaccinated during the neonatal period receive the BCG-M vaccine after recovery. Children aged 2 months and older are first given the Mantoux test 2TE PPD-L and only those who are tuberculin-negative are vaccinated. Other preventive vaccinations can be carried out at an interval of at least 1 month before (with the exception of vaccinations against viral hepatitis B) and after BCG vaccination. Revaccination . 1. Acute infectious and non-infectious diseases, exacerbation of chronic diseases, including allergic ones. Vaccination is carried out 1 month after recovery or remission. 2. Immunodeficiency conditions, malignant blood diseases and neoplasms. When prescribing immunosuppressants and radiation therapy, vaccination is carried out no earlier than 6 months after the end of treatment. 3. Patients with tuberculosis, persons who have had tuberculosis and are infected with mycobacteria. 4. Positive and questionable Mantoux reaction with 2 TE PPD-L. 5. Complicated reactions to the previous administration of the BCG vaccine (keloid scar, lymphadenitis, etc.). In case of contact with infectious patients in the family, child care facility, etc. Vaccinations are carried out after the end of the quarantine period or the maximum incubation period for a given disease. Other preventive vaccinations can be carried out at an interval of at least 1 month before and after BCG revaccination. Persons temporarily exempt from vaccinations must be monitored and registered, and vaccinated after full recovery or removal of contraindications. If necessary, appropriate clinical and laboratory examinations are carried out. Release form. In ampoules containing 0.5 mg (10 doses) or 1.0 mg of the drug (20 doses) complete with a solvent - 0.9% sodium chloride solution, 1 or 2 ml per ampoule, respectively. One pack contains 5 ampoules of BCG vaccine and 5 ampoules of 0.9% sodium chloride solution (5 sets). Best before date . 2 years. A drug that has expired cannot be used. Storage and transportation conditions. Store the drug at a temperature not exceeding 8° C according to SP 3.3.2.028-95. Transportation by all types of transport at a temperature not exceeding 8° C according to SP 3.3.2.028-95. Complaint . All cases of unusual post-vaccination reactions, complications and discrepancies in the physical properties of the drug must be reported to the State Research Institute for Standardization and Control of Medical Biological Preparations named after. L.A. Tarasevich (121002, Moscow, Sivtsev Vrazhek, 41; tel./fax 241-39-22) and to the address of the manufacturer who manufactured the drug. In this case, a card (of complications) is drawn up with an exact indication of the series, expiration date of the BCG vaccine and the manufacturer.
← Back
What complications can occur after BCG vaccination?
Complications after this vaccination are divided into two categories:
- Severe complications associated with generalization (spread) of infection. The BCG vaccine is, as noted above, a live culture. Therefore, it can cause specific (i.e., related to the development of the tuberculosis process) complications. As a rule, such complications are associated with improper selection of children for vaccination. However, I would like to emphasize that the risk of such complications is much less than the risk of the disease in an unvaccinated child.
- Milder complications associated, among other things, with a violation of the vaccine administration technique or with a low-quality vaccine.
Among the main possible complications after BCG:
- Ulceration of the infiltrate. The area of compaction or thickening of tissue at the injection site (infiltrate) increases in diameter (more than 1 mm) and ulcerates; The ulcer is painless, with little discharge.
- Formation of subcutaneous infiltrate. The infiltrate does not form in the skin, but under the skin. It looks like a “ball” that can be felt under smooth, unchanged skin. This complication is associated with an excessively deep injection of the vaccine, and if you do not consult a doctor in time, the infiltrate may break through and the infection will enter the bloodstream.
- Formation of a keloid (rough scar). This is a fairly rare complication, and it occurs less frequently in newborns than in older children. It is a common hereditary disease in which any damage to the skin is accompanied by excessive growth of scar tissue. If a keloid forms after vaccination, the scar becomes bright, blood vessels are visible through it, and sometimes itching appears.
- Spread of infection to lymph nodes. In this case, enlarged, painless axillary lymph nodes are identified, which mothers most often notice when bathing their child. Such a lymph node is the size of a hazelnut, and sometimes the size of a chicken egg. Occasionally, the infection breaks through the skin and a fistula is formed, that is, a channel through which pus drains.
If any of the above complications, as well as other unusual phenomena, occur, you should immediately consult a doctor.
Vaccine as salvation
How is it possible to scientifically explain this relationship between statistics on coronavirus infection and the tuberculosis vaccine? After all, tuberculosis is caused by bacteria, and the causative agent of COVID-19 is a virus. As with cancer immunotherapy, there is no exact answer. Some doctors believe that the BCG vaccine trains the immune system and strengthens a person’s natural immunity to viral respiratory diseases.
“The hypothesis that widespread BCG vaccination reduces mortality from COVID-2019 requires scientific confirmation. Currently, science does not have basic information that would confirm the antigenic relationship between mycobacterium tuberculosis and the causative agent of COVID-2019,” comments Alexander Sergeev, Doctor of Medical Sciences, Professor, Deputy Director of the Center for Development and Implementation of NPO Microgen.
“Firstly, a more complete study of the statistics of the coronavirus outbreak is required. In particular, epidemic statistics are influenced by a lot of factors that must be taken into account: methods for counting infected and dead people in different countries, diagnostic approaches and capabilities, etc. Secondly, an analysis of the antigenic relationship between tuberculosis bacteria and the causative agent of COVID-2019 is required. If this is discovered, then it will be possible to draw further conclusions that the body’s immune response to BCG vaccination helps cope with coronavirus infection,” he said.
Scientists continue to study this mechanism. For example, a study is currently underway in Australia, in which 4 thousand doctors are participating. Half are vaccinated with BCG, the rest are given a placebo drug. The hypothesis that needs to be confirmed is that people vaccinated with the vaccine are more likely not to get coronavirus infection or the disease will be mild. If this is scientifically proven, then the BCG vaccination can be used until a special vaccine for COVID-2019 appears on the market. Dozens of laboratories around the world are now working on it. In Russia, testing of the domestic vaccine from Novosibirsk on volunteers will begin no later than June.
Every minute, the number of people infected with coronavirus in the world continues to grow. As of this writing, more than 1.44 million cases of COVID-19 have been confirmed. In Russia, 8,672 cases were identified, 580 patients were cured, and 63 people died. At the moment, the most effective thing we can do for our safety is quarantine and compliance with all hygiene rules.
Vaccination against tuberculosis: pros and cons
The BCG vaccine has been used for a long time, and it has a number of disadvantages, but so far it remains the most effective way to prevent tuberculosis.
At the same time, it is the effectiveness of immunoprophylaxis that causes the most controversy:
- The BCG vaccine does not prevent tuberculosis infection.
- If a person is already infected with Mycobacterium tuberculosis, the vaccine does not protect against the disease becoming active. According to WHO, a third of people worldwide are carriers of Mycobacterium tuberculosis.
- The immunity formed by the vaccine weakens over several years. Revaccination is not always effective, and because of this, adults are vulnerable to both primary infection and the transition of the latent form of tuberculosis to the active form.
- The BCG vaccine in children prevents up to 80% of severe forms of tuberculosis infection.
- Vaccination reduces the number of deaths associated with tuberculosis by 65%. The incidence of tuberculous meningitis is reduced by 64%, disseminated tuberculosis (with the formation of multiple lesions of lung tissue) - by 78%.
- Even if infected, those who have been vaccinated have a much milder course of the disease, with fewer complications.
The safety of the BCG vaccine is also controversial. Its use can indeed lead to a number of complications, but they occur very rarely. Local reactions associated with a violation of the drug administration technique are more common, but even these are not very common.
What is included in the BCG vaccine?
The vaccine contains mycobacterium bovis (bovine) and a solvent – monosodium glutamate. Bovis was chosen because it is similar in structure to Mycobacterium tuberculosis, but is safer. This microbe is grown on a special nutrient medium and is attenuated (weakened) through repeated division outside the body. This causes the bacterium to lose its ability to cause disease. The strain of bacteria included in the vaccine does not multiply uncontrollably. Its properties (the ability to provoke disease and the ability to create immunity) are constantly monitored during production. The strain used for the vaccine in Russia is considered one of the safest in the world. Somewhat later, the BCG-M vaccine, containing a smaller number of mycobacterial strains, was developed to vaccinate weakened children.