Compound
1 tablet contains the active substances guaifenesin and butamirate citrate in volumes of 100 mg and 4 mg, respectively; excipients are also present: colloidal silicon dioxide , glyceryl tribehenate , mannitol , magnesium stearate, MCC.
1 ml of Stoptussin drops contains the active substances guaifenesin and butamirate citrate in volumes of 100 mg and 4 mg, respectively; excipients: 96% ethanol - 0.3 g, purified water - 0.007 g, floral flavor (alpine flowers) - 0.002 g, liquid licorice extract - 0.003 g, polysorbate 80 - 0.001 g, propylene glycol - up to 1 ml.
Pharmacodynamics and pharmacokinetics
The drug is a combined antitussive and expectorant. The substance guaifenesin allows you to break down phlegm . This occurs due to increased secretion of the bronchial glands and decreased mucus viscosity. In turn, butamirate citrate can have an anesthetic effect on the patient’s throat, reducing cough .
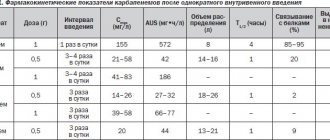
After the drug Stoptussin enters the body, it is immediately completely absorbed by it. At the same time, the connection of the substance with proteins and plasma is as much as 94%. As for guaifenesin , it is quickly absorbed from the gastrointestinal tract, despite the fact that the connection of this substance with proteins and plasma is insignificant.
Cough ranks high among the symptoms caused by pathology of the respiratory system. It should be considered not as a pathological symptom, but as a protective reaction of the body that creates optimal conditions for a person to exist. Nevertheless, quite often cough loses its physiological purpose, becomes chronic and turns into a factor that significantly reduces the patient’s quality of life [1, 2].
Depending on the duration of the cough, it can be acute, protracted or chronic. The most common causes of acute cough
are upper respiratory tract infections such as acute respiratory viral infections (ARVI), acute bacterial rhinosinusitis, whooping cough, exacerbation of chronic obstructive pulmonary diseases, allergic rhinitis. The most common cause of acute cough is viral infections of the upper respiratory tract. In patients with ARVI without treatment, the frequency of this symptom in the first 48 hours of the disease reaches 83%, and by the 14th day it decreases to 26%. Cough during ARVI is stimulated by the drainage of secretions from the nasopharynx and irritation of the mucous membrane of the pharynx and larynx. With adequate treatment for ARVI, the cough goes away without a trace. However, situations arise when the cough becomes protracted.
Persistent cough
most often begins with an upper respiratory tract infection and lasts from 3 to 8 weeks; most often it is so-called post-infectious, or serves as a manifestation of bacterial rhinosinusitis or asthma [3].
Chronic cough.
A common cause of chronic cough is smoking, which has a direct irritant effect on the cough receptors of the respiratory tract, and also causes irritation and an inflammatory reaction in the mucous membrane of the tracheobronchial tree. Other causes of chronic cough are:
1. Syndrome of postnasal drip of mucus into the throat due to rhinitis or sinusitis. The term “postnasal drip syndrome” (PNS) refers to clinical situations characterized by an inflammatory process in the upper respiratory tract (nasopharynx, nose, paranasal sinuses (NS)), in which discharge from the nose flows down the back wall of the pharynx into the tracheobronchial tree.
2. A special variant of bronchial asthma, which is manifested by coughing without suffocation, often at night. The so-called “cough bronchial asthma” accounts for 20-28% of all cases of chronic cough.
3. Gastroesophageal reflux (gastroesophageal reflux disease). It is believed that in more than 20% of patients with chronic cough, the cause of the latter is gastroesophageal reflux.
4. Cough often becomes a side effect when taking angiotensin-converting enzyme (ACE) inhibitors in the treatment of patients with arterial hypertension and circulatory failure. This is due to the accumulation of bradykinin, which adversely affects the bronchi. It is noted that not all ACE inhibitors have this side effect equally. Cough occurs much less frequently when using pyrindopril (Prestarium) and monopril [1].
In most cases, the occurrence of cough is associated with pathology of the respiratory system. However, there are types of it in which there is no pathology in the respiratory tract. It's reflexive
and
neurogenic
cough.
When treating cough, it is necessary to take into account its etiology, course and nature.
The most effective is etiotropic therapy, which involves either eliminating the cause of the cough or eliminating the pathological process that led to the cough. In cases where etiological and pathogenetic therapy for one reason or another is impossible or not effective enough, symptomatic therapy of cough is carried out. The choice of medications depends primarily on the nature of the cough, its intensity and other characteristics.
Today, in the pharmaceutical reference book you can find several dozen drugs that have an antitussive effect, among which traditionally there are antitussives of central and peripheral action, drugs with an indirect antitussive effect (bronchodilators, anti-inflammatory, antiallergic, decongestants, etc.), as well as combined drugs.
Such an abundance of proposed remedies for the treatment of cough is due, on the one hand, to the need to solve various therapeutic problems depending on the nature of the cough, the stage of the infectious process and the combination of certain pathological factors underlying it, and on the other hand, the insufficient effectiveness of the therapy. According to the literature, 36% of patients consider the cough medications they take to be useless; 57% note a slight therapeutic effect and only 7% report an improvement in their condition when taking the medication [4].
In the current situation, the emergence of an innovative combination drug rengalin with a fundamentally different mechanism of action opens up new opportunities for optimizing cough therapy. It belongs to the group of release-active drugs, has a complex antitussive, anti-inflammatory, bronchodilator effect and is effective against both dry and wet cough [5].
Rengalin is developed on the basis of release-active antibodies (RA-AT) to bradykinin, histamine and morphine. Due to its composition, rengalin modifies the activity of interaction with B1 and B2 receptors (bradykinin receptors), with H1 histamine and opiate receptors. The drug affects the central and peripheral parts of the cough reflex, regulating the activity of the cough center through opioid receptors (in particular, μ-receptors), exerting an inhibitory effect on the pain center and peripheral pain impulses, providing an analgesic effect. Release-active antibodies to bradykinin in the composition of rengalin influence the inflammatory process and the formation of the cough reflex by suppressing the synthesis and release of bradykinin, relaxing the smooth muscles of the respiratory system, and release-active antibodies to histamine affect the histamine-dependent activation of H-receptors and reduce vascular permeability , hyperproduction of mucus and reduce swelling of the mucous membrane [6-9].
Due to its effect on different parts of the cough reflex, rengalin has a complex anti-inflammatory, bronchodilator, decongestant and analgesic effect, flexibly regulates the activity of the cough center, controls inflammation in the respiratory tract and helps to stop or “optimize” cough depending on its nature and stage of the infectious process.
It should be noted that in the presence of codeine-like action, rengalin does not have the risk of developing side effects characteristic of centrally acting antitussive drugs: it does not cause respiratory depression, drug dependence, and does not have narcotic or hypnotic effects [10].
The therapeutic effect of rengalin is manifested in the effective relief of daytime and nighttime cough. A progressive decrease in cough intensity begins with the first use of rengalin and continues throughout the entire period of therapy. The antitussive activity of rengalin is comparable to the effectiveness of the combination drug Codelac [11].
As already mentioned, there are many causes of chronic cough, one of them is the PNS. PNS is a clinical situation when an inflammatory and/or allergic process in the upper respiratory tract (nasopharynx, nasal cavity, SNP) is accompanied by drainage of secretions along the back wall of the pharynx into the tracheobronchial tree. There is a distinction between primary, or idiopathic PNS, when the cause of the syndrome is not established, and secondary, caused by the presence of any pathology in the patient's nasal cavity, SNP and nasopharynx.
Patients complain of a feeling of “draining down the throat,” the need for frequent coughing, and accumulation of mucus in the nasal cavity. And although the cough is dry in nature, due to the coughing up of nasal mucus that has flowed into the respiratory tract, in the complaints of patients it looks like a productive one. Awareness of doctors regarding this syndrome is important, since cough in this condition is not always interpreted correctly and is mistakenly attributed to chronic bronchitis.
The standard treatment regimen for PNS includes three main points:
— therapy of identified diseases of the nasal cavity, acute respiratory tract and nasopharynx (rhinosinusitis, allergic rhinitis, etc.);
— surgical elimination of the anatomical prerequisites for the syndrome (septoplasty, adenotomy, resection of nasopharyngeal cyst, etc.);
- exclusion of possible etiological factors or their compensation (smoking, alcohol abuse, stress, occupational hazards, diseases of the gastrointestinal tract, diseases of the lower respiratory tract, etc.).
According to standards, the management regimen for patients with this syndrome includes irrigation of the nasal cavity with an isotonic solution of sea water in the form of a nasal aerosol up to 6 times a day and intranasal glucocorticosteroids in combination with antihistamines for at least 2 weeks, followed by assessment of the effectiveness of therapy. Unfortunately, treatment of these patients does not always lead to a positive result.
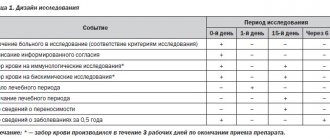
We conducted a comparative assessment of the effectiveness of the drug rengalin in the treatment of cough caused by postnasal drip in adults. The study included outpatients over 18 years of age with clinically confirmed postnasal drip syndrome that did not require surgical intervention on the ENT organs, as well as with nonproductive cough as a clinical manifestation of PNS, with a duration of at least 12 weeks (see table). 2 clinical groups of 32 patients were formed.
Distribution of patients by gender and age
The duration of cough ranged from 12 to 18 weeks. Most patients suffered from 13 to 15 weeks.
The study consisted of visit 0 - day of inclusion in the study, examination, treatment; then observation and assessment of the effectiveness of treatment: 1st visit - 5th day, 2nd visit - 10th day, 3rd visit - 15th day, 4th visit - 21st day, 5th visit - 28th day.
Treatment in the main group included irrigation of the nasal cavity with isotonic solution up to 6 times a day, the use of topical corticosteroids 400 mg 2 times a day - day 21, rengalin 1 tablet 3 times a day for 14 days. In the control group, the same regimen plus an antihistamine, 1 tablet per day for 14 days, but without rengalin.
Considering that cough is largely a subjective symptom, effectiveness was assessed using diagnostic tests: a scale for assessing daytime and nighttime cough, and a visual analogue scale for quality of life (VAS).
Daytime cough was scored from 0 to 5: 0 - no cough, 1 - single cough impulses, 2 - rare cough during the day, 3 - frequent cough that does not affect daily activity, 4 - frequent cough that reduces daily activity, 5 - severe cough, which makes daytime activity impossible.
Night cough was also assessed using a 5-point system: 0 - no cough, 1 - cough that does not interrupt sleep, 2 - cough that interrupts sleep no more than 2 times, 3 - cough that interrupts sleep more than 2 times, 4 - frequent interruption of sleep, 5 - cough that prevents you from falling asleep.
Patients also independently assessed their quality of life from 0 points (no cough) to 10 points (very severe cough).
Against the background of the treatment, positive dynamics were noted in both groups, however, in the main group it was more pronounced in relation to daytime cough already by the 1st visit ( p
<0.05) and was maintained at subsequent visits (Fig. 1).
Rice.
1. Comparative dynamics of the severity of daytime cough (scores), significance of differences at *p<0.05. Also, significant differences in the reduction of night cough between groups were recorded at the 1st visit and decreased at subsequent visits. In the main group, the effect occurred earlier, by day 5 (Fig. 2).
Rice. 2. Comparative dynamics of the severity of night cough (scores), significance of differences at *p<0.05.
Significant differences in the well-being of patients according to VAS between groups were recorded at the 1st visit and persisted at subsequent visits (Fig. 3).
Rice. 3. Comparative assessment of patients’ well-being according to VAS (scores), significance of differences at *p<0.05.
At the end of the study, complete relief of cough was noted in 89% of patients in the main group, and in 81% in the control group.
Thus, the use of rengalin in complex therapy of patients with postnasal drip has a pronounced clinical effect already by the 5th day from the start of treatment, reduces the number of episodes of daytime and night cough and its intensity, and also improves the quality of life of patients with chronic cough from the first days from start of treatment.
An analysis of the above studies demonstrated that rengalin makes cough therapy convenient for both the doctor and the patient. The drug flexibly regulates the activity of the cough center, controls inflammation in the respiratory tract and has a complex anti-inflammatory, bronchodilator, decongestant and analgesic effect. The combined effect of its components on various pathogenetic mechanisms of cough syndrome is effective in the treatment of both dry and wet cough, which, combined with high safety, allows us to recommend it for wide use in clinical practice.
Conflict of interest: The authors of the article have confirmed that they have no financial support/conflict of interest to report.
Instructions for use of Stoptussin (Method and dosage)
The tablets are taken orally and washed down with water without chewing. The dosage depends on the patient's weight. If weight is less than 50 kg, then half a tablet. A whole tablet if the weight is from 50 to 70 kg and 1.5 tablets if the weight is more than 70 kg.
How to take Stoptussin drops? To do this, you need to dissolve the drops in one hundred milliliters of liquid. The dosage depends on the patient's weight. If you weigh less than 7 kg, 8 drops are enough. If the weight is more than 70 kg, then you need to dissolve 40 drops in one hundred milliliters of liquid.
The instructions for Stoptussin-Fito are very simple. For children, half a tablespoon of syrup. If an adult, then a whole tablespoon of syrup.
Analogs
Level 4 ATX code matches:
Cashnol
Anise oil
Bronchophyte
Pine buds
Pertussin
Bronchosan
Gedelix
Mixture for inhalation
Herbion ivy syrup
Herbion plantain syrup
Herbion primrose syrup
Mukaltin
Sinupret Forte
Dr. Theiss syrup with plantain
Bronchosept
Joset
Thermopsol
Tussamag
Marshmallow syrup
Dry cough syrup
An analogue of Stoptussin is the drug Stresam , which contains the same substances. However, the price of this drug is 3-4 times higher than the price of Stoptussin, which makes medicine from the Czech Republic more preferable.
Reviews for Stoptussin
The summary of the drug is that if we talk about reviews of the tablets, they are very positive, and everyone recommends them. Moreover, many even prefer them to drops. Regarding how many days you can take Stoptussin, many talked about the immediate effect and that after a few days of using the medicine, the cough had already gone away completely.
If we talk about reviews of Stoptussin-Fito, they are not clear-cut. Of course, many users have stated that the medicine is excellent for children and has a very good expectorant effect. But there were also those who stated that the syrup had no effect.
Newspaper “News of Medicine and Pharmacy” 4 (402) 2012
Cough is not an independent disease, but a clinical symptom. Cough accompanies more than 100 different diseases; it can be a painful ailment, and therefore a serious problem not only for the patient, but also for the doctor.
Cough is a reflex reaction of the body, caused by irritation mainly of the mucous membrane of the respiratory tract and accompanied by involuntary forced respiratory movements. There is ongoing debate around the world about the most acceptable clinical definition of cough. In the British Thoracic Society guidelines for the management of adult cough, the working group adopted the following definition: cough is a forced expiratory maneuver, usually with the vocal cords closed, that is accompanied by a characteristic sound (AH Morice et al., 2007). The physiological significance of cough is to cleanse the respiratory tract from substances that have entered them from the outside (smoke, dust, various microorganisms, foreign bodies, etc.) and from endogenous components (particles of bronchial epithelium, mucus, etc.). Normally, due to the peristaltic movements of the small bronchi and the activity of the ciliated epithelium of the large bronchi and trachea, from 10 to 100 ml of secretion are evacuated along the tracheobronchial tree (Yu.M. Mostovoy, A.V. Demchuk, 2005). An increase in the viscosity of the secretion reduces the mobility of the cilia of the bronchial mucosa and causes a violation of their cleansing drainage function. The movement of secretions along the bronchial tree slows down, sometimes stopping altogether. The mucus plugs that form in this case, blocking the lumen of the distal bronchi, cause the development of obstructive syndrome. If the patient has bronchospasm, then obstruction occurs easier and faster and is much more severe.
Cough is classified according to a number of signs and causes of its occurrence (by nature, intensity, duration, course, etc.) (Yu.M. Mostovoy, A.V. Demchuk, 2005).
The diagnostic search for a patient with a cough depends primarily on whether the cough occurs acutely or exists for a long time and how treatable it is (RS Irwin, 2010). In cases of acute respiratory infection affecting both the upper and lower respiratory tract, especially during epidemics, the cause of the cough is usually not in doubt. If necessary, the diagnosis is clarified by consultation with an ENT doctor and confirmed by the effectiveness of the therapy or X-ray studies performed (M.A. Ryabova, 2010).
Acute cough is the most common symptom in primary care physician practice and is most often associated with viral infections of the upper respiratory tract. In the absence of significant concomitant pathology, acute cough, as a rule, has a benign course and resolves spontaneously. In the UK, the cost of acute cough is at least £979 million, of which £875 million is lost due to lost productivity and £104 million is spent on medical care and over-the-counter medicines. It has been established that in the United States, due to the common cold (excluding influenza-like respiratory tract infections), 25,000 million USD are lost, of which 16,600 million are lost due to decreased labor productivity, 8,000 million due to absenteeism and 230 million due to absence from work due to the need to care for the sick (A.H. Maurice et al., 2007).
Clinically significant upper respiratory tract infections (URTIs) occur with a frequency of 2–5 episodes per adult per year and 7–10 episodes per school-age child per year. If we take 2 episodes per year per adult as the minimum incidence of URTI, this equates to 120 million URTI episodes per year in the UK.
Sales of over-the-counter cough medicines in the UK amounted to £96.5 million in 2001. This figure is an underestimate because it does not take into account sales outside the pharmacy chain. With cough medicines costing an average of £3–4 per pack in the UK, this equates to at least 24 million episodes per year.
As a rule, difficulties arise when recognizing a chronic, especially uncorrectable cough. In patients with an unclear cause of cough, a thorough analysis of its features is necessary, which sometimes helps to establish its etiology. In many cases, the cause of cough can be determined by studying anamnesis, laboratory and instrumental studies.
Chronic cough has a variety of effects on your overall health. Assessing general health status is a necessary part of the evaluation of a patient with chronic cough, both in clinical practice and in research.
The Leicester Cough Questionnaire is a well-validated cough-specific quality of life questionnaire that can be used to assess the long-term impact of chronic cough.
Observational studies have shown a significant predominance of women among patients with chronic cough. In women with a cough, the sensitivity of the cough reflex is increased. Smoking is one of the most common causes of persistent cough, which appears to be dose-dependent. Patients often note that the nature of their cough changes after quitting smoking. The prevalence of chronic cough is higher in smokers (Yu.I. Feshchenko, 2009). A case-control study involving almost 2 thousand people showed a significant predominance of chronic cough in smokers. Quitting smoking leads to a short-term increase in the sensitivity of the cough reflex (A.H. Maurice et al., 2007).
According to consensus, questioning a patient with a cough should necessarily cover certain points. You can recommend that the patient fill out an anamnesis questionnaire.
To choose the right cough treatment tactics, it is important to determine its cause. The approach to cough treatment depends on the diagnosis. In cases where the cough is so intense that it significantly interferes with the quality of life, its symptomatic treatment is indicated (A.V. Babushkina, 2010). The decision to prescribe antitussive drugs should be justified by the presence of a painful cough that causes significant physical and psychological discomfort in the patient. The choice of an antitussive drug (S.A. Rachina, S.N. Kozlov, 2006) should be made individually, taking into account the mechanism of action, antitussive activity of the drug, the risk of side effects, the presence of concomitant pathologies, and possible contraindications. Indications for the use of antitussive drugs are clinical conditions in which there is an obsessive, debilitating cough, leading to disturbances in sleep, appetite, and sometimes even vomiting (painful, debilitating cough) (A.V. Volkov, 2009). Consequently, the rational choice of antitussive therapy is always based on a good knowledge of the mechanisms of action of drugs (A. Belov, 2009).
Since cough is a reflex (N.V. Shartanova, 2009), then, like any reflex, it has a reflex arc: a receptor link, a cough center, nerve fibers that transmit information, and an executive link - the respiratory muscles. Cough is suppressed most effectively at two levels - the receptor level and at the level of the cough center. In this regard, antitussive drugs are divided into two groups - central and peripheral action. In cases of non-productive cough, the use of cough suppressant medications is indicated. In mild cases of dry cough, resorption of special lozenges and infusions of antitussive herbs, as well as acupressure, are effective. For severe non-productive cough, especially painful (in cancer patients, with pleural pathology, at the onset of influenza), antitussive drugs are used. According to the mechanism of action, they are divided into drugs of central narcotic and non-narcotic action, causing inhibition of the cough center, and peripheral action, reducing the sensitivity of cough receptors (local anesthetics, drugs of combined action and drugs that suppress the release of neuropeptides by inhibiting the conduction of nerve impulses along C-fibers). The most well-known narcotic antitussive drug is codeine (I.G. Bereznyakov, 2007). Its use, like other medications in this group, is sharply limited by addiction to them. Currently, they are prescribed mainly to cancer patients. Clearly, for the treatment of cough resulting from inflammatory diseases of the respiratory tract in adult patients and especially in pediatric patients, the most safe and effective antitussive drug should be prescribed.
An example of such a combination of safety and effectiveness is Stoptussin (manufactured by Teva), a combined antitussive and expectorant drug whose active components are butamirate citrate and guaifenesin.
Butamirate citrate is a peripherally acting antitussive substance and has a peripheral, local anesthetic effect on lung receptors, which provides an antitussive effect. Unlike opioid antitussives, it does not cause central nervous system inhibition, does not depress respiration, does not cause dependence, and also has moderate bronchodilator properties. Stoptussin is approved for use in children starting from 6 months of age. The drug does not interfere with intestinal motility, so it can be recommended for digestive problems.
Butamirate citrate is quickly and completely absorbed. 98% of it is bound by plasma proteins. Metabolized to form two main metabolites (2-phenylbutyric acid and diethylaminoethoxyethanol), which also have an antitussive effect. 90% of metabolites are excreted by the kidneys and only a small part is excreted in the feces. The biological half-life of the drug is 6 hours.
It is also suitable for patients prone to caries and patients with diabetes mellitus, since butamirate citrate does not contain glucose or sugar. There are a number of advantages of butamirate citrate over other similar agents:
— high efficiency: suppresses persistent cough, even with whooping cough, improves and facilitates breathing;
- excellent tolerability: much better tolerated than codeine-containing drugs, does not have the disadvantages of codeine;
— the antitussive effect of butamirate citrate begins after 30 minutes and lasts for 6 hours.
Guaifenesin in its action occupies an intermediate position between expectorants and mucolytic drugs. Reduces the surface tension and adhesive properties of sputum, which reduces its viscosity and facilitates evacuation from the respiratory tract. Since guaifenesin has an anxiolytic (anti-anxiety) effect, its use is most justified for painful paroxysmal coughs. After oral administration, it is quickly and easily absorbed from the gastrointestinal tract. A small amount of the drug binds to blood plasma proteins. It is excreted by the kidneys, mainly in the form of metabolites, a small amount is unchanged. The biological half-life is 1 hour.
Despite the different mechanisms of action of the above substances and apparent incompatibility, Teva managed to combine them and create an effective drug. The drug is available in several forms: Stoptussin tablets - for adults and children from 12 years of age, Stoptussin drops - for adults and children from 6 months, Stoptussin syrup - for adults and children from 3 years of age (all forms contain butamirate and guaifenesin) and Stoptussin Phyto (contains liquid extracts of thyme (Thymi herba), creeping thyme (Serpylli) and plantain (Plantaginis)), which can be recommended for adults and children from 1 year.
The high effectiveness of the drug Stoptussin was confirmed in extensive multicenter clinical studies, one of which was conducted in 1985 involving 4326 patients with ARVI, pneumonia and exacerbation of chronic respiratory diseases. A reduction in cough intensity and frequency was achieved in 94.7%.
During 2001–2002 Two multicenter, open-label, randomized, parallel-group studies were conducted. During these studies, the effectiveness of Stoptussin was determined in patients of different age groups with obsessive, debilitating cough (Fig. 4, 5).
Both studies assessed three outcomes: reduction in cough frequency, reduction in cough intensity, and improvement in sputum production. According to the research results, Stoptussin demonstrated high efficiency simultaneously in all three assessed indicators, thereby proving the complexity and effectiveness of its action against obsessive cough. The safety of Stoptussin was also assessed, which in both studies was more than 95%.
Another form of Stoptussin - Phyto syrup - contains liquid extracts of thyme (Thymi herba), creeping thyme (Serpylli) and plantain (Plantaginis) and can be used in the treatment of adults and children from one year of age. The drug has a mucolytic, secretomotor, antitussive and anti-inflammatory effect, acting on the surface of the mucous membranes of the respiratory tract, reducing the viscosity of sputum, thereby separating it from the walls of the mucous membrane and modulating cough.
The effectiveness of the use of Stoptussin Phyto syrup in the treatment of acute respiratory infections and acute respiratory viral infections was demonstrated in an open controlled study in laboratory and outpatient conditions in children aged 1.5 to 15 years (n = 52) (T.L. Kiseleva, T.A. Mironenko, T.V. Urzhumova, G.S. Kozina, O.A. Afanasyeva, Institute of Traditional Medicine and Homeopathy, Ministry of Health of the Russian Federation, 2001). Based on the results of the study, it was concluded that Stoptussin Phyto syrup is effective for dry coughs and coughs with sputum and can reduce the duration of the disease by an average of 30%.
The experience of combined use of the drugs Stoptussin Phyto and Stoptussin drops in children with ARVI is interesting. At the same time, Stoptussin Phyto was prescribed 3 times a day in an age-appropriate dosage and Stoptussin drops - in an appropriate age-specific dosage at night for 12 days (Yu.M. Mostovoy, A.V. Demchuk, 2005).
Thus, Stoptussin effectively achieves two treatment goals: it reduces the frequency and intensity of cough - it removes “extra” or “empty” cough shocks (which do not contribute to the evacuation of sputum, but only interfere with the patient) and improves the discharge of sputum.
In all studies, Stoptussin was prescribed to patients at the very beginning of the disease, when the cough was extremely dry and debilitating.
In rare cases (about 4%), patients may experience side effects - dyspeptic disorders (nausea, vomiting, diarrhea, stomach pain), dizziness, headache, drowsiness, urticaria and skin rash, which indicates the safety of the drug.
conclusions
1. Stoptussin is most effective for obsessive, debilitating cough.
2. The best effect is achieved in the initial stages of acute respiratory infections and acute respiratory viral infections.
3. By reducing the frequency and intensity of cough impulses, it does not inhibit the process of formation and discharge of sputum.
4. Has an equivalent effect in equivalent doses in different forms of release.
5. Stoptussin in the form of drops can be used in the treatment of children from 6 months of age.
6. Relieves the feeling of fear during prolonged paroxysmal cough due to the anti-anxiety effect of one of the components of the drug.
7. Has a minimal frequency of side effects and reactions.
8. The use of Stoptussin in the complex therapy of diseases of the respiratory system, accompanied by an obsessive cough, can help improve the effectiveness and safety of therapy for the underlying disease.
Stoptussin price, where to buy
The price of tablets is around 110-140 rubles for one pack of 20 tablets.
If we talk about syrup, the price for Stoptussin-Fito is 166 rubles.
Stoptussin cough drops have the best effect for children. The price for them varies from 72 rubles to 212, depending on the volume of the medicine.
- Online pharmacies in RussiaRussia
- Online pharmacies in UkraineUkraine
- Online pharmacies in KazakhstanKazakhstan
ZdravCity
- Ambrobene stoptussin cap.
for oral administration 10 mlTeva Pharmaceutical 151 rub.order - Ambrobene stoptussin drops for oral administration 4 mg + 100 mg/ml fl. with cap. 50mlTeva Pharm. enterprises s.r.o.
RUB 365 order
Pharmacy Dialogue
- Ambrobene STOPTUSSIN (tab. 4 mg + 100 mg No. 20) Teva Operations
RUB 262 order
- Ambrobene STOPTUSSIN (bottle 10ml)Teva Czech Industries SRO
147 RUR order
- Ambrobene STOPTUSSIN (drops d.pr. orally 4mg+100mg/ml 50ml) Teva Czech Enterprises s.r.o.
RUB 377 order
- Ambrobene STOPTUSSIN (25ml bottle) Teva LLC
RUB 253 order
- Ambrobene STOPTUSSIN (bottle 25ml)Teva Czech Industries SRO
280 rub. order
show more
Pharmacy24
- Stoptussin Phyto 100 ml syrup TEVA Czech Industries s.r.o., Czech Republic
107 UAH.order - Stoptussin No. 20 tablets TEVA Czech Industries s.r.o., Czech Republic/TOV Teva Operations Poland, Poland
66 UAH order
- Stoptussin 100 ml syrup TEVA Czech Industries s.r.o., Czech Republic
121 UAH order
PaniPharmacy
- Stoptussin phyto liquid Stoptussin phyto syrup 100ml, Teva Czech Industries
127 UAH order
- Stoptussin liquid Stoptussin drops 10ml, Teva Czech Industries
89 UAH order
- Stoptussin liquid Stoptussin syrup 100ml, IVAX Pharmaceuticals
158 UAH order
- Stoptussin tablets Stoptussin tablets. No. 20, Teva Czech Industries
79 UAH order
- Stoptussin liquid Stoptussin drops 25ml, Teva Czech Industries
148 UAH order
show more
STOPTUSSIN (drops)
t and other forms of release in 10 ml and 50 ml, respectively, the price if you purchase a different volume will differ significantly.
I almost always buy the medium size, it is enough for a course of use and it is not as expensive as in large quantities. The bottle in which the medicine is packaged is made of dark glass. Stoptussin cough drops themselves are colorless and look like plain water. The bottle with the medicine is equipped with a dispenser to collect the required number of drops, because it is in them that the dose for administration is measured. The number of drops depends on the weight; it is better to read the details in the attached instructions. There is also a lot of useful information, it is better to read it before taking the medicine, because there are contraindications for taking it and possible side effects.
The medicine is serious, it contains alcohol, so it can affect activities that require increased attention and this fact must be taken into account. My daughter started taking the cough medicine Stoptussin at the age of three, when she had a severe allergic cough that got worse at night. Many medications did not save me from an obsessive dry cough, but this medicine became a salvation. The improvement became noticeable immediately after the first dose; after about 20 minutes, the coughing attacks began to stop. When taking Stoptussin drops, you need to drink a lot for the effect to be stronger, but most importantly, the effect is there and it is very noticeable. This medicine should be used while the cough is dry; when sputum begins to cough up, you need to look for another suitable remedy; Stoptussin is not suitable in this case.
With all its advantages, the drug Stoptussin has a significant drawback - it contains alcohol, which is why the drug has a bitter taste and a specific smell. Not every child will calmly take such a medicine; many will simply refuse it when they try it. It’s good that the drops can be added to any drink, tea, compote, etc., but the taste of the medicine is still noticeable even in sweet drinks, only less pronounced. That is, the drug has a good effect in helping to relieve an irritating cough, but it is not suitable for everyone due to its composition and taste.
I will recommend it, since it really helped us in different situations and did not cause any negative reactions, but it is better after the recommendation of a doctor in order to avoid negative effects and other unpleasant consequences from taking it.
Thank you all for your attention to my review!